An NSQIP survey of outcomes after resection of choledochal cysts in adults
2022-01-07JosephBrungardtClayKingKurtSchropp
Joseph G. Brungardt , Clay D. King, Kurt P. Schropp
Department of Surgery, The University of Kansas, 40 0 0 Cambridge, M/S 2005, Kansas City, KS 66160, USA
TotheEditor:
Choledochal cysts, now generally termed biliary cysts to include intrahepatic cysts, are a rare lesion with unknown incidence [1] .These cysts more often affect females than males (4:1) [2] . Often associated with the pediatric population of congenital etiology,some series have found adults equally affected [3] . Classification of biliary cysts follows the Todani classification with six groups [4] .This has allowed physicians to consider treatment according to their type. While treatment typically consists of excision with Roux-en-Y reconstruction, data on the subject is limited to case series or single-institution cohorts. Other treatment modalities include sphincterotomy (endoscopic more commonly than open) in the case of type III cysts, and a liver transplant for patients with type V cysts, which were not captured in this study. Without treatment, patients risk poor biliary drainage, leading to hepatic fibrosis, or neoplastic transformation [5] . The low incidence of biliary cysts creates difficulty in their study. A recent multi-institutional study included 135 children and 259 adults, with adult rate of overall complication 35%, readmission rate of 1.4%, and 30-day mortality of 6.9%, which is representative of other studies [6] . Few studies have been done within larger databases to evaluate shortterm clinical outcomes after surgery for biliary cysts. We sought to determine morbidity and mortality in patients undergoing surgical treatment of biliary and choledochal cysts within a nationally recognized database.
Data used was from the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP), years 2015 to 2018 [7] . This database contains patient-level, aggregate data,and is Health Insurance Portability and Accountability Act (HIPAA)-compliant as it does not identify hospitals, physicians, or patients.The Institutional Review Board of the University of Kansas approved this study.
The study included all patients 18 years of age and older with a postoperative diagnosis of choledochal cyst, according to the International Classification of Diseases (ICD) 9th and 10th editions.These codes were 751.69 or Q44.4. Patients were then stratified into two groups, those who underwent reconstruction (non-Roux Loop) and those who underwent excision with Roux-en-Y reconstruction by current procedural terminology coding. The database could not provide method of diagnosis or exam, type of cyst, exact method of reconstruction, or technical details of surgery. As no liver transplants were coded, we assumed all procedures were some form of biliary tract resection. If coding noted a Roux-en-Y,then it was grouped as such; but if no such coding existed, it was assumed to be a non-Roux Loop reconstruction. The age, sex, race,comorbidities, perioperative variables, elective operation, wound classification, admission quarter, mortality, operative time, length of hospital stay, discharge destination, and postoperative outcomes such as readmission and return to the operating room, as well as complications such as deep vein thrombosis or wound infection,were included in the analysis as available in NSQIP up to 30 days.Data on each patient is not collected after the 30-day period.
Baseline characteristics were compared by the Chi-square test or Wilcoxon test, using Fisher’s exact test where necessary. Postoperative outcomes were analyzed utilizing the same tests. Multivariable regression modeling was not carried out due to the small sample size and homogeneity between preoperative variables. Statistical analysis and data management were performed using SPSS(IBM Corp. IBM SPSS Statistics for Windows, version 23.0. Armonk,NY, USA) and Excel (from Microsoft version 16.32). APvalue<0.05 was considered statistically significant.
A total of 240 patients were captured by the NSQIP database from 2010 to 2015 ( Table 1 ). The median age was 47 years,with no difference in age between the two study groups. 85.42%of the population was female. The majority of patients were white (62.50%), with no differences between the groups. Comorbidities were clinically and statistically similar between the two groups, with 99.17% of the population being functionally independent. 19.58% of the population were current smokers. 89.58%of operations were classified as elective. There appeared to be an comparable distribution of admissions by quarter, with no differences between the two groups. Wound classification was clean/contaminated in 82.08% of the population. As there is no way to perform a “clean” case during biliary surgery, these 8 cases(3.33%) may have been coded incorrectly.
The median length of hospital stay was 5 days ( Table 2 ). Median operative time was 238.0 min. There were no statistical differences in length of hospital stay and operative time between the two groups. The 30-day mortality was 1.25%, and discharge to home occurred in 96.25% of the population. Readmission forthe entire population was 11.67%, with 27 readmissions (11.25%)related to the operation. Ten patients (4.17%) returned to the operating room, all of which were related to the operation. Return to the operating room occurred for a postoperative diagnosis of:ileus (1), hypertrophic pyloric stenosis (1), intraabdominal injury(1), post-procedureal complications (1), post-procedureal hemorrhage (1), obstruction of bile duct (1), and peritoneal abscess (1).Organ space surgical site infection was statistically different between groups, with 15 patients being affected in the excision group(15.00%) and 5 (3.57%) affected in the reconstruction group (P<0.01).
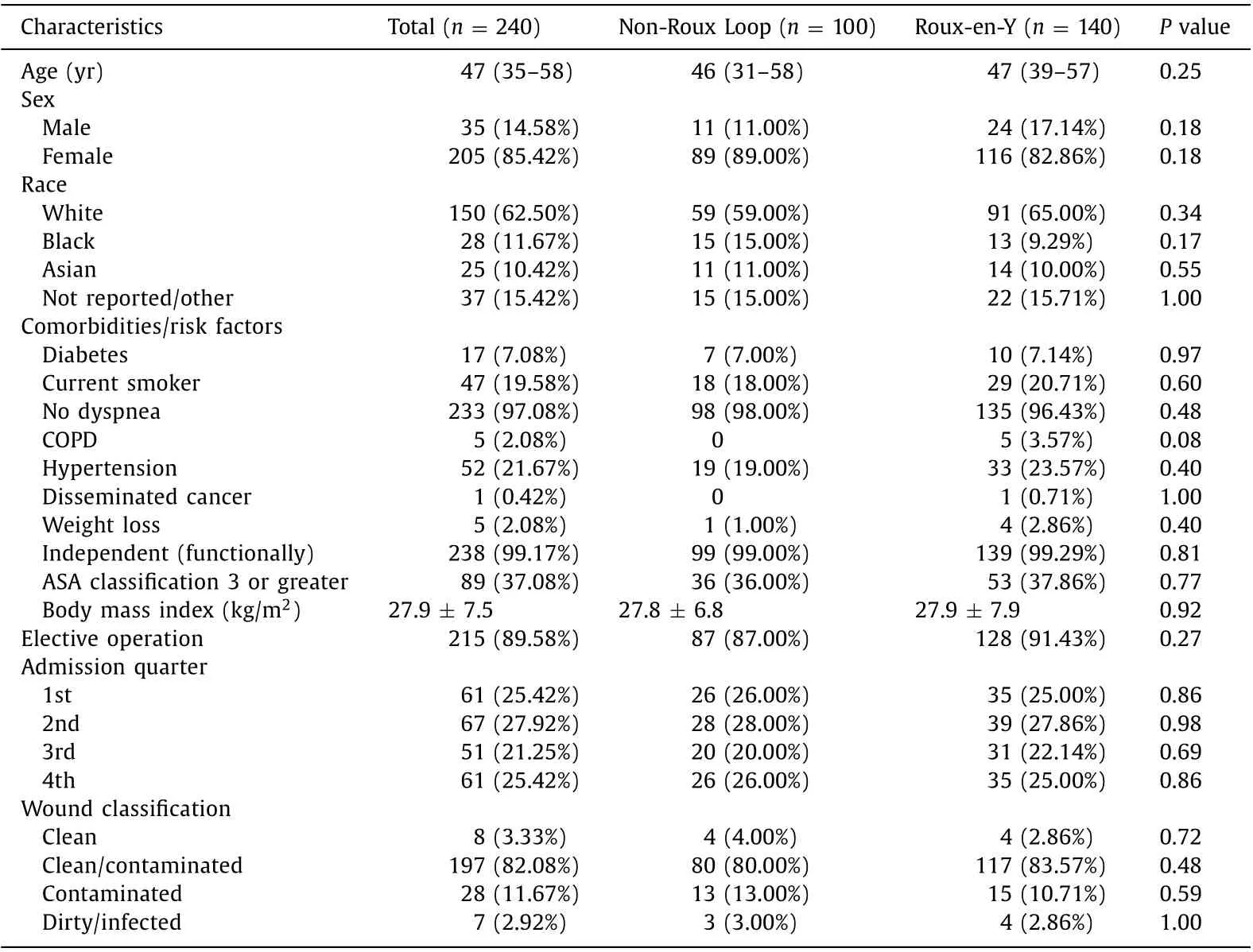
Table 1 Baseline demographics, comorbidities and risk factors of adults with choledochal cysts.

Table 2 Perioperative outcomes of adults with choledochal cysts.
This analysis describes a large national cohort of patients undergoing surgical treatment of choledochal cysts. Furthermore, it describes that outcomes after treatment, with or without Roux-en-Y reconstruction, may have similar immediate clinical outcomes.Patients undergoing excision without a Roux-en-Y (i.e. a non-Roux Loop) may experience higher rates of organ space surgical site infection, which may have been coded as such in patients who experience bile leaks. This analysis should support the surgeon counseling patients on outcomes of surgery with more granular, large scale population data of short-term outcomes. Also, this analysis contributes to the growing body of literature on adults with pathologies classically associated with children, who may require surgical intervention. The data at a minimum provides estimates of immediate postoperative outcomes of patients with choledochal cysts.
This study may represent the largest national analysis of adult patients undergoing excision of choledochal cysts. While we were able to stratify our population into two groups of patients who underwent excision of cysts with and without complex Roux-en-Y reconstruction, further relevant detail is lacking. The strength of this study lies in the ability to obtain outcomes such as length of hospital stay, mortality, and readmission as well as rare complications such as deep vein thrombosis, reintubation, and sepsis up to 30 days. Not captured within the NSQIP database are repeated operations, prior surgery, lesion type, oncologic diagnoses, and longterm outcomes such as stricture or recurrent cholangitis. A recent national cohort in the Netherlands by de Kleine et al. describes incidence of types of cysts, outcomes, though mortality is noted to be 2% compared to 0.6% in this study [8] . A large recent series in children notes better short-term in hepaticoduodenostomy and comparable long-term outcomes compared to Roux-en-Y hepaticojejunostomy reconstructions [9] . Overall morbidity in some series is as high as 58%, compared to 50% overall morbidity (complication of any kind) in our study [10] . Further large series on the laparoscopic treatment of choledochal cyst in children highlight the steep learning curve to achieve outcomes seen in open treatment [11] .
Contributions to the current knowledge and treatment of choledochal cysts include estimations of short-term outcomes after surgery, as they pertain to the adult population. Prior studies have demonstrated an increased incidence of choledochal cyst disease in adults, making the study of what is often considered a pediatric pathology more pertinent [ 6 , 8 ]. This study also confirms the female predominance of disease, at a rate even higher than described previously [1] . While Soares et al. [6] described a nearly one-third readmission rate at six months, we saw a rate of readmission, which was much lower, though at one month. Furthermore, large studies of this disease in non-Asian populations are rare, making this analysis of a Western population important.
Our study’s limitations are its retrospective nature and the limitations inherent to the database. The ACS NSQIP database acknowledges several limitations inherent to their database [7] . Generic variables are collected, patients are only followed for 30 days, and some variables are not present for each case. Data are only from participating hospitals, and surgical or surgeon volume is not collected; thus, we are unable to control for this. Having these variables in such a database would allow for analysis and control for specialty volume and hospital volume. Finally, while coding captures Roux-en-Y, the final reconstructive anatomy, assumed to be hepaticoduodenostomy, is limited by this coding process.
This is a large adult cohort in a Western population which describes outcomes of patients undergoing surgical treatment for choledochal cysts. The findings suggest that immediate outcomes for resection or reconstruction are similar. However, resection without a Roux-en-Y reconstruction may portend a higher risk of organ space infection, which may be bilomas or seromas. Procedure targeted files for more complex procedures such as these could capture clinical details necessary for the study of larger populations.
Acknowledgments
None.
CRediT authorship contribution statement
Joseph G. Brungardt: Data curation, Formal analysis, Writing -original draft. Clay D. King: Methodology, Writing - original draft.Kurt P. Schropp: Conceptualization, Supervision, Writing - review& editing.
Funding
None.
Ethical approval
This study was approved by the Institutional Review Board at the University of Kansas as Human Subjects exempt.
Competing interest
The American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) and the hospitals participating in the ACS NSQIP are the source of the data used herein; they have not verified and are not responsible for the statistical validity of the data analysis or the conclusions derived by the authors. The authors declare that they have no conflict of interest.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Hepatocellular-cholangiocarcinoma with sarcomatous change:Clinicopathological features and outcomes
- Successful treatment of complete traumatic transection of the suprahepatic inferior vena cava with veno-venous and cardiopulmonary bypass with hypothermic circulatory arrest ✩
- Successful withdrawal of antiviral treatment in two HBV-related liver transplant recipients after hepatitis B vaccination with long-term follow-up
- High perioperative lactate levels and decreased lactate clearance are associated with increased incidence of posthepatectomy liver failure
- Glucagonoma syndrome with necrolytic migratory erythema as initial manifestation
- A rare type of choledochal cysts of Todani type IV-B with typical pancreaticobiliary maljunction