A rare type of choledochal cysts of Todani type IV-B with typical pancreaticobiliary maljunction
2022-01-07XuTingZhiBingRanYuZhiQiangChen
Xu-Ting Zhi , Bing-Ran Yu , Zhi-Qiang Chen
Department of Hepatobiliary Surgery, General Surgery, Qilu Hospital, Cheeloo College of Medicine, Shandong University, Jinan 250012, China
Choledochal cysts (CCs), first described by Vater and Ezler in 1723, are rare congenital cystic dilations of biliary tract [1] . The most widely adopted classification system from Todani et al. divides CCs into five major types and several subtypes [2] . Almost all of the CCs are type I and type IV-A, while type IV-B is extremely rare [ 3 , 4 ]. The accurate diagnosis and precise categorization of CCs are crucial for surgeons to perform proper operative strategy. Here,we report a typical CCs of Todani type IV-B with a typical scenario of pancreaticobiliary maljunction (PBM) in a 50-year-old male,and proper surgical treatment was conducted with uneventful recovery.
A 50-year-old male presented with intermittent abdominal pain in the right upper quadrant for the last five years with symptoms worsening and occasional slight fever in the past three months.The patient had no history of vomiting, abdominal trauma, liver cirrhosis or hepatitis. Physical examination revealed mild conjunctival icterus and epigastric tenderness without signs of peritonitis. Laboratory findings showed obstructive jaundice and pancreatitis as follows: white blood cells 6.46 × 109/L, neutrophil 82.2%,total bilirubin 72.6 mmol/L, direct bilirubin 50.2 mmol/L, aspartate aminotransferase 250 IU/L, alanine aminotransferase 137 IU/L,gamma-glutamyl transferase 1156 U/L, blood amylase 541 U/L and lipase 462 IU/L. All the other laboratory routines not mentioned above were within normal range. Preoperative magnetic resonance cholangiopancreatography (MRCP) was taken and a percutaneous transhepatic cholangial drainage (PTCD) was placed to ameliorate symptoms ( Fig. 1 A). The biliary drainage amylase level was tested to be 972 U/L. Then a further cholangiography via PTCD ( Fig. 1 B)consistent with MRCP showed multiple extrahepatic dilatations of biliary tract, and a diagnosis of congenital CCs was made and classified as Todani type IV-B (type I + type III). Moreover, there was a coexistence of PBM which is defined as pancreatic and bile ducts join outside the duodenal wall, usually forming a long common channel; in this case, it was identified as insertion of the type I cyst and pancreatic duct into the type III cyst outside duodenum. After preoperative preparations, the patient underwent surgical procedures including extrahepatic biliary duct excision of type I cyst ( Fig. 2 A), Roux-en-Y hepaticojejunostomy and transduodenal marsupialization of the type III cyst ( Fig. 2 B) with an uneventful recovery. Postoperative pathology revealed chronic inflammation and fibrosis of biliary wall as well as atrophy of glandular epithelia, and it needs to be noted that there were more nerve fiber bundles distributed in the biliary wall which is not commonly seen in normal tissues ( Fig. 3 ). The patient was followed up for 50 months after surgery with symptoms totally relieved and no complications.
CCs are rare congenital cystic dilatations of the biliary tract,with approximately 80% of cases diagnosed in childhood within the first decade of life. According to the most widely adopted classification system from Todani and colleagues, CCs are categorized into five major types and several subtypes according to the morphology and location of the cysts [2] . The specific etiology of CCs is unknown except type V (also called Caroli’s disease, which is an autosomal recessive disorder). Some theoretical etiologies include PBM and pancreatic juice regurgitation, disturbed embryonic development, and high intraluminal pressure with a narrow segment distal to the cyst [ 3 -5 ]. PBM was previously considered the major cause of CCs as it allows pancreatic juice reflux into biliary duct and causes inflammation, impairment and weakening of biliary wall, leading to subsequent dilatation [1] . However, this theory is now questioned as so many patients with PBM without CCs are discovered and animal models of PBM do not develop CCs [5] . And some clinical studies advocated that intraluminal pressure of bile duct played a more important role than pancreatic reflux in the development of cystic dilatation [ 3 , 4 ]. As shown in this case, there was a typical scenario of PBM but the level of bile amylase was not as high as that seen in classical PBM regurgitation, thus indicating PBM may not be the major etiology for this patient. While notably and intriguingly, the postoperative pathology revealed a distribution of more nerve fiber bundles in the resected type I cyst epithelia. But it is a pity that we did not take biopsy from the type III cyst during operation, so the pathology of type III cyst was missing and the role of nerve fiber bundles was not clear for this patient and it needs further investigations.
The clinical presentations vary according to different degrees of pathophysiologic changes including most commonly presented obstructive jaundice, pancreatitis, cholelithiasis and cholangitis,and the incidence of cholangiocarcinoma is reported to be much higher than that in ordinary population [ 1 , 2 ]. Different management strategies are implemented for each type and surgical resection of extrahepatic biliary duct and hepaticojejunostomy are recommended for type I and type IV-A cysts, but sometimes personalized treatment may be indicated for complicated situations such as for this case.

Fig. 1. Preoperative MRCP ( A ) and cholangiography via PTCD ( B ) showed multiple dilatations of extrahepatic biliary duct: one (type I cyst, yellow asterisk) was a fusiform dilation of common bile duct where the gallbladder joined in; another (type III cyst, black asterisk) was at the terminus of common bile duct within head of pancreas where the pancreatic duct (white arrowheads) converged outside duodenum, which made a diagnosis of PBM. The black arrowhead showed outlet of type III cyst into duodenum.MRCP: magnetic resonance cholangiopancreatography; GB: gallbladder; DU: duodenum; PTCD: percutaneous transhepatic cholangial drainage.
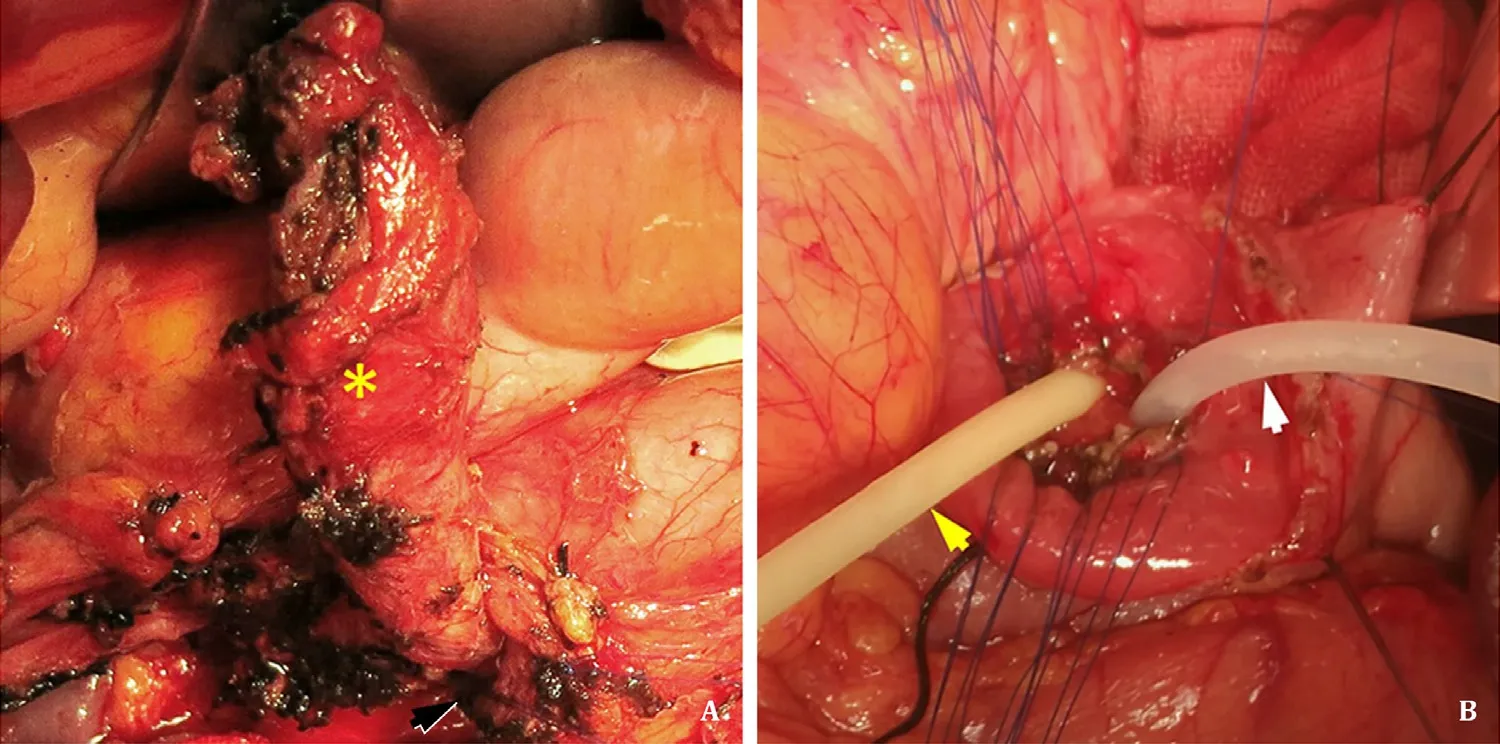
Fig. 2. Intraoperative photos showed resection of extrahepatic bile duct ( A , yellow asterisk for type I cyst and black arrow for the narrow end) and transduodenal marsupialization of the type III cyst ( B , two navigation tubes were used during operation as yellow for bile duct and white for pancreatic duct).
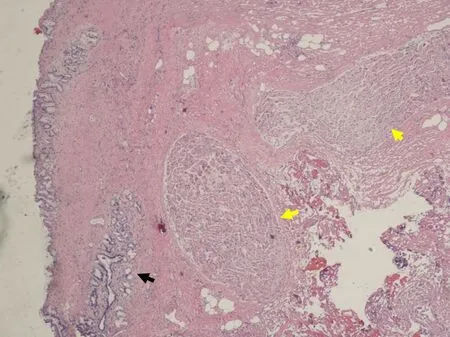
Fig. 3. Postoperative pathology revealed chronic inflammation, fibrosis of biliary wall, atrophy of glandular epithelia (black arrow) and most notably more nerve fiber bundles (yellow arrows) distributed in the tissue than in those normal biliary wall.
After exhaustive literature review, we identify only two analogous cases reported. The first case comes from original case series of Todani et al. in which they illustrated type IV-B cysts as dilated extrahepatic bile duct and choledochocele. However, the cholangiography of this type represented actual type IV-A cysts with a dilated common channel that had several protein plugs in it, but not a choledochocele [2] . Another case comes from a 10-month infant reported by Lao et al. [6] , that an unclear MRCP image showed similar cystic dilatations of extrahepatic duct as in the present case.
This study is the first time in literature that typical clear images have been illustrated for Todani type IV-B (type I + type III) CCs with classical scenario of PBM in adult patient, and proper surgeries were documented, providing some implementations for future treatment strategy and etiological investigations for this rare subtype of CCs.
Acknowledgments
None.
CRediT authorship contribution statement
Xu-Ting Zhi: Formal analysis, Writing - original draft. Bing-Ran Yu: Formal analysis, Writing - original draft. Zhi-Qiang Chen: Conceptualization, Supervision, Writing - review & editing.
Funding
None.
Ethical approval
Informed consent for publication was obtained from the reported patient.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Hepatocellular-cholangiocarcinoma with sarcomatous change:Clinicopathological features and outcomes
- Successful treatment of complete traumatic transection of the suprahepatic inferior vena cava with veno-venous and cardiopulmonary bypass with hypothermic circulatory arrest ✩
- Successful withdrawal of antiviral treatment in two HBV-related liver transplant recipients after hepatitis B vaccination with long-term follow-up
- High perioperative lactate levels and decreased lactate clearance are associated with increased incidence of posthepatectomy liver failure
- An NSQIP survey of outcomes after resection of choledochal cysts in adults
- Glucagonoma syndrome with necrolytic migratory erythema as initial manifestation