Unilateral versus bilateral Y-type stent-in-stent metal stent insertions in inoperable malignant hilar biliary strictures: A multicenter retrospective study
2022-01-07IkHyunJoChngNyolPikDeBumKimJesinLeeJongYulLeeJeHyukChngKyuHyunPikWonSukPrk
Ik Hyun Jo , Chng-Nyol Pik ,, De Bum Kim , Jesin Lee , Jong Yul Lee ,Je Hyuk Chng , Kyu-Hyun Pik , Won-Suk Prk
a Department of Internal Medicine, College of Medicine, St. Vincent’s Hospital, The Catholic University of Korea, Seoul, Korea
b Department of Internal Medicine, College of Medicine, Incheon St. Mary’s Hospital, The Catholic University of Korea, Seoul, Korea
c Department of Internal Medicine, College of Medicine, Bucheon St. Mary’s Hospital, The Catholic University of Korea, Seoul, Korea
d Department of Internal Medicine, College of Medicine, Daejeon St. Mary’s Hospital, The Catholic University of Korea, Seoul, Korea
Keywords:Cholestasis Extrahepatic neoplasm Cholangiopancreatography Endoscopy Self-expandable metal stents
ABSTRACT
Introduction
Malignant hilar biliary strictures (MHBSs) are difficult to diagnose definitively, and mostly unsuitable for surgical treatment at the point of diagnosis [1 , 2] . Endoscopic biliary drainage had advantages over percutaneous biliary drainage with shorter hospital stay and less invasiveness for patients with MHBS [3-5] . The current international consensus recommends the use of metal stents rather than plastic stents for palliative intervention, considering better survival and cost-effectiveness [6] .
An argument over the extent of biliary drainage has been ongoing. Even in the case of draining about 25%-30% of the total liver volume, there was no inferiority in survival, and the technical difficulties and complications were higher in patients with bilateral drainage; therefore, unilateral drainage was deemed sufficiently effective [7 , 8] . The necessity of bilateral decompression has also emerged, as several reports have pointed out the incomplete relief of hyperbilirubinemia or possible biliary tract infections in patients with unilateral drainage [9 , 10] . However, previous studies were mostly retrospectively designed, with small number of enrolled subjects [ 8 , 11 , 12] . A recent prospective study suggested the advantages for bilateral metal stents, but heterogenous methods as stentin-stent or side-by-side were included, without discrimination [13] .
This study aimed to compare the clinical usefulness and therapeutic outcomes of unilateral drainage and Y-type stent-in-stent bilateral drainage during endoscopic implantation of biliary selfexpandable metal stents (SEMSs) in MHBS patients.
Methods
Study design and population
A multicenter retrospective designed study was conducted in four teaching hospitals in Korea (St. Vincent’s Hospital, Incheon St. Mary’s Hospital, Bucheon St. Mary’s Hospital, and Daejeon St.Mary’s Hospital). Patients diagnosed with inoperable MHBS who underwent unilateral or Y-type stent-in-stent bilateral drainage with SEMS from January 2009 to December 2019 were included.A total of 409 patients were recruited, and those who met the following criteria were excluded from the study: age under 18 years,a history of hepatobiliary tract surgery, insufficient medical records for stent patency or survival status, mixed therapy with metal and plastic stents, Bismuth-Corlette classification type I, and incomplete laboratory data. A total of 236 subjects were included. Patients who inserted a unilateral stent due to the bilateral SEMS failure were not included in the unilateral SEMS group. The primary outcome was loss of patency after endoscopic stent placement. The secondary outcomes were success rates, procedure-related complications, and overall survival after biliary stenting.
Procedures
The patient was in a supine position and moderate sedation was performed using intravenous midazolam and meperidine. The same types of side-viewing duodenoscope (TJF-260V, Olympus Optical Co., Ltd, Tokyo, Japan) were used in all hospitals. One-sided or two-sided biliary stent insertion was decided according to the preference of the endoscopists, the patient’s medical condition, and the imaging modality results. After the selective cannulation and endoscopic sphincterotomy, a 0.035-inch-diameter guidewire was passed through the lesion, and then a through-the-scope (TTS)-type unilateral stent was moved through the working channel of the scope and mounted under fluoroscopic guidance. Bilateral stenting was executed in the following order. The first stent was inserted in the same way as the unilateral procedure. An additional guidewire was introduced into the lumen of the stent already installed and then placed into the counterpart of the lesion by penetrating through the first metal stent. After that, the second stent was finally placed by a stent-in-stent method. The bilateral stents were installed at once on the same day as possible, but it was allowed to be placed at time intervals of several days for certain reasons like the patient’s medical condition. The prophylactic antibiotics administration was started before the endoscopic retrograde cholangiopancreatography (ERCP) and maintained until successful bilirubin reduction with no sign of cholangitis confirmed after the procedure.
SEMS
Uncovered cross-wired SEMSs were from four manufacturers,Standard Sci Tech. (Seoul, Korea), Taewoong Medical (Seoul, Korea),M.I. TECH (Pyeongtaek, Korea), and S&G Biotech Inc. (Seoul, Korea).Stents were selected among four manufacturers depending on the inventories of each participating hospital or the preference of the operator, without any randomization. In the case of bilateral biliary drainage, the two inserted stents were selected from the same manufacturer. The diameter of the SEMS was 10 mm. The length of the SEMS was determined before or during the procedure, depending on the operator’s judgment.
Definitions of variables and outcomes
Age, sex, height, body weight, past medical history, and lifestyle information (smoking and alcohol consumption) of the patients were collected from the electronic medical records. All institutions conducted blood tests and checked vital signs within 24 to 48 h before endoscopic stent placement, and the data closest to the procedure were used for analysis.
In patients with MHBSs due to cholangiocarcinoma, the stage was classified according to the American Joint Commission on Cancer and the Union for International Cancer Control (AJCC/UICC) 8th edition and the Bismuth-Corlette classification [ 14 , 15] . We evaluated rates of technical and clinical success. Technical success was defined as stents installed in place by the manner originally planned and the confirmed flow of bile or contrast agent immediately after the procedure. Clinical success was defined as a decrease in total bilirubin levels of more than 50% from baseline within one week after stent drainage or 75% within four weeks [16] . Procedure-related complications as follows were investigated. Acute pancreatitis was defined by the presence of more than 2 of the 3 criteria: (1) an elevation in serum amylase and/or lipase more than three times the upper normal limit; (2) abdominal pain; (3) and/or characteristic findings from imaging consistent to acute pancreatitis [17] . Acute cholangitis was defined as fever,chilling, and elevation of inflammatory markers with cholestasis or evidence on imaging [18] . Gastrointestinal bleeding was defined as any hemorrhage signs (hematemesis, melena, or hematochezia),and/or a rapid decrease in hemoglobin levels (2 g/dL or more), or active bleeding observed by the endoscope [19] . Perforation was defined as definite perforation found during the procedure or free air shadows in the post-stent X-ray images. Patency loss events were defined as one of the following three criteria: (1) an increase in total bilirubin levels that persisted after stent insertion, (2)the performance of additional endoscopic or percutaneous biliary drainage, or (3) a stent obstruction confirmed through computed tomography (CT), magnetic resonance imaging (MRI), or ERCP.
Statistical analysis
R Studio was used for all data analyses and visualizations (ver.1.0.153, R Foundation for Statistical Computing, Vienna, Austria).Data were expressed as mean ± standard deviation (SD) or median and interquartile range (IQR) or number (percentage), as appropriate. The differences were analyzed by Student’st-test, Wilcoxon-Mann-Whitney test, Chi-square test, or Fisher’s exact test. To compare the patency loss and overall survival between the two groups,Kaplan-Meier curves were plotted, and log-rank tests with stratification were conducted to identify significant differences. A Cox proportional hazards model was used to determine the possible factors associated with either stent patency loss or overall survival,and the hazard ratio (HR) values of each factor. Statistical significance was defined asPvalues of less than 0.05.
Results
Characteristics of the study population
During the study period, a total of 236 patients underwent SEMS insertions for MHBS. The proportion of males was higher than that of females (59.3% vs. 40.7%), and the median age of the patients was 77 years (IQR: 69-83). Other demographics are shown in Table 1 .
Bilateral stenting was performed in 63 (26.7%) cases. Among them, the number of two-stage procedures was 32 (50.8% of 63 bilateral stenting). The mean time interval between the first and second stents was four days. Patients with cholangiocarcinoma weremore likely to have bilateral involvement (Bismuth-Corlette classification type IV, 52 of 140, 37.1%) and advanced disease (the AJCC/UICC stage IV, 51 of 148, 34.5%). Further data regarding disease status are presented in Table 2 .

Table 1 Baseline characteristics of the study population.
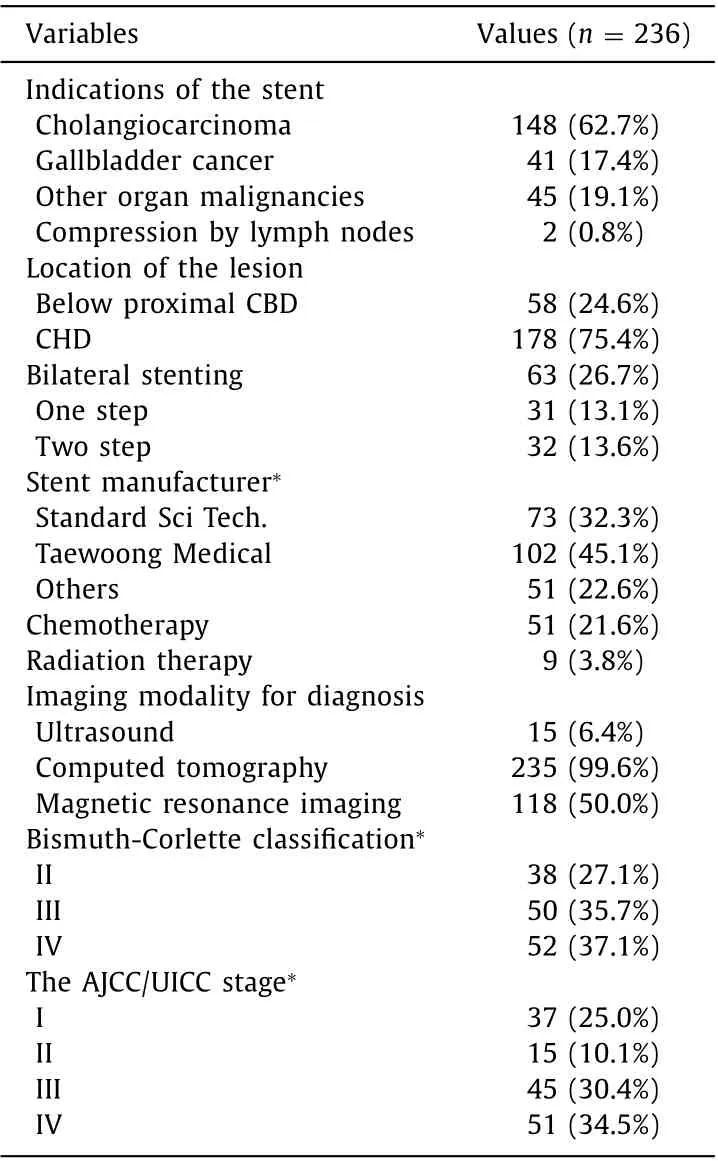
Table 2 Basic information about the disease status.
Comparison of unilateral and bilateral metal stent groups
There was no significant difference between unilateral and bilateral groups in demographics, vital signs, medical histories, and lifestyle factors except the occurrence of dyslipidemia and concomitant malignancies ( Table 3 ). Regarding the laboratory findings, higher lactate dehydrogenase (LDH), erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) levels were found in the unilateral metal stent group (P<0.05). As an indication for biliary stenting, the proportion of cholangiocarcinoma was higher in the bilateral group, whereas other diseases were more frequent in the unilateral group as presented in Table 4 . Types of Bismuth-Corlette classification were not significantly different between unilateral and bilateral groups, but more patients had advanced-stage disease (AJCC/UICC stage III and IV) in the unilateral group (74.5%vs. 48.2%,P= 0.001).
Success rate and procedure-related complications
The technical success rate was 98.8% in the unilateral group and 82.5% in the bilateral group (P<0.001). However, the clinical success rate of bilateral group was superior to that of unilateral group(85.7% vs. 70.5%,P= 0.028).
Early complications were reported in 40 patients, and late complications were reported in 13 patients. Pancreatitis was the most common early complication (28 of 236, 11.9%), and cholangitis was the most common late complication (5 of 236, 2.1%). Rates of early or late complications were not significantly different between unilateral and bilateral groups ( Table 4 ). There were no differences in the composition of early and late complications between the two stent groups, either.
Survival analysis for outcomes
During the study period, a total of 58 patients in the unilateral stent group (33.5%) and 30 in the bilateral stent group (47.6%) were confirmed with patency loss (P>0.05, Table 4 ). There was no significant difference between the two groups. The median time of stent patency was 195 (93-1134) days in the unilateral stent group and 318 (153-536) days in the bilateral stent group. There was no significant difference in the risk of patency loss according to the stent group (P= 0.80) ( Fig. 1 ). With respect to mortality, the unilateral group had a higher rate than the bilateral group (48.0% vs.33.3%), and the same tendency was also found in the log-rank test(P<0.01) ( Fig. 2 ). The median overall survival time in the two groups was 202 days and 828 days, respectively. Stratifications for the stent indication (cholangiocarcinoma vs. other indications), the Bismuth-Corlette classification, and the AJCC/UICC stage were also performed, and the overall survival were not significantly different in the entire study population.
No variables were associated with the incidence of patency loss( Fig. 3 ), while the indications for biliary stenting, concomitant malignancies, lesion length, serum total bilirubin and CRP were positively associated with overall mortality. Only bilateral stent insertion was negatively associated with overall mortality ( Fig. 4 ). The multivariate analysis showed a higher risk of death in the cases of compression by lymph nodes (HR = 9.803,P= 0.003) and higher CRP (HR = 1.007,P= 0.005) and lower risk in those with bilateral SEMS insertions (HR = 0.316,P= 0.001, Table 5 ).
Discussion
In this study, we evaluated the difference in success rates, complications, patency loss, and overall survival between unilateral metal stent and bilateral Y-type metal stent placements in inoperable MHBS patients. To date, there have been no established guidelines for the optimal method or drainage extent in metal stent applications for MHBS, although various studies have been conducted on the topic [ 7-9 , 13] . According to the results of our study, Y-type metal stent insertion was inferior in terms of the technical successrate compared to unilateral metal stents, but similar in complication rates and patency loss, with superior overall survival. Therefore, Y-type metal stents can be a better treatment option unless the procedural difficulty is considered.
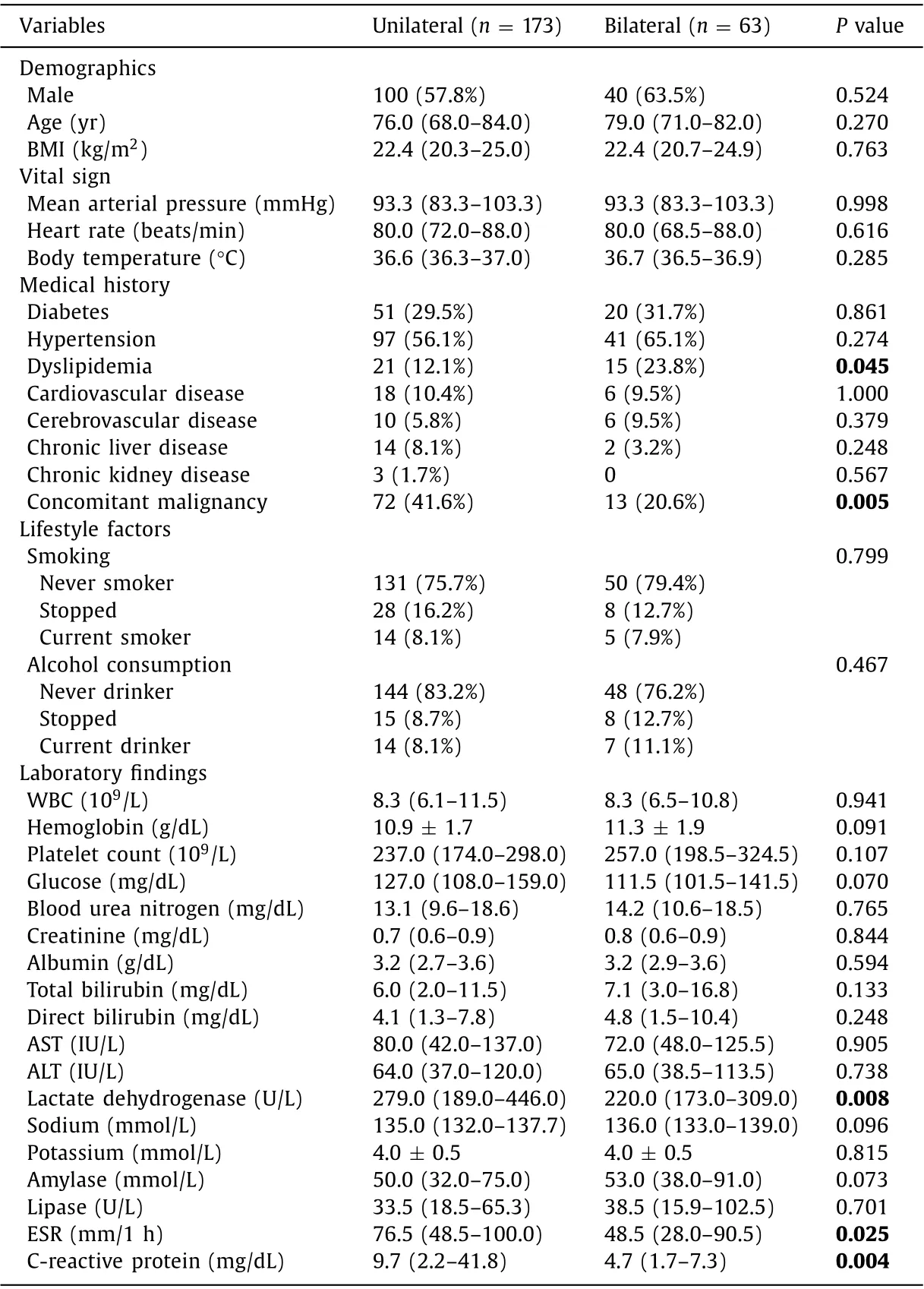
Table 3 Comparison of two biliary stent groups in demographic factor, medical histories, and pre-stent status of patients.

Fig. 1. The Kaplan-Meier curve for stent patency loss.
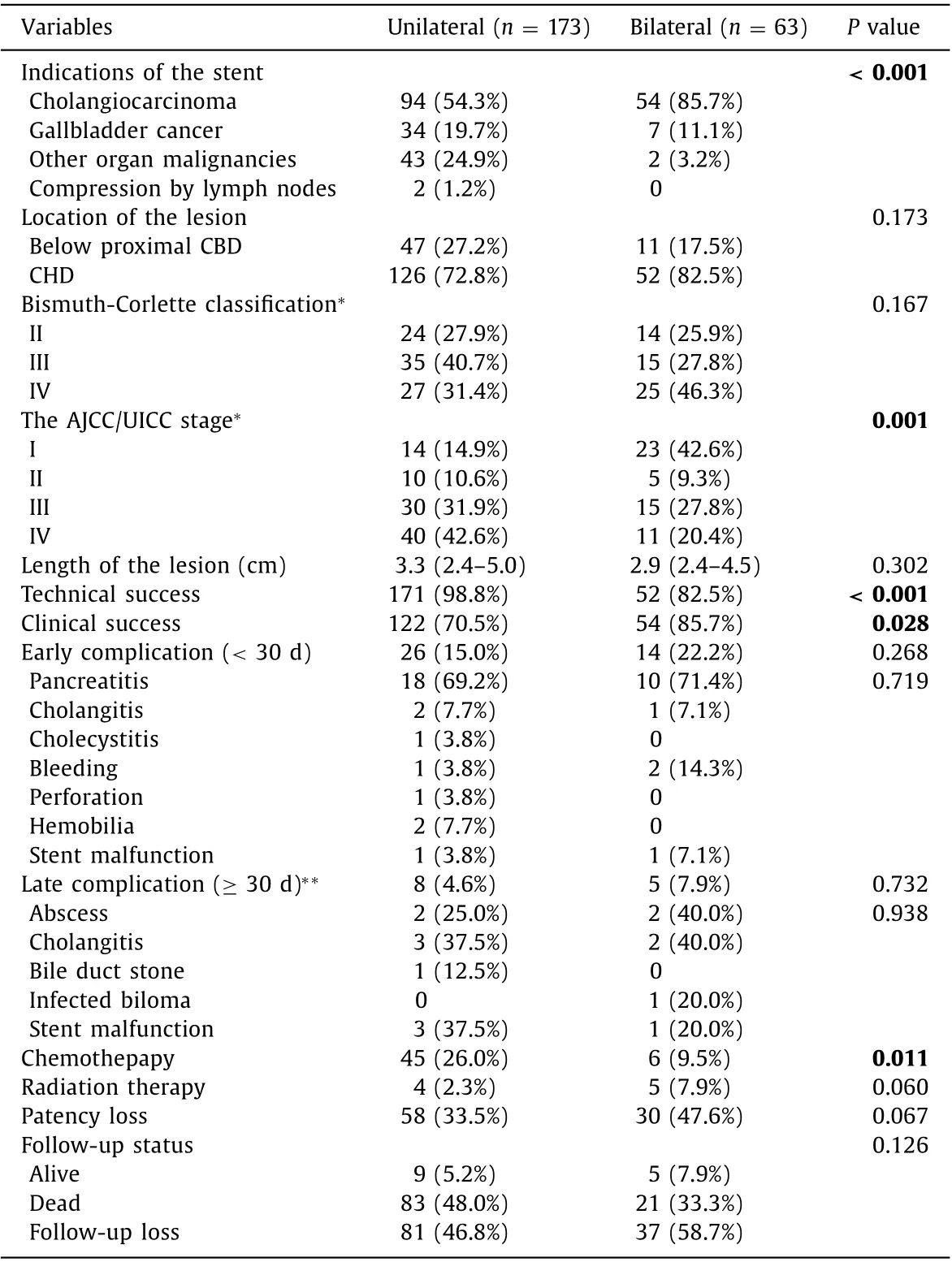
Table 4 Differences of two biliary stent groups in underlying malignancy and postprocedure outcomes.
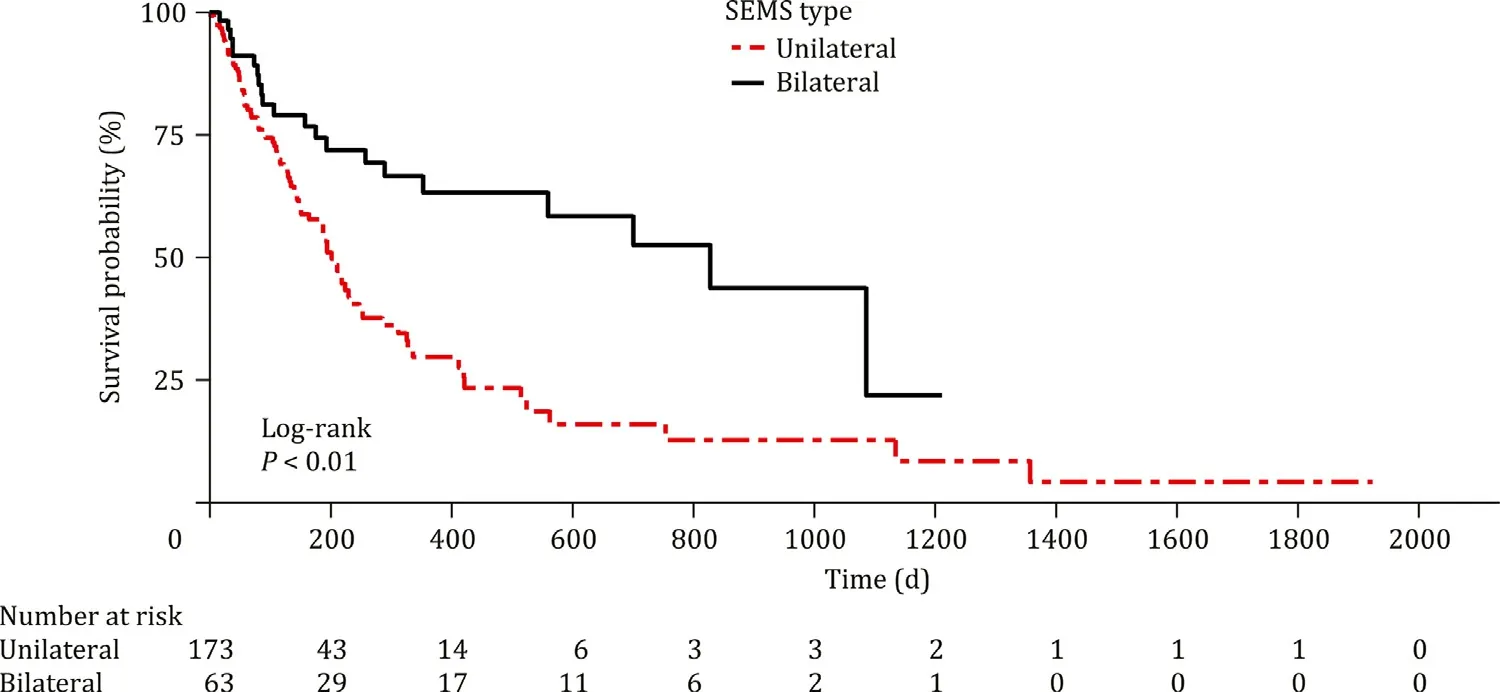
Fig. 2. The Kaplan-Meier curve for overall survival.
Previous studies on this topic have reported similar conclusions [ 2 , 8-10 , 12 , 20] . A retrospective study in Japan analyzed 46 MHBS patients who underwent endoscopic biliary stenting and confirmed that there was no difference in the incidence of early and late complications, consistent with our results [8] . A meta-analysis also similarly claimed the superiority of bilateral metal stent insertion [2] . Studies have reported that cholangiocarcinoma patients with metal stents on both sides showed better clinical success rates than those with a unilateral stent, and there was no significant difference in re-intervention or complication rates [ 9 , 12 , 20] . A recent large-scale retrospective study investigated better overall survival in bilateral metal stent group over unilateral metal stent [10] .
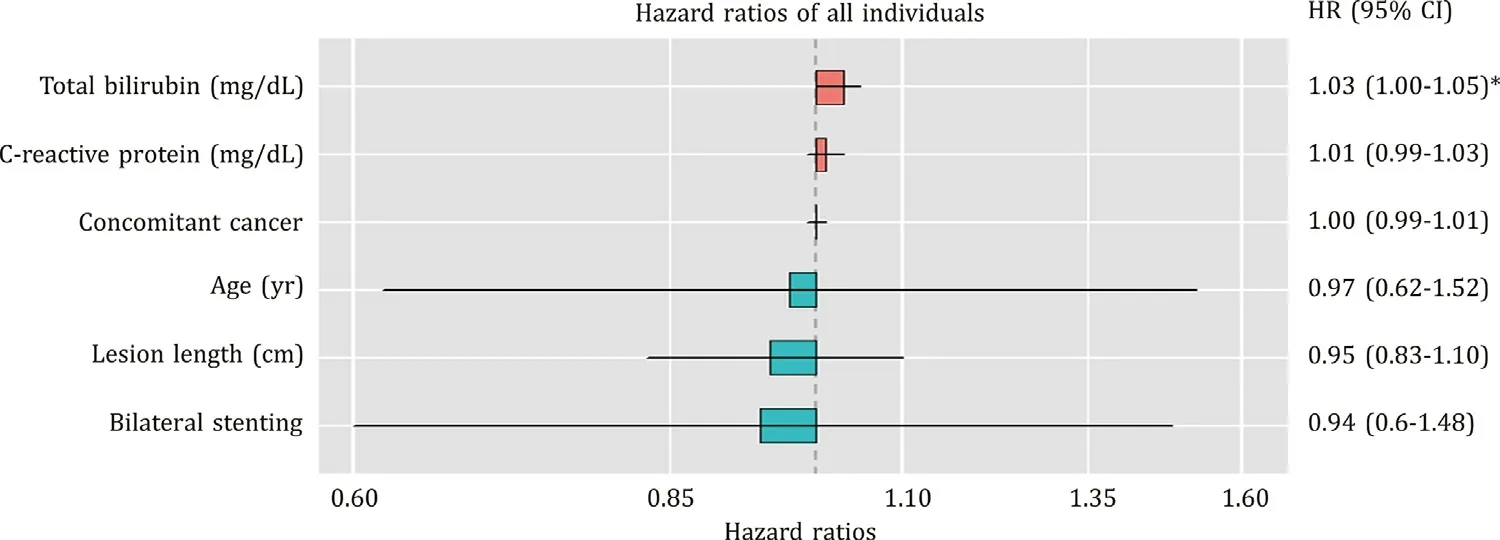
Fig. 3. Hazard ratio plot of variables for stent patency (*P < 0.1).

Fig. 4. Hazard ratio plot of variables for overall survival ( *P < 0.1, ** P < 0.05, ***P < 0.001).

Table 5 Multivariate Cox proportional hazards analysis for overall survival.
Several studies reported different results from ours [ 11 , 13 , 21] .A multicenter study in Korea demonstrated that the bilateral SEMS group showed advantages in terms of postprocedure complications and patency maintenance, with no significant difference in survival outcomes [13] . However, two different types of bilateral metal stenting, the side-by-side and the stent-in-stent methods, were analyzed without distinction. Regarding procedure-related complications, a study argued that unilateral metal stenting was recommended because more liver abscesses were observed in bilateral stent patients [11] . Nevertheless, the small number of subjects and the similar rate of severe complications in both stent groups should be considered when interpreting the results. In our study,the occurrence of liver abscesses also showed a high tendency in the bilateral stent patients, but there was no statistical significance.A recently published multinational and multicenter study reported significantly higher complication rates and death risk in the bilateral stent group of unresectable cholangiocarcinoma [21] . However,there were limitations that fewer cases of unilateral stents compared to bilateral stents were included in the study and a considerable number of patients were excluded due to insufficient medical records. Given that there were no acute complications in the unilateral stent group, it is worth doubting that the two groups compared were sufficient to represent each stenting method.
The strengths of this study were that every bilateral SEMS insertion was performed by the same technique (stent-in-stent),which led to better homogeneity of the study population. We were able to obtain multicenter-based data for a large number of patients. All participating hospitals are affiliated and within the same network with standardized patient management protocols. Accordingly, even in the multicenter design, no significant differences in the details of endoscopic stent implantation and patient management were seen before or after the procedure. Another strength of the study was that we investigated the HR for each variable adjusted through multivariate analysis for patency loss and overall survival.
There were some potential limitations to this study. First, because it was a retrospective study, the association between the type of SEMS insertion and outcomes does not necessarily imply a causal relationship. The second limitation was the substantial dropout rate of patients due to the retrospective design. To compensate for this point, the subjects with malignant hilar obstructions were limited to patients undergoing metal stent insertions with unilateral and bilateral stent-in-stent procedures. We also used strict criteria for patient selection based on the hospital evidence fulfilling demographic, laboratory, and clinical data during the follow-up period. Third, the technical success rate of bilateral SEMS insertions in this study was somewhat lower than that reported in other studies. In Korea, national health insurance coverage for bilateral metal stent placement in MHBS patients was granted relatively later than that in foreign countries. This study collected data on biliary SEMS insertions performed for 11 years,and the temporal difference between the two types of SEMS procedures might cause partial random effects because the unilateral procedures were performed for a longer time than the bilateral procedures. Finally, since the SEMS method was determined by the operator’s judgment, the presence of selection bias could not be excluded when comparing two SEMS groups. These limitations could be addressed through future prospectively designed studies targeting the same patient group and procedures.
In conclusion, for patients with inoperable MHBS, bilateral biliary drainage using SEMSs has similar patency loss and better performance in overall survival, compared with unilateral drainage.Although the success rate of the bilateral stenting is rather low,it is anticipated to become a more physiological and valuable therapeutic option for palliative therapy, given the future development of endoscopic techniques.
Acknowledgments
None.
CRediT authorship contribution statement
Ik Hyun Jo: Data curation, Formal analysis, Investigation,Methodology, Visualization, Writing - original draft. Chang-Nyol Paik: Conceptualization, Methodology, Project administration, Supervision, Writing - review & editing. Dae Bum Kim: Data curation, Investigation. Jaesin Lee: Data curation, Investigation.Jong Yul Lee: Data curation, Investigation. Jae Hyuck Chang: Data curation, Investigation. Kyu-Hyun Paik: Data curation, Investigation. Won-Suk Park: Data curation, Investigation.
Funding
None.
Ethical approval
This study was approved by the Institutional Review Board of The Catholic University of Korea (XC20RIDI0095) and adhered to theDeclarationofHelsinki.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Hepatocellular-cholangiocarcinoma with sarcomatous change:Clinicopathological features and outcomes
- Recent advances in immunotherapy for hepatocellular carcinoma
- Toll-like receptors and hepatitis C virus infection
- Involvement of the circular RNA/microRNA/glucose-6-phosphate dehydrogenase axis in the pathological mechanism of hepatocellular carcinoma
- Progress in hepatitis B virus-related acute-on-chronic liver failure treatment in China: A large, multicenter, retrospective cohort study using a propensity score matching analysis ✩
- From conventional two-stage hepatectomy to ALPPS: Fifteen years of experience in a hepatobiliary surgery unit