Has platelet-rich plasma any role in partial tears of the anterior cruciate ligament? Prospective comparative study
2021-06-18JuanPabloZicaroIgnacioGarciaMansillaAndresZuainCarlosYacuzziMatiasCostaPaz
Juan Pablo Zicaro, Ignacio Garcia-Mansilla, Andres Zuain, Carlos Yacuzzi, Matias Costa-Paz
Juan Pablo Zicaro, Ignacio Garcia-Mansilla, Andres Zuain, Carlos Yacuzzi, Matias Costa-Paz, Knee Division, Hospital Italiano de Buenos Aires, Buenos Aires 1181, Argentina
Abstract BACKGROUND Partial tears of the anterior cruciate ligament (ACL) are frequent, and there is still considerable controversy surrounding their diagnosis, natural history and treatment.AIM To examine patient-reported outcomes, physical examination and magnetic resonance imaging (MRI) findings of partial ACL tears treated with an intraarticular injection of platelet-rich plasma (PRP) compared to a control group.METHODS From January 2015 to November 2017, consecutive patients from a single institution with partial ACL tears treated nonoperatively were prospectively evaluated.Partial tears were defined as a positive Lachman test with a clear endpoint, a negative pivot-shift and less than 3 mm of side-to-side difference using the KT1000 arthrometer.Patients in group 1 were treated with one intraarticular injection of PRP and specific physical therapy protocol.Control group consisted of patients treated only with physical therapy.Prospective analyzed data included physical examination, Tegner activity level and Lysholm and International Knee Documentation Committee scores.Baseline MRI findings and at 6 mo follow-up were reviewed.Failure was defined as those patients with clinical instability at follow-up that required a subsequent ACL reconstruction.RESULTS A total of 40 patients where included, 21 treated with PRP injection with a mean follow-up of 25 mo [standard deviation (SD): 3.6] and 19 in the control group with a mean follow-up of 25 mo (SD: 5.68).Overall failure rate was 32.0% (n = 13).No significant differences were observed between groups regarding subjective outcomes, return to sport and failure rate.MRI findings revealed an improvement in the ACL signal in half of the patients of both groups.However, we did not find a significant relationship between MRI findings and clinical outcomes.CONCLUSION Overall, 95.0% of patients returned to sports at a mean follow-up of 25 mo.Mean time to return to sports was 4 mo.Out of these patients, almost 30.0% in each group had a new episode of instability and required surgery at a median time of 5 mo in group 1 and 8 mo in group 2.The addition of PRP alone was not sufficient to enhance any of the outcome measures evaluated, including MRI images, clinical evaluation and failure rate.
Key Words: Anterior cruciate ligament; Partial tears; Platelet-rich plasma; Non-operative treatment
INTRODUCTION
Partial tears account for 10% to 30% of all anterior cruciate ligament (ACL) tears[1,2].There is still considerable controversy surrounding the diagnosis, natural history and treatment of this type of lesion[3,4].Diverse criteria are often used to define a partial ACL tear.Magnetic resonance imaging (MRI) features include the estimation of the percentage of torn fibers, specific affected bundle (anteromedial or posterolateral) and location of the tear (proximal, middle third or distal).The physical examination is decisive in this type of lesion[1].Finally, arthroscopy remains the gold standard for the diagnosis of macroscopic integrity of the intact bundle.Intraoperative findings of intact remnant ACL fibers from femur to tibia insertion points confirm the diagnosis[5-7].
Regarding natural history, complete ACL tears have low intrinsic healing capacity, which prevent restoring anatomy and function.However, there has been some disagreement concerning whether partial ACL tears could heal.Though favorable results have been reported with either nonoperative or surgical treatment (such as repair or augmentation) as well as with biological approaches, some authors reported progression to complete deficiency of the ACL and symptomatic knee laxity with conservative treatment[4,7-10].
Platelet-rich plasma (PRP) has received much attention in the last years as a biologic alternative for the treatment of sports-related injuries.Various growth factors and bioactive proteins from the a-granules contained in platelets can potentially enhance tissue healing[11-14].PRP utilization in ligament injuries has grown remarkably[15-17].Regarding specifically to ACL injuries, the focus has been mostly on biologic augmentation to improve graft healing after a reconstruction, and only a few studies aimed to improve healing of the native injured ACL[18-22].
The purpose of this study was to examine patient-reported outcomes, physical examination and MRI findings of partial ACL tears treated with an intraarticular injection of PRP compared to a control group.
MATERIALS AND METHODS
Patient population
Following Institutional Review Board approval, all patients who were diagnosed with a partial ACL tear and treated nonoperatively between January 2015 and November 2017 were retrospectively selected from a database of prospectively collected data.Figure 1 shows the algorithm used for the diagnosis and treatment of partial ACL tears.It consists of an adaptation of a previously published algorithm by Sonnery-Cottetet al[1].We included patients with a positive Lachman’s test with a firm endpoint, negative pivot shift, a side-to-side differential laxity less than 3 mm measured by arthrometer (KT-1000 knee arthrometer, MEDmetric Corp.) and MRI signs of partial ACL tear.Patients with a differential laxity between 3 and 5 mm without meniscal lesions and/or participation in high-risk sports were also included.
The exclusion criteria were as follows: patients younger than 18-years-old, patients with less than 6 mo follow-up, patients diagnosed after 1 mo of injury, previous ipsilateral ACL tear or reconstruction, confirmed or suspected contralateral ACL injury, diagnosis of concomitant ipsilateral posterior cruciate ligament, posterolateral corner or grade 3 medial collateral ligament injury and arthritis (International Knee Documentation Committee C or higher).
Nonoperative treatment consisted of one intra-articular injection of leukocyte reduced PRP during the first 4 wk after injury (within the inflammatory phase) and specific physical therapy protocol (group 1).However, not all patients were able to receive the PRP injection, mostly because medical insurance coverage or refusal from the patient to do so.These patients were considered the control group (group 2).
Data collection and definitions
All medical care interventions are centrally registered in a computerized data repository, with only one electronic health record per person.After initial consultation and treatment, patients underwent clinical follow-up at 1, 3, 6 and 12 mo by the same observer.Variables analyzed included patient gender, age, Tegner activity Score both at time of injury and at time of final follow-up, return to sports (RTS) rate, time to RTS and subsequent surgeries.Subjective assessment included Lysholm and International Knee Documentation Committee scores.
Objective stability was tested at the time of injury and at 6 mo follow-up with a knee arthrometer test (KT-1000 knee arthrometer, MEDmetric Corp.), and the manual maximum difference between knees (in mm) was used for analysis of reported mean side-to-side differences.All patients were evaluated by a single orthopedic observer (JPZ-staff member/knee surgeon).
Baseline MRI findings and at 6 mo follow-up were reviewed.Images were analyzed according to a classification published by van Meeret al[23].Nine features are used to assess the ACL on MRI: fiber continuity, signal intensity, slope of ACL with respect to the Blumensaat line, distance between the Blumensaat line and ACL, tension, thickness, clear boundaries, assessment of original insertions and assessment of intercondylar notch.A total score is determined by summing scores for these 9 features.A score of 10 is maximally abnormal for all features, whereas a score of 0 is normal for all features.Lesion localization was also determined (proximal, middle third and distal).All images were evaluated by a single orthopedic observer (JPZ) who was blinded to the treatment group.
Failure was defined as those patients with clinical instability at follow-up that required a subsequent ACL reconstruction.
PRP preparation
On the basis of previously published reports on criteria that influence the composition or biological effect of PRP[24], we included the following information regarding PRP preparation.After harvesting 150 mL of blood, the extracted unit was doubled centrifuged in a Thermo Scientific Sorvall BP-16 Refrigerated Blood Bank Centrifuge.First, a light centrifugation for 4 min at 1400 rpm to separate the PRP from the globular mass was performed.The product obtained was separated into satellite bags without opening the circuit, guaranteeing the sterility of the process.Next, the PRP was centrifuged for 6 min at 3000 rpm to achieve a higher concentration of the product.At the end of the process, quality control was carried out on the product through an XT ROCHE hematological counter.It consists of volume, platelet count, white blood cell count and calculation of product concentration.
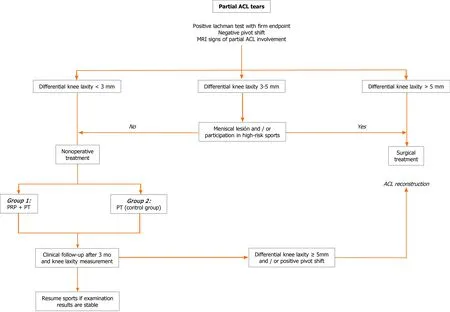
Figure 1 Flow chart for partial anterior cruciate ligament tears.
Injection protocol
Group 1 (PRP group) received a single intra-articular injection of PRP.A median of 8 mL (6-10) was injected.All injections were performed by one of the authors (Zicaro JP).Intra-articular injection aiming at the ACL was performed as a standard sterile procedure.A 25-gauge 3.0-inch needle was inserted through the skin in a similar localization as a medial portal, towards the ACL femoral insertion.No imaging was used as guidance.The median concentrations of platelets and white cells of the product are detailed in Table 1.After the procedure, full weight bearing, cryotherapy and daily life activities was allowed as tolerated.No post treatment bracing was administered.Physical therapy protocol began after 72 h of the injection.
Physical therapy protocol
Even though not all patients performed the rehabilitation at the same center, both groups received the same rehabilitation protocol.The goals of the first 4 wk were to recover range of motion, prevent quadriceps inhibition and normalize proximal muscle strength.Nonimpact exercises such as bicycle or swimming were allowed during the first week.Linear impact and strengthening exercises began 6 wk after injection, with progression to multiplanar exercises between 8 to 10 wk.The goal was to return to their previous sport not before 3 to 4 mo after injection.
Statistical analyses
Descriptive statistics including means, standard deviations (SDs), medians and quartile ranges were applied as appropriate to assess the available demographic, surgical, physical examination and patient-reported outcome data.Statistical hypothesis testing was performed using the Fisher exact test and Wilcoxon rank-sum test.Categorical data was performed using Chi square test.Analysis was performed with 95% confidence interval, andPvalues < 0.05 were considered statistically significant.All statistical analyses were performed using STATA version 13.
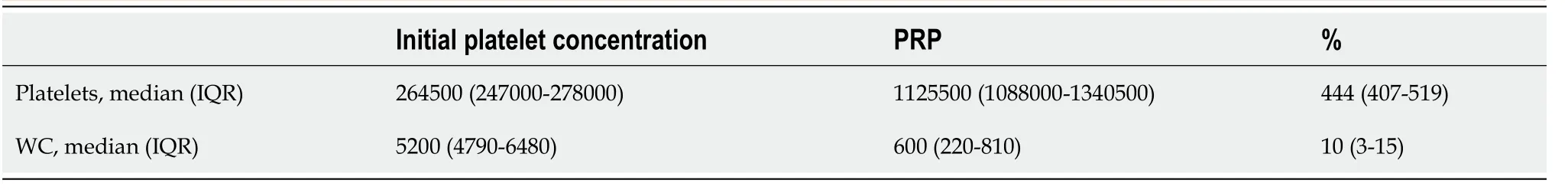
Table 1 Details of the baseline and platelet rich plasma platelets and white cells concentrations
RESULTS
A total of 40 patients where included.In total, 21 treated with PRP injection (group 1) with a mean follow-up of 25 mo (SD: 3.60) and 19 in the control group (group 2) with a mean follow-up of 25 mo (SD: 5.68).The overall median age was 26.0-years-old (IQR 22.5-35.0).Demographic data is shown in Table 2.The only statistically significant difference between groups was gender; no females were included in the control group (P= 0.021).
Results at final follow-up are shown in Table 3.One patient in each group (5.0%) was unable to RTS due to subjective instability.The other 95.0% in each group were able to return to their previous sports level.Overall mean RTS time was 4 mo (SD: 1.06), without significant differences between groups.We found no significant differences for subjective outcomes between groups.
Regarding objective stability, at 6 mo follow-up in group 1, 13 presented a decrease in the side-to-side difference, 7 remained with the same difference, and 1 had 2 mm more.In group 2, 9 had a decrease in the side-to-side difference, 9 remained with the same difference, and 1 had 1 mm more.None of the patients had a positive pivot shift at final follow-up.
According to van Meeret al[23], MRI classification for partial ACL tears at baseline for most patients were classified between 4 and 10 in both groups (Table 4).At 6 mo follow-up, more than 50.0% of patients in both groups where classified as 0 and 3, showing an improvement in the ACL MRI signal (Figure 2).
Overall failure rate was 32.0% (n= 13) with no significant differences between groups (Table 3).Five failures in group 1 where Tegner 7, one Tegner 8 and one Tegner 5.In group 2, four failures where Tegner 7 and two Tegner 6.We found no significant differences when analyzing the location of the lesion and failure in both groups.Two proximal (2/10) and five mid-substance (5/11) tears failed in group 1 (P= 0.21).Four proximal (4/12) and two mid-substance (2/7) tears failed in group 2 (P= 0.83).
DISCUSSION
The present study evaluated the results of a series of patients with partial ACL tears treated nonoperatively.No significant differences were identified between patients treated or not with a single intraarticular injection of PRP.Overall, 32.0% failures were observed in both groups at a mean follow-up of 25 mo.The remaining 67.0% of patients were able to RTS in a mean of 4 mo.
A key factor in the treatment of partial ACL tears is a correct diagnosis.There has been some disagreement with regard to the definition of this lesion, and most of them are underdiagnosed.Some authors agree that physical examination cannot differentiate a partial ACL tear from an intact ACL[25,26].On the other hand, MRI has a low level of accuracy for the diagnosis of partial ACL tears (25.0%-50.0%), mainly because of the significant overlap of the imaging findings between partial and complete tears, mucoid degeneration of the ACL and the initial post-traumatic hematoma[27].Therefore, many surgeons rely on arthroscopy to define the extent of injury.A recently published study analyzed the correlation between preoperative clinical assessment and the arthroscopic examination in patients with ACL tears[26].While evaluation under anesthesia demonstrated a high sensitivity for the detection of partial tears (100%), it was not necessarily specific (65.5%) and resulted in a high number of false positive partial tears.MRI, on the other hand, demonstrated a relatively high sensitivity (90.9%) and specificity (85.7%).The accuracy of MRI (86.3%) was also greater than that of evaluation under anesthesia (69.5%).These results suggested that MRI is 1.24 times more likely to result in correctly diagnosing a partial tear, which was a statistically significant finding.
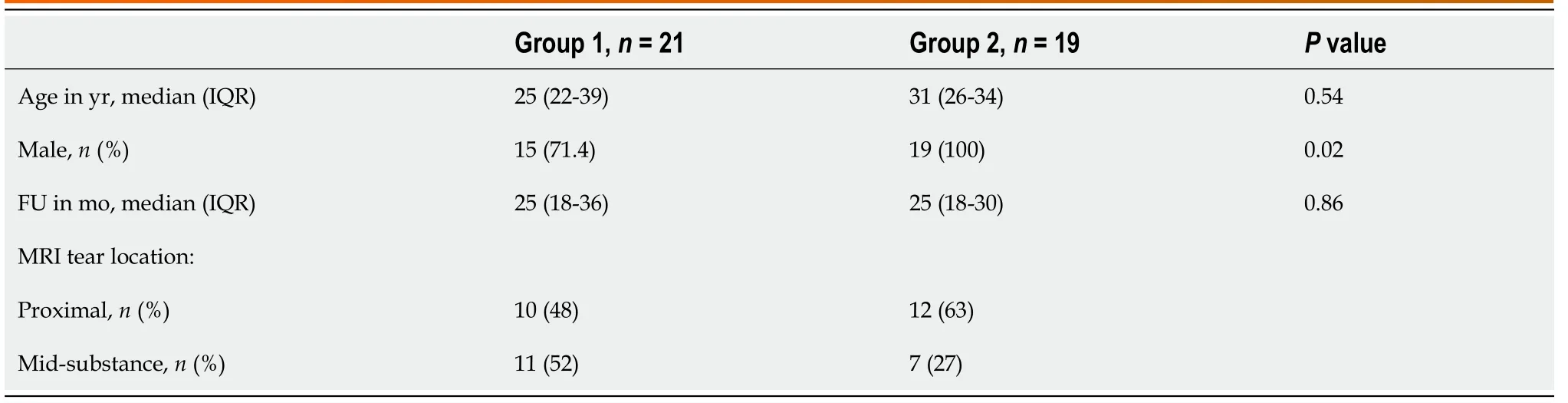
Table 2 Demographic data
Table 3 Results at final follow-up
Table 4 Magnetic resonance image Van Meer classification at baseline and at 6 mo
Regarding nonsurgical management of partial ACL tears, Pujolet al[8] performed a systematic review and analyzed 12 articles where diagnosis was confirmed on arthroscopy, without ACL surgery.A total of 436 patients were followed up over the period 1976-1997 with a mean follow-up of 5.2 years (range 1.0-15.0).They found good short- and mid-term functional results, especially when patients limited their sports activities.The mean rate of revision ACL was 8.1% (0%-21.0%).RTS rate was 52.0% (21.0%-60.0%), lower than our findings, with 95.0% of patients returning to the same level.Noyeset al[7] reported a 38.0% progression to a complete rupture in a prospective evaluation of 32 patients with a partial ACL tear.Lehnertet al[28] reviewed a series of 39 partial ACL tears 5 years after injury and found that 56.0% had progressed to ACL deficiency.Finally, Fritschyet al[9] reported a rate of 42.0% in 43 patients.and Fruensgaardet al[29] reported 51.0% in a series of 41 patients.Although these results may be comparable to our overall 32.0% failure, these findings are to be viewed in the light of the indications for ACL surgery in vogue 30 years ago.It is important to highlight that in some cases, side-to-side difference in KT-1000 arthrometric evaluation was greater, probably due to a lack of healing of ACL fibers, particularly cases when the anteromedial bundle was affected.Nevertheless, most of these patients were active in their sports practice.
Figure 2 Magnetic resonance images.
The use of biologic agents, including growth factors, PRP, stem cells and biological scaffolds, has been the focus of current research in ACL repair and healing[3].In a systematic review analyzing biologic agents for ACL healing, the large majority of articles (21 out of 23) were focused on their application during ACL reconstructive surgery, whereas only two trials, both case series, investigated their potential in partial ACL tears[19].Centenoet al[30] published a prospective case series of 10 patients treated with percutaneous injection of autologous bone narrow nucleated cells, using fluoroscopic guidance.Patients were included if they had a grade 1, 2 or 3 ACL tear without greater than 1 cm retraction.Treatment protocol consisted of a preinjection of a hypertonic dextrose solution into the ACL followed by a reinjection of 2-3 mL of bone marrow cells, PRP and platelets 2-5 d after, using the same procedure.Seven of ten patients demonstrated improvement in MRI measures of ACL integrity at a mean follow-up of 3 mo.The lack of a control group and the multiple component of the protocol are the main shortcomings of their methods.On the other hand, Seijaset al[20] published a retrospective case series of 19 football players (Tegner 9-10) with a partial ACL tear treated with an arthroscopic intraligamentary application of PRP (leukocyte poor).All cases presented a complete rupture of the anteromedial bundle with an intact posterolateral bundle.RTS rate was 84%.Average RTS in 15 patients Tegner 9 was 16 wk and in 2 patients Tegner 10 was 12 wk.In our study, mean time to return to sport was 4 mo.
Regarding the use of MRI in partial ACL tears, we consider there is an important role in the diagnosis and follow-up.However, these results must not be considered in isolation.Although we thoroughly analyzed nine different imaging parameters, no significant correlation was found between laxity and MRI images.Neither association was identified between lesion localization and treatment failure.These findings might be due to the low number of patients.
The lack of standardization of PRP protocols has been published recently[24].Chahlaet al[24] analyzed 105 studies finding high inconsistences in the way PRP preparation was reported.The majority of studies did not provide sufficient information to allow the protocol to be reproduced, which also prevents comparison of the PRP products.Based on this review and following the proposed guidelines, we included in our study data regarding PRP preparation and composition of the PRP delivered.
It is plausible that a number of limitations may have influenced the results obtained.First, the sample size might be considered to be low.However, a sample size estimation was not possible due to the lack of studies published with the same treatment.Although a control group was established, this group was not randomized, which may raise the possibility of a selection bias.Another possible source of error related to the procedure.The injections were not guided by imaging, and patients underwent only one injection.Nevertheless, there is no standardization in terms of how much and how many PRP injections are required for better results.
CONCLUSION
Our research provided further evidence about natural history of nonoperative management of partial ACL tears.Overall, 67% of patients with this type of lesion RTS in a mean of 4 mo without clinical instability either with or without an intra-articular PRP injection.The addition of PRP alone was not sufficient to enhance any of the outcome measures evaluated, including MRI images and clinical evaluation.
ARTICLE HIGHLIGHTS
Research background
Platelet-rich plasma (PRP) is being widely used in many orthopedic areas.The use of PRP has for “healing” purposes is still controversial in the field of partial ligamentous lesions.
Research motivation
To our knowledge, there are no comparative series reported in the literature regarding the use of PRP for partial anterior cruciate ligament (ACL) tears.
Research objectives
The aim was to prospectively compare the patient-reported outcomes, rerupture rate and magnetic resonance (MR) findings in patients with partial ACL tears treated with a single PRP intra-articular injection compared to a control group.
Research methods
Patients who met the inclusion criteria for stable partial ACL tears were divided into two groups.One group received a single intra-articular leukocyte-poor PRP injection within the first 4 wk after the lesion.Both groups received the same rehabilitation protocol.Clinical objective outcomes (KT1000 arthrometric evaluation), subjective outcomes, time to return to sports, rerupture rate and MR findings were evaluated.PRP preparation data was detailed.
Research results
Forty patients where included, 21 treated with PRP injection (group 1) (mean followup of 25 mo) and 19 in the control group (group 2) (mean follow-up of 25 mo).Overall,95% of patients in each group returned to their previous sport at a mean time of 4 mo.After 6 mo follow-up, more than 50% of patients improved the ACL signal intensity in the MR.Overall failure rate was 32% (n = 13) with no significant differences between groups.
Research conclusions
A single PRP intra-articular injection was not sufficient to enhance any of the outcome measures evaluated, including MR images and clinical evaluation.Overall, 67% of patients returned to sports in a mean of 4 mo without clinical instability either with or without an intra-articular PRP injection.
Research perspectives
Further rigorous and objective studies including more patients and different PRP preparations, such as less platelet concentrations or leukocyte-rich preparations,would be useful to determine the true efficacy of PRP for enhancing healing properties of partial ACL lesions.
杂志排行
World Journal of Orthopedics的其它文章
- Developing an enhanced recovery after surgery program for oncology patients who undergo hip or knee reconstruction surgery
- Slacklining: A narrative review on the origins, neuromechanical models and therapeutic use
- Off-the-shelf 3D printed titanium cups in primary total hip arthroplasty
- Evidence-based approach to providing informed consent for hip fracture surgery during the COVID-19 era
- Dermatomyositis and polymyositis in total hip arthroplasty
- Outcome and revision rate of uncemented humeral head resurfacing:Mid-term follow-up study