Developing an enhanced recovery after surgery program for oncology patients who undergo hip or knee reconstruction surgery
2021-06-18MariaBourazaniEleniAsimakopoulouChrysseidaMagklariNikolaosFyrfirisIoannisTsirikasGiakoumisDiakoumisMarthaKelesiGeorgiaFasoiTheodorosKormasGunhildLefaki
Maria Bourazani, Eleni Asimakopoulou, Chrysseida Magklari, Nikolaos Fyrfiris, Ioannis Tsirikas, Giakoumis Diakoumis, Martha Kelesi, Georgia Fasoi, Theodoros Kormas, Gunhild Lefaki
Maria Bourazani, Eleni Asimakopoulou, Chrysseida Magklari, Nikolaos Fyrfiris, Gunhild Lefaki, Department of Anesthesiology, “Saint-Savvas” Anticancer Hospital of Athens, Athens 11522, Attica, Greece
Maria Bourazani, Martha Kelesi, Georgia Fasoi, Department of Nursing, University of West Attica, Athens 12243, Attica, Greece
Ioannis Tsirikas, Physiotherapy Center, Egaleo, Athens 12242, Attica, Greece
Giakoumis Diakoumis, Theodoros Kormas, Orthopedic Clinic, “Saint-Savvas” Anticancer Hospital of Athens, Athens 11522, Attica, Greece
Abstract Enhanced recovery after surgery (ERAS) protocols are applied in orthopedic surgery and are intended to reduce perioperative stress by implementing combined evidence-based practices with the cooperation of various health professionals as an interdisciplinary team.ERAS pathways include pre-operative patient counselling, regional anesthesia and analgesia techniques, post-operative pain management, early mobilization and early feeding.Studies have shown improvement in the recovery of patients who followed an ERAS program after hip or knee arthroplasty, compared with those who followed a traditional care approach.ERAS protocols reduce post-operative stress, contribute to rapid recovery, shorten length of stay (LOS) without increasing the complications or readmissions, improve patient satisfaction and decrease the hospital costs.We suggest that the ERAS pathway could reduce the LOS in hospital for patients undergoing total hip replacement or total knee replacement.These programs require good organization and handling by the multidisciplinary team.ERAS programs increase patient's satisfaction due to their active participation which they experience as personalized treatment.The aim of the study was to develop an ERAS protocol for oncology patients who undergo bone reconstruction surgeries using massive endoprosthesis, with a view to improving the surgical outcomes.
Key Words: Hip or knee replacement; Joint reconstruction; Enhanced recovery after orthopedic surgery; Fast-track orthopedic surgery; Enhanced recovery after surgery pathways in orthopedic surgery; Rehabilitation after hip or knee replacement
INTRODUCTION
Orthopedic prosthesis has been used globally since the 1960s.The aim is to restore the function of the joint replaced and to improve the patient's quality of life[1].The first primary hip arthroplasty with a metal prosthesis was performed in 1953 by the Englishman George McKee[2].Since then, different interventions have been developed varying in terms of their design and construction material, for a number of joints, revolutionizing the specialty of orthopedics[3,4].Nowadays, the use of orthopedic prostheses is very common.It is estimated that more than 600000 knee arthroplasties are performed in the United States each year[5].
Endoprostheses are used in two areas of orthopedics: (1) In reconstructions of joints, which have been damaged by trauma, degenerative or systemic diseases and need to be replaced by metal endoprosthesis (semi- arthroplasty of the hip, knee and shoulder, total ankle arthroplasty and total hip and knee arthroplasty) for better functional and long-term results[6]; and (2) In orthopedic oncology after tumor resection due to malignancies or, less often, benign diseases, where bone and tissue deficits are restored with extensive prosthesis.Until about 1970, the only treatment for bone tumors and soft tissue sarcomas was amputation, without improving patient survival though.Since then, rapid advances in prosthesis technological has allowed the rescue of limps, which in combination with chemotherapy have significantly improved the survival rate[7].
The idea of enhanced recovery pathways was first introduced by Kehlet in the late 1990s, improving the mental and physical effects of post-operative stress on the recovery and general clinical condition of a patient undergoing surgery[8,9].The concept of fast-track surgery, as it is widely known, included a combination of minimally invasive surgical techniques, combined anesthesia and analgesia, early feeding and early mobilization[10,11].It was initially applied to colorectal surgery and later to almost all general surgeries[12,13].
Nowadays, fast-track programs have evolved into enhanced recovery after surgery (ERAS) protocols applied by a variety of surgical specialties, including orthopedics.Studies have shown that ERAS protocols reduce length of stay (LOS) without increasing mortality, readmissions or complications rates, decrease hospital cost and enhance patient satisfaction[14,15].
ERAS protocols are intended to reduce perioperative stress, which causes metabolic and immune changes with side effects on the various body systems and increases susceptibility to post-operative infections[14,16,17].This is achieved through a combination of multifactorial evidenced-based practices performed by various health specialties collaborating in an interdisciplinary team (surgeon, anesthesiologist, nurse, physiotherapist,etc.).An ERAS protocol is divided into three phases: Pre-operative, intraoperative, and post-operative (Table 1).It often begins before the patient’s admission to the hospital and continues after discharge.The active participation of patients is required throughout the program[17-19].
According to ERAS protocols, there are several components of perioperative care that affect stress response and accelerate recovery.These include pre-surgical counselling, short fasting period, early mobilization, bowel and bladder preparation, anesthesia and analgesia, thrombocytopenia, prevention of nausea and vomiting and fluid management[20].
PRE-OPERATIVE PERIOD
Informed consent
In order for the patient to follow an ERAS protocol, it is necessary to be informed about all the care practices they will receive, the expected results of their care and the active role they will play in the program, and be acquainted with all the members of the interdisciplinary team.Some patients feel reticent about new practices out of either ignorance or fear, so they disagree or need time to decide.The interdisciplinary team should answer each question of the patient and give them the written protocol instructions[16,20,21].
Patient’s medical history and determination of vital signs
After the diagnosis and before the surgery is decided by the surgeon, the multidisciplinary team meets the patient to determine their vital signs and identify any health conditions they may have that may be improved until the planned surgery[22,23].Patients at high risk for post-operative complications are identified by calculating individual risk based on family history, symptoms, and health status measurement using specific questionnaires[24,25].One such tool is the Revised Cardiac Risk Index (Lee Criteria), which assesses the risk of more serious heart events based on a history of ischemic heart disease, heart failure, stroke, insulin-dependent type II diabetes, serum creatinine > 177 μmol/L and high risk surgery[24,26-28].There are many specialized tools for measuring a patient's physical function, severity of surgery and anesthesia, post-operative mortality and morbidity, as well as various measurements of frailty related to clinical outcomes from surgery, supported by the American Society of Anesthesiologists[26-28].
Counseling
ERAS protocols aim to increase the patient's physiological and functional reserves before surgery, which is, in fact, their main difference from fast-track proto-cols[11,29,30].Studies have demonstrated the effectiveness of targeted pre- operative counseling.In particular, to reduce the risk of respiratory complications, such as infection or atelectasis, and the risk of post-operative wound inflammation, pre-operative smoking cessation within 2-4 wk of surgery is recommended[31,32].If this is not possible, then it is recommended to reduce the number of cigarettesperday rather than quitting smoking, as this would result in a reflex increase in secretions that would have the opposite effect.Patients who consume alcohol have a slow recovery and increased rates of post-operative complications, so it is recommended to follow alcohol withdrawal programs before surgery when possible[33-35].
Pre-operative fasting
According to ERAS protocols, the routine of “being nil by mouth” from midnight before surgery to patients who are going to be operated is considered obsolete and incorrect.Fasting increases the peri-operative stress and its adverse effects as catabolism, insulin resistance and hyperglycemia[36,37].ERAS protocols recommend shortening the pre-operative fasting time; clear fluid fasting for 2 h and solid food fasting for 6 h before surgery are enough for most patients.Patients with gastroparesis, esophageal achalasia or previous upper gastrointestinal surgery, morbid obesity and previous history of post-operative nausea and vomiting are excluded[38,39].Preoperative administration of oral carbohydrate drinks has been studied in recent years and shown to significantly improve insulin resistance without significant impact on the recovery time of patients undergoing hip or knee replacement surgery[40-42].Although carbohydrate intake in orthopedic surgery has been shown to improve patients’ well-being, metabolism, and post-operative pain, it is not recommended as a standard practice[17,43,44].
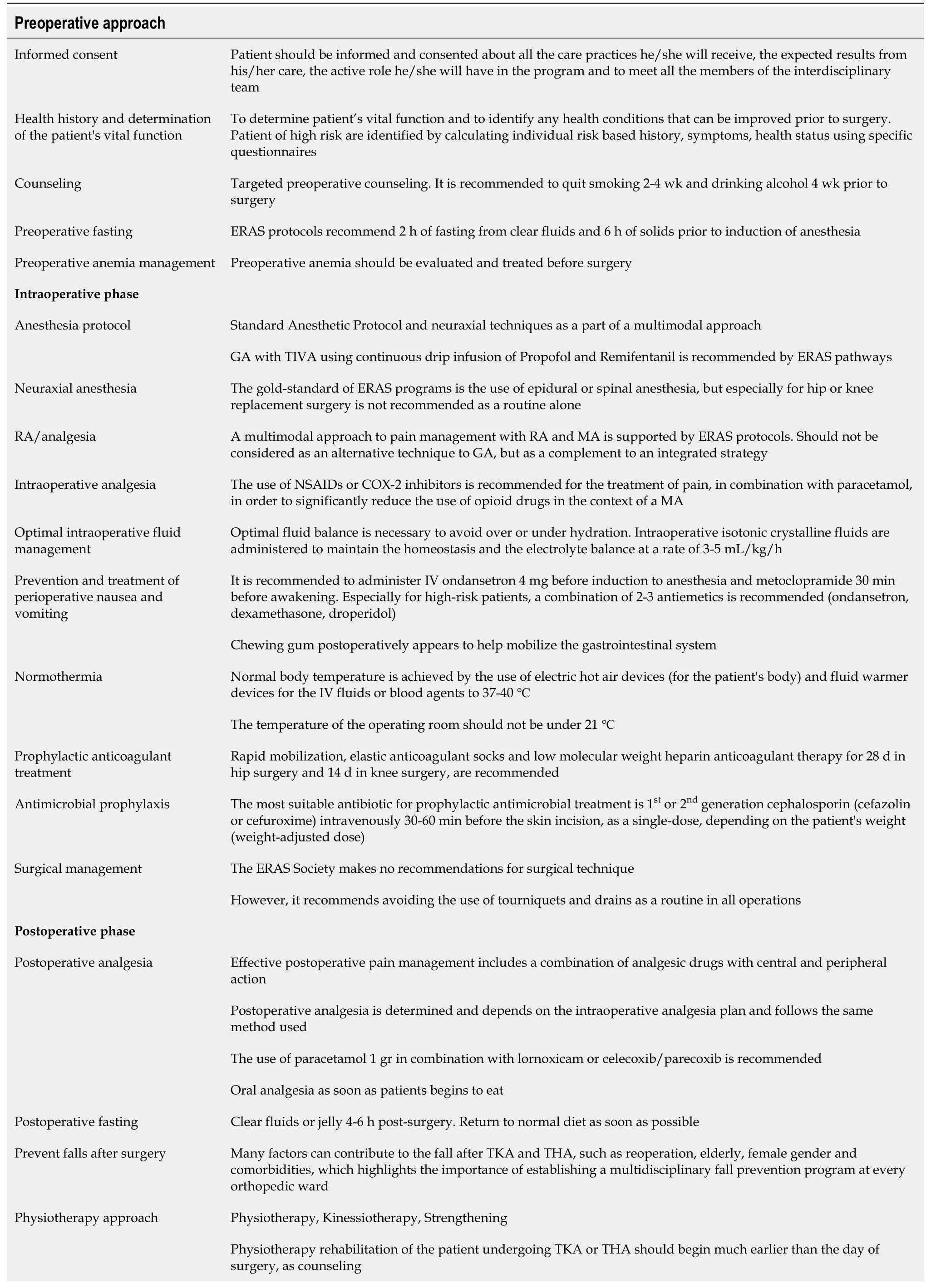
Table 1 Summary of enhanced recovery after surgery pathways for oncology patients who will undergo hip or knee reconstruction surgery
ERAS: Enhanced recovery after surgery; TIVA: Total intravenous anesthesia; BMI: Body mass index; GA: General anesthesia; MA: Multimodal analgesia; NSAIDs: Nonsteroidal anti-inflammatory drugs; COX-2: Cyclooxygenase-2; TKA: Total knee arthroplasty; THA: Total hip arthroplasty; RA: Regional anesthesia.
Pre-operative anemia management
Pre-operative anemia should be evaluated and treated before surgery.Pre- operative anemia is associated with increased rates of allogeneic transfusion, longer stay in hospital, increased risk of post-operative infection, higher post- operative morbidity, complications and readmissions[45,46].Clinical intervention studies about preoperative and post-operative treatment with iron (Fe) or erythropoietin have reported statistically and clinically significant reduction in allogeneic blood transfusions[46-48].The algorithm used to detect and correct pre- operative anemia by ERAS certified centers was associated with a reduction in the rate of transfusions, LOS, hospital readmissions, admissions to intensive care units and hospital cost[49].
INTRA-OPERATIVE AND POST-OPERATIVE PERIODS
Anesthetic protocol
In order to extract comparable results from an ERAS protocol, a standard anesthetic protocol must be followed.However, this is not always possible (for various reasons), which causes problems with regard to the homogeneity of parameters and the quality of the study methodology, thus challenging its reliability[50,51].General anesthesia (GA) with total intravenous anesthesia using continuous drip infusion of Propofol and Remifentanil is recommended by ERAS pathways.In vitro studies have shown the properties of propofol as an anti-inflammatory agent and as a stimulant of immune response with beneficial effects on cancer recurrence prevention[52-55].Oncology patients have peculiarities compared to the rest of the population.They are usually patients with metastatic or primary disease who have undergone chemotherapy and/or radiotherapy and have increased risk of intraoperative complications, especially during bone reconstruction with endoprosthesis and use of bone cement[56].After a systematic review and meta-analysis of anesthesia techniques used for total knee replacement (TKR) and total hip replacement (THR) in non-cancer patients, the choice of anesthesia type was based on the type of surgery and the patient's general condition[57].The level of evidence was low for GA or neuraxial anesthesia (NA), but the recommendation strength for both types of anesthesia was strong for patients undergoing hip or knee arthroplasty[52,58].
Neuraxial Anesthesia
The gold-standard of ERAS programs is the use of epidural or spinal anesthesia, but it is not recommended as a routine specifically for hip or knee replacement surgery[57,59,60].There is a strong recommendation from the ERAS society not to inject high doses of opioids into epidural or spinal cord to avoid the risk of respiratory depression, post-operative nausea-vomiting (PONV), pruritus and urinary retention[61-63].Morphine in low doses (0.1-0.18 mg) prevents the risk of respiratory depression and provides an adequate analgesic effect compared with continuous local anesthetic infusion after peripheral nerve blocks (PNB).NA with morphine promotes early patient mobilization[64].Recent clinical trials using non- opioid formulations, such as bupivacaine, have shown excellent results with minimal risk of complications[51,65].
In ERAS protocols for hip or knee replacement, NA is recommended for its superiority over GA in reducing the stress response and the insulin resistance[19,66].NA offers great analgesic benefits and reduces LOS and hospital costs, but may cause side effects such as respiratory depression, PONV and pruritus, therefore not recommended as a routine[19].
Regional anesthesia/analgesia
Regional anesthesia (RA) can reduce the incidence of cancer recurrence due to reduced need for opioids, suppression of the sympathetic nervous system, reduction of perioperative stress, and immediate anti-inflammatory and anticancer effect on immune system[54,67,68].Although there are many studies that support the positive effects of RA on cancer recurrence, more studies are needed to determine the effects of RA on orthopedic cancers.Data may be incomplete, as orthopedic oncology procedures often involve resection of large bones and/or muscle groups and can take up to 12 h, making GA more common[69].However, these resections can be performed using RA, either alone or in combination with GA[55,69].
RA provides a greater advantage in joint reconstruction as it delivers sufficient anesthesia for orthopedic surgery and great post-operative analgesia, inhibits the release of stress hormones and reduces insulin resistance.A multimodal approach to pain management with RA and multimodal analgesia (MA) is supported by ERAS protocols[17,68].RA always plays an important role in minimizing the intra- operative requirements for opioids and should not be considered as an alternative to GA, but rather as a complement to an integrated strategy[68].
Morphine has a negative effect on the functioning of the immune system and it is strongly recommended to minimize doses[70-72].MA is of paramount importance in the perioperative period, because it helps to reduce the need for opioids[73].Opioid sparing analgesia based on intravenous lidocaine, nonsteroidal anti-inflammatory drugs (NSAIDs) and ketamine has been found to maintain immune function[73].
RA seems to benefit most elderly and debilitated or seriously ill patients or those undergoing major orthopedic and thoracic surgeries[74].Recent studies have shown that total arthroplasty may be possible with the use of RA in all age groups, regardless of the severity of the comorbidity[58,67].
ERAS programs significantly reduced the incidence of post-operative complications, such as myocardial ischemia and mortality, over a period of 30 d compared to conventional treatment[58,66].
Intra-operative analgesia
For purpose of pain manageme nt, using a combination of NSAIDs or inhibitors of cyclooxygenase-2 (COX-2) with paracetamol (acetaminophen) is recommended to significantly reduce the administration of opioid drugs in the context of a MA[21,75,76].Concomitant use of paracetamol and NSAIDs is the main axis of perioperative MA and one of the most important components of ERAS[73,76].Studies have shown that MA has great analgesic effects on moderate pain and reduces the additional use of opioids after TKR and THR[57,77].NSAIDs and COX-2 inhibitors are not recommended for patients with contraindications (allergy, pre-existing kidney disease,etc.)[78].
Optimal intra-operative fluid management
Intravenous fluids and maintenance of normovolemia are very important for perioperative patients.Failure to maintain normovolemia may lead to increased morbidity/mortality, affect tissue oxygenation, increase post-operative cardiopulmonary complications, increase trauma inflammation and prolong hospital stay[17,19,21].Intra-operative isotonic crystalline fluids are administered to preserve homeostasis and the electrolyte balance at a rate of 3-5 mL/kg/h.ERAS society recommends early transition from IV to PO fluid therapy within 24 h for patients undergoing major surgery[79].
Prevention and treatment of PONV
PONV is undoubtedly an unpleasant adverse effect, which is experienced by 20%-30% of surgical patients and 70% of high-risk patients (patients with gastroparesis, esophageal achalasia, dysphagia, neurological diseases, gastrointestinal surgery, Whipple procedure, gastrectomy,etc.)[38].For the prevention and treatment of PONV, it is recommended to administer 4 mg IV infusion of ondansetron before induction of anesthesia and metoclopramide half an hour before awakening.Especially for highrisk patients, a combination of 2-3 antiemetics is recommended.Such a combination may be ondansetron 4mg overnight, dexamethasone 4-5 mg after induction of anesthesia and droperidol 0.625-1.25 mg at the end of surgery[17,19,21,80].Caution is needed in the use of dexamethasone as an antiemetic in oncology patients because of its potential immunosuppressive and hyperglycemic effects[81].A recent study has shown that dexamethasone significantly decreased the incidences of PONV as well as pain, improved respiratory parameters, and reduced the need for additional postoperative analgesic and antiemetic drugs[81].It is worth noting that Ganet al[80] and Sherifet al[82] created a simplified PONV probability scoring system using only four risk factors: (1) Female gender; (2) Previous PONV history; (3) Smoking; and (4) Opioid analgesics[80,82].Therefore, a combination of two drugs is recommended for patients with one or two risk factors, while for patients with more than two factors the recommendation is a combination of three drugs[80,83].Finally, chewing gum post- operatively appears to help mobilize the gastrointestinal system[84].
Normothermia
Hypothermia affects over 60% of patients.Maintaining body temperature at normal levels throughout the surgery has been shown to help reduce post- operative wound infection, intraoperative bleeding, cardiovascular complications, post-operative stress and its metabolic effects[85,86].Prevention of perioperative hypothermia is achieved by using electric hot air devices for the patient's body and fluid heating pumps to administer intravenous fluids or blood products at 37-40 ℃ intraoperatively.The temperature in the operating room should be 21 ℃ for total joint surgeries[19,86-89].
Prophylactic anticoagulant treatment
There is a significant correlation between deep vein thrombosis, pulmonary embolism and hip and knee replacement surgery, which can lead to post- thrombotic syndrome or even death[90].The NICE guidelines recommend early mobilization and fast return to baseline activity[61], as well as low-molecular-weight heparin anticoagulant therapy for 28 d in hip surgeries and 14 d in total knee operations[90-92].
Antimicrobial prophylaxis
One of the most serious and harmful post-operative complications in orthopedic surgery is bone tissue and prosthetic joint infections.Infection after THR or TKR surgery is called osteomyelitis and remains to date the worst complication to treat[21,93].Bone infection treatment often requires removal of the prosthesis in order to reduce osteolysis and inflammation[94-97].Recommendation for prophylactic antimicrobial therapy is 1stor 2ndgeneration cephalosporin (Cefazolin, Cefuroxime) 30-60 min before the skin incision as a single-dose, depending on the patient's weight (weightadjusted dose)[98].
Surgical management
Although there are many comparative studies on surgical techniques and approaches to TKR and THR, we cannot conclude with certainty which technique is superior to all.ERAS society does not recommend a specific surgical technique[16].
ERAS protocols recommend avoiding the use of tourniquets and drains as a routine.It seems that tourniquet does not reduce the total blood loss from surgery, while increasing the risk of thromboembolic events, edema and complications[99-101].Regarding wound drainage, studies show that not only does it not help prevent hematomas, but it also increases the risk of inflammation and blood loss because it eliminates the tamponade effect and may cause a retrograde infection[102-104].
Post-operative analgesia
Effective post-operative pain management includes a combination of analgesic drugs with central and peripheral action, aimed at early mobilization and feeding.Once the patient begins to eat solid food, the IV analgesic regimen should be administeredperos[19,36].In ERAS protocols, MA is very important for pain management, enhanced recovery and patients discharge.MA significantly reduces the opioid requirements and helps reduce PONV, post-operative stress and the risk of complications[16,19].The use of paracetamol in combination with lornoxicam or celecoxib/parecoxib is recommended.Paracetamol is very effective in acute post-operative pain without significant side effects and constitutes a key component of MA in all ERAS guidelines[17,78,105].
Prevention of in-hospital falls after surgery
RA is responsible for in-hospital falls in post-operative patient after TKR and THR.Patients with GA have a higher rate of in-hospital falls compared to NA.The group of PNB has not been significantly associated with patients’ falls[67], while PNB-induced quadriceps insufficiency is not the only cause for in-hospital falls[106].Many factors can contribute to an in-hospital fall after TKR and THR, such as re-operation, advanced age, female gender and comorbidities, which highlights the importance of establishing a multidisciplinary in-hospital fall prevention program in every orthopedic ward[35,107,108].
Multimodal post-operative analgesia, including RA or PNB techniques, in combination with goal-directed rehabilitation are important components that prevent in-hospital falls.This approach accelerates functional recovery and minimizes the risk of in-hospital falls, increases patient satisfaction and reduces overall hospital stay and costs[109,110].
PHYSIOTHERAPY REHABILITATION
Physiotherapy rehabilitation of patients after TKR or THR surgery should begin much earlier than the day of surgery, in the form of counseling.After the physical evaluation, interventions are made to reduce body mass index and increase muscle strength by increasing physical exercise and activity[71,111].The procedure can be started up to 4 wk before scheduled surgery, with regular sessions aimed at early mobilization.Patients are initially informed in detail about the surgery and the postoperative stage even with appropriate leaflets.If possible, patient counseling can be performed simultaneously to a group of people who will undergo surgery on the same day.At the same time, an exercise and stretching program can be implemented to strengthen the muscles of the lower extremities of patients, who learn how to perform it on their own[112,113].
Patients who have followed a counseling program delivered by the physiotherapist, have become more comfortable with the use of walking-aid, made the suggested interventions in the configuration of their residence so that it is safe for a faster return home and have returned home on the 3rd post-operative day without complications[114,115].
The strengthening part is very important because patients who are going to undergo TKR or THR surgery, already have deficient function of the quadriceps due to arthritis or cancer.This is caused by reduced functional use of the joint due to pain and atrophy.Muscle strengthening with progressively increasing resistance and neuromuscular electrical stimulation perioperatively have been shown to improve the functional performance of the quadriceps[116].
Pre-operative mobilization and strengthening seems to be crucial because there is a significant reduction in muscle strength and ability to perform the leg press test within the 1stweek after surgery[117].In fact, the decrease is not due to objective findings (inflammation, swelling) but subjective symptoms (insecurity, pain), which subside to such an extent when applying the pre-operative approach and early mobilization, that patients are discharged earlier and, in some cases, do not need post-operative physiotherapy other than an exercise routine they are trained to perform at home[118,119].
Psychological support of the patients from the interdisciplinary team is necessary, because it increases their sense of security and satisfaction[120].The team reports on the benefits of early mobilization within 8-12 h after the surgery.Even patients who disagree or hesitate to follow the instructions of physiotherapists should at least agree to cooperate.Their initial reluctance is followed by surprise, as they experience less pain than they thought during the recovery period and are satisfied with their postoperative progress[121].
Early mobilization reduces the LOS as patients can be discharged sooner without increasing the risk of complications.Depending on the pain experienced by the patient, he or she may be able to stand or walk without aid on post- operative day 1 if the visual analogue scale score is lower than 5[122].
Pain management, reduced swelling, autonomous movement and normal mobilization with walking-aids are criteria for the patient's discharge from the hospital.Indicatively, following TKR the aim is for the patient to be able to lift their limb with stretched knee and achieve pain-free flexion to 90 degrees, while safe and controlled walking to and from the bed suffices after THR surgery[111,115,122].Postoperatively, standard physiotherapy (kinesiotherapy) as well as other methods, including electrical stimulation, are applied in order to strengthen the muscles, increase the range of motion, reduce swelling and enhance independent gait[123,124].
All of the above ERAS pathways that developed for the rapid postoperative recovery of oncological patients undergoing Total Knee or Hip Reconstruction are summarized in Table 1.
CONCLUSION
ERAS programs undoubtedly reduce hospitalization days without increasing the risk of complications or relapses and reduces hospital costs.These programs require good organization and handling by the multidisciplinary team.Nurses have a central role in the implementation of ERAS programs.ERAS programs increase the patient's sense of satisfaction due to their active participation which they experience as an individualized treatment.However, their implementation is not common practice in Greece, so additional multicenter clinical trials at are required.
杂志排行
World Journal of Orthopedics的其它文章
- Slacklining: A narrative review on the origins, neuromechanical models and therapeutic use
- Off-the-shelf 3D printed titanium cups in primary total hip arthroplasty
- Evidence-based approach to providing informed consent for hip fracture surgery during the COVID-19 era
- Dermatomyositis and polymyositis in total hip arthroplasty
- Outcome and revision rate of uncemented humeral head resurfacing:Mid-term follow-up study
- Trends in leadership at orthopaedic surgery sports medicine fellowships