Effect of preoperative nutrition therapy type and duration on short-time outcomes in gastric cancer patient with gastric outlet obstruction
2021-05-19JiyangLiShaoqingLiHongqingXiPeifaLiuWenquanLiangYunheGaoChuangWangBoWeiLinChenYunTangZhiQiao
Jiyang Li,Shaoqing Li,Hongqing Xi,Peifa Liu,Wenquan Liang,Yunhe Gao,Chuang Wang,Bo Wei,Lin Chen,Yun Tang,Zhi Qiao
1Department of General Surgery,the First Medical Center,Chinese PLA General Hospital,Beijing 100853,China;2Liposuction Center of Plastic Surgery Hospital,Chinese Academy of Medical Sciences and Peking Union Medical College,Beijing 100144,China
Abstract Objective:To avoid perioperative complications caused malnutrition,nutrition therapy is necessary in gastric outlet obstruction (GOO) patients.Compared to parenteral nutrition (PN),enteral nutrition (EN) is associated with many advantages.This study aimed to investigate whether preoperative EN has beneficial clinical effects compared to preoperative PN in gastric cancer patients with GOO undergoing surgery.Methods:According to the methods of preoperative nutrition therapy,143 patients were divided into EN group(n=42) and PN group (n=101) between January 2013 and December 2017 at the Chinese People’s Liberation Army General Hospital.Multiple logistic regression models were used to assess the association between the methods of preoperative nutrition therapy and postoperative day of flatus passage.The generalized additive model and twopiecewise linear regression model were used to calculate the inflection point of the preoperative nutritional therapy time on the postoperative day of flatus passage in the PN group.Results:EN shortened the postoperative day of flatus passage in gastric cancer patients with GOO,which is a protective factor,especially in patients who underwent non-radical operations and the postoperative day of flatus passage reduced when the preoperative PN therapy was up to 3 d and a longer PN therapy (>3 d) did not accelerate the postoperative recovery of gastrointestinal functions.Conclusions:Preoperative EN therapy would benefit gastric cancer patients with GOO by accelerating postoperative recovery.For patients with absolute obstruction,no more than 3-day PN therapy is recommended if patients can tolerate general anesthesia and surgery.
Keywords:Nutrition therapy;gastric cancer;gastric outlet obstruction;enteral nutrition;parenteral nutrition
Introduction
Gastric outlet obstruction (GOO),a mechanical gastric emptying dysfunction,is mainly caused by cancer invasion or scarring after ulcer healing in the distal stomach (1).The main clinical symptoms are abdominal distension and vomiting,which become increasingly severe as the disease progresses and ultimately result in dystrophy,general fatigue,water and electrolyte balance disorders (2,3).Surgical removal of the obstruction is the primary goal of treatment in GOO patients (4).However,edema of the stomach and malnutrition lower the function of immune system,which increases the risk of perioperative complications (2). To avoid complications such as infection,anastomotic leakage,and preoperative decompression of the stomach,nutrition therapy is necessary in these patients (5).
Until recently,parenteral nutrition (PN) was preferred for ileus,dysmotility,and subacute obstruction (considered as intestinal failure) to maintain nutritional support until the underlying disease was corrected (6).However,PN,although effective in delivering nutrients,has serious metabolic complications and catheter-related bloodstream infections (7).Compared to PN,enteral nutrition (EN) is associated with improvements in gastrointestinal mucosal integrity,immune function,tissue repair responses,and less infectious complications.This translated into decreased nosocomial infections,multiorgan failure,mortality,hospital stay,and health-care costs (8-10).
Developments in techniques of enteral access enabled the application of EN over the past decade.Compared with PN,whether EN has protective or deleterious effects on gastric cancer patients with GOO remains controversial.Thus,we aimed to investigate whether preoperative EN had beneficial clinical effects compared with preoperative PN in short-time outcomes in GOO patients received surgical treatment.
Materials and methods
Research objects
Between January 2013 and December 2017,157 patients were diagnosed as having gastric cancer with GOO at the Chinese People’s Liberation Army General Hospital.The inclusion criteria are summarized as:1) had no serious conditions due to which they could not tolerate general anesthesia and surgery;2) were confirmed to have GOO with upper gastrointestinal contrast computed tomography(CT) or gastroscopy;and 3) had undergone surgery for obstruction.Patients were excluded if they received preoperative radiation or chemotherapy.Fourteen patients were excluded from the study because their clinical data were severely incomplete,which finally left 143 gastric cancer patients with GOO who were included in this study.According to the methods of preoperative nutrition therapy,the 143 patients were divided into enteral nutrition group (n=42,EN group) and parenteral nutrition group (n=101,PN group).Ethical approval for the retrospective study was obtained from the Ethical Committee of the Chinese PLA General Hospital.
Treatment and clinical criteria
The total daily energy requirement for each patient was at least 35 kcal/kg.In the EN group,the EN solution(Nutrison,400 g/tin,Abbott Laboratories,Netherlands,United States) was fed through a nasojejunal feeding tube placed under a gastroscope or an X-ray before surgery.The total energy required in the PN group was attained by infusing the total PN.Additional water,electrolytes,intravenous vitamins,and trace elements were administered as needed.The nutritional risk screening (NRS) was assessed according to the NRS-2002 of the European Society of Parenteral Enteral Nutrition (11). The nutritional statuses were expressed by hemachrome (HB),total protein (TP),and albumin (ALB) levels.The surgical methods included distal gastrectomy,radical total gastrectomy,gastrojejunostomy,and jejunostomy.The reconstruction methods included Billroth I,Billroth II,and Roux-en-Y.The primary outcome was the postoperative day of flatus passage,and secondary outcomes were the postoperative day of drainage and postoperative hospital stay. Postoperative complications including duodenal stump fistula,anastomotic leakage or stenosis,gastric retention,intestinal paralysis,postoperative hemorrhage,pancreatic leakage,pleural or peritoneal effusion,pyothorax,pyocelia,upper respiratory infection,central venous catheter-associated infection,hypoalbuminemia,arrhythmia,bacteremia,fungal infection,hypokalemia or hyperkalemia,phlebitis and skin rash were also recorded.
Statistical analysis
Continuous variables were expressed as,and normality of the distribution was checked using the Mann-Whitney U test and compared using an analysis of variance (Student’st-test or Mann-Whitney U test).Binomial and categorical data were evaluated using a Pearson’s χ2or a two-tailed Fisher’s exact test.Non-adjusted and adjusted multiple logistic regression models were used to assess the association between the methods of preoperative nutrition therapy and postoperative day of flatus passage.Covariates were considered in the adjusted model if the matched odds ratio changed by at least 10% as a result of adding those covariates (12).Next,non-linear relationship analyses were performed by a generalized additive model to determine the correlation between preoperative nutritional therapy time and postoperative day of flatus passage in the two groups. We further applied a two-piecewise linear regression model to calculate the inflection point of the preoperative nutritional therapy time on the postoperative day of flatus passage in the PN group.All analyses were performed using the statistical software package R(http://www.R-project.org; The R Foundation for Statistical Computing,Vienna,Austria) and Empower States (http://www.empowerstates.com;X &Y Solutions,Inc.,Boston,MA,USA).The 95% confidence interval(95% CI) was calculated for intergroup differences,and P values less than 0.05 (two-sided) were considered statistically significant.
Results
No thirty-day mortality occurred in either group.Demographic and clinical characteristics and surgical factors are summarized inTable 1.There was no significant difference in age,sex,body mass index (BMI),NRS score and diabetes between the two groups.The duration of inability to eat solid food was significantly longer in PN group than in EN group (10.0 dvs.5.5 d,P<0.001).The preoperative nutritional therapy time was longer in PN group than in EN group (6.73 dvs.5.95 d,P=0.031).
The tumor size and location,lymph node metastasis (N stage),distant metastasis (M stage),preoperative and postoperative HB,TP,and ALB of the two groups were not significantly different.Patients in PN group had more tumors of ulcerative type (47.78%vs.21.95%,P=0.031)and moderate differentiation (29.17%vs.7.14%,P=0.022)than those in EN group;however,patients in EN group had more tumors of T4a stage (90.48%vs.53.76%,P<0.001) than those in PN group (Table 2).The surgical treatments were similar in the two groups,including the percentage of radical and minimally invasive operations,surgical methods,reconstruction methods,estimated blood loss,and intraoperative transfusion of red blood cell or plasma.
Postoperative outcomes
The EN group had significantly shorter first flatus time than the PN group (3.79 dvs.4.74 d,P<0.001);however,the pull nasogastric tube and drainage time were similar in the two groups.Postoperative complications were not significantly different between the two groups.The postoperative treatment time and hospital stay of EN group were shorter than those of PN group;however,the differences were not statistically significant.The difference in the total hospitalization costs between the two groups was not statistically significant (Table 2).
Effect of preoperative PN and EN on postoperative day of flatus passage
The univariable analyses showed that the method of preoperative nutrition therapy (EN or PN),diabetes,duration of inability to eat solid food,and percentage of radical operation were correlated with the postoperativeday of flatus passage (P<0.05) (Table 3).The relationship between the preoperative PN or EN and postoperative day of passage in the different models is presented inTable 4.In the crude model,EN showed a negative correlation with the postoperative day of flatus passage (β=-0.96,95% CI:-1.49 to -0.43,P<0.001).In the minimally adjusted model(adjusted preoperative nutritional therapy time,diabetes,and T stage),the result did not have any obvious changes(β=-0.65,95% CI:-1.18 to -0.11,P=0.020).However,when we fully adjusted the model using preoperative nutritional therapy time,diabetes,Bormmann type,degree of histologic differentiation,T stage,N stage,complication,and radical operation,we did not detect the correlation (β=-0.30,95% CI:-0.83 to 0.22,P=0.256).
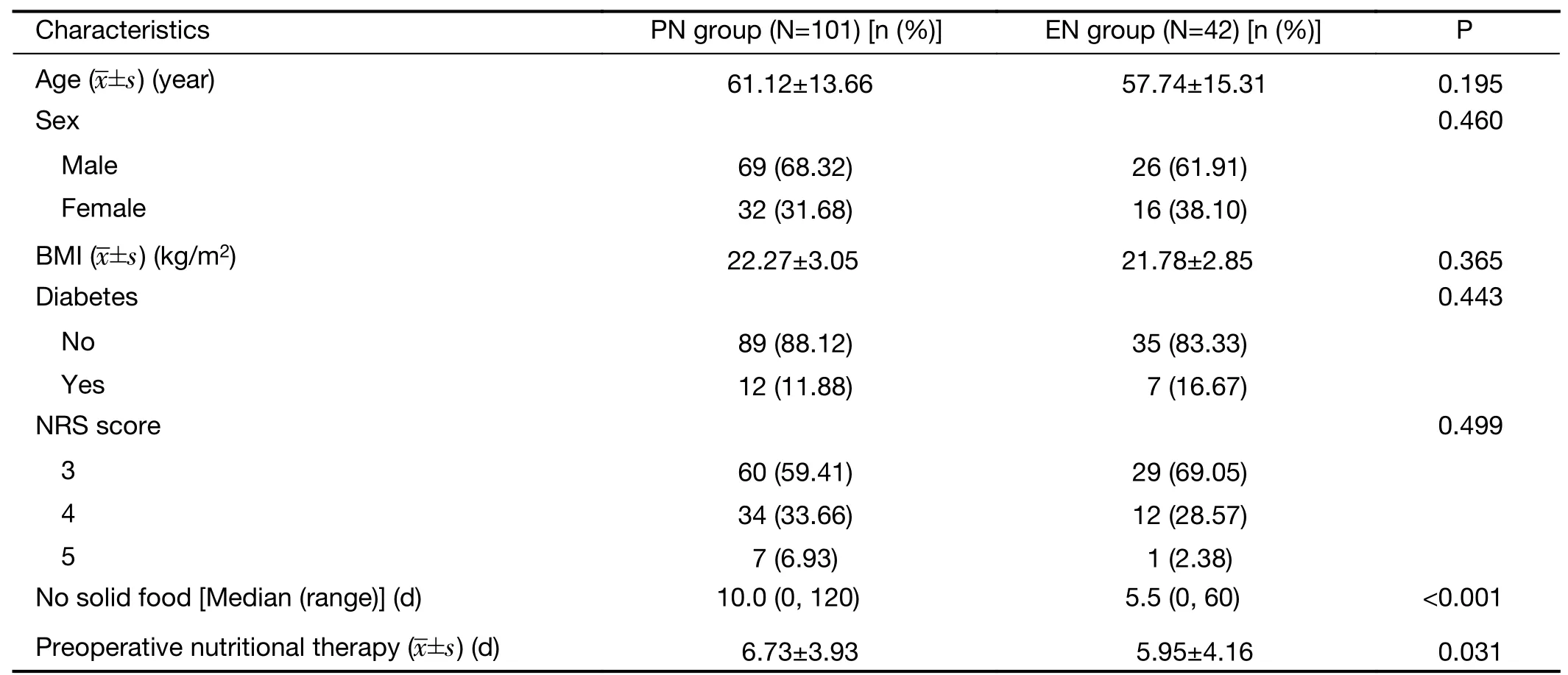
Table 1 Preoperative characteristics of patients in PN group and EN group

Table 2 Clinicopathological characteristics,treatment information and postoperative outcomes

Table 2 (continued)
Effect of preoperative nutritional therapy time on postoperative day of flatus passage in PN group
As the preoperative nutritional therapy time was a continuous variable,an analysis of the non-linearrelationship could be conducted.As shown inFigure 1A,a threshold non-linear association between the preoperative nutritional therapy time and postoperative day of flatus passage was found by a generalized additive model in PN group (P=0.022),but not in EN group (P=0.545).Additionally,by the two-piecewise linear regression model,we calculated that the inflection point was 3 in PN group.On the left of the inflection point,the effect size (β),95% CI and P value were -1.61,-3.10 to -0.11,and 0.038,respectively.However,we observed no relationship between the preoperative nutritional therapy time and postoperative day of flatus passage to the right of the inflection point (-0.02,-0.09 to 0.06,P=0.689) (Table 5,Figure 1B).This indicated that the postoperative day of flatus passage reduced when the preoperative PN therapy was up to 3 d and that a longer PN therapy (>3 d) did not accelerate the postoperative recovery of gastrointestinal functions.

Table 3 Univariate analysis for postoperative day of flatus passage
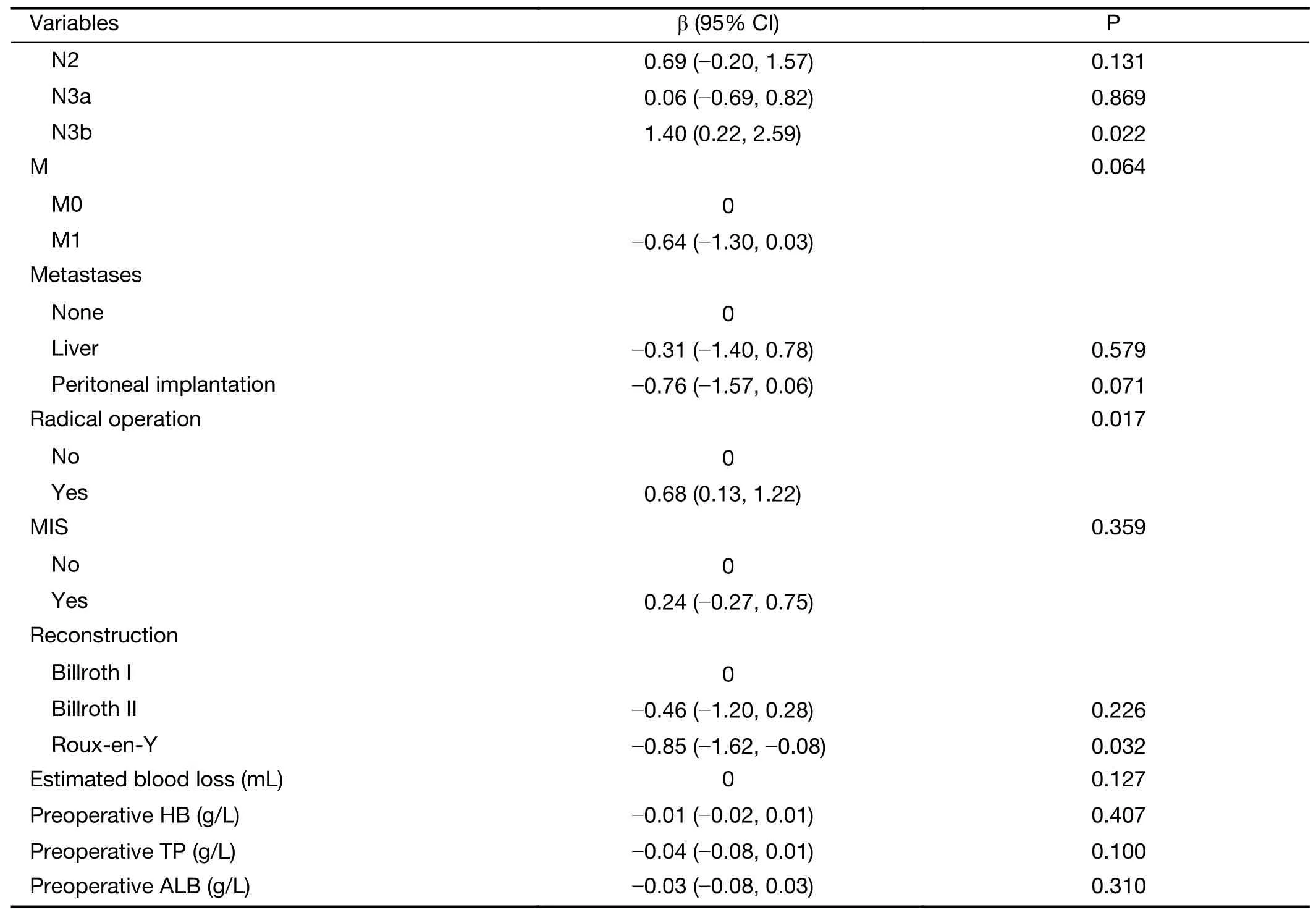
Table 3 (continued)
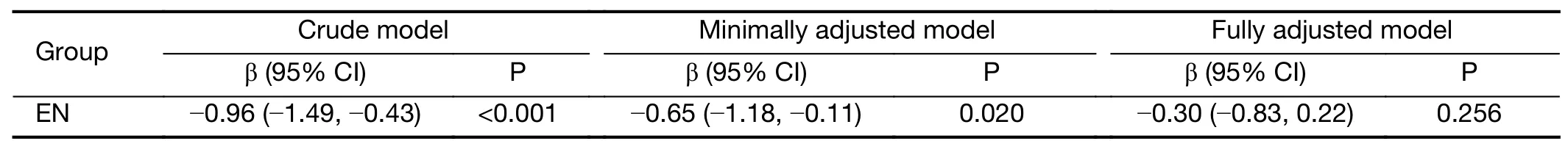
Table 4 Relationship between preoperative PN or EN and postoperative day of flatus passage in different models
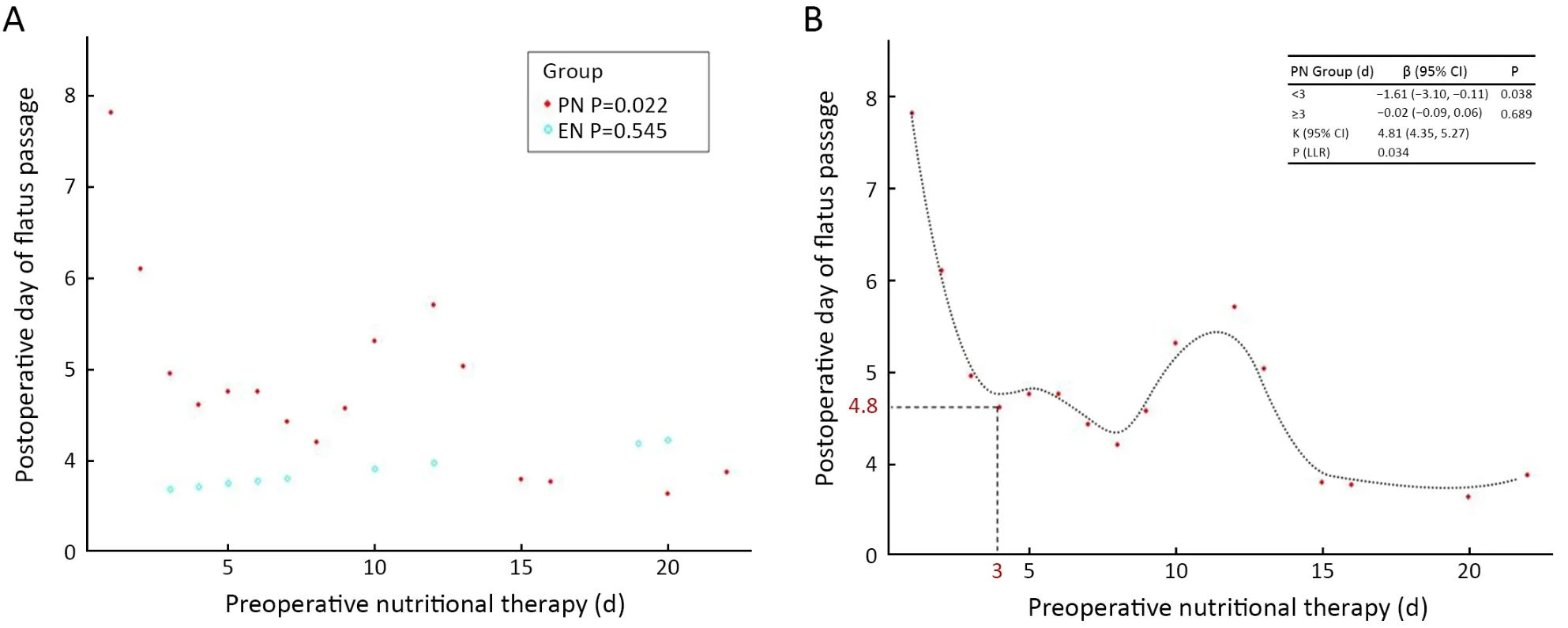
Figure 1 Effect of preoperative nutritional therapy time on postoperative day of flatus passage in PN group.(A) A threshold,non-linear association between the preoperative nutritional therapy time and postoperative day of flatus passage found by a generalized additive model in PN group (P=0.022) but not in EN group (P=0.545);(B) Two-piecewise linear regression model showing that the inflection point was 3 in PN group.When patients received preoperative PN treatment for 3 d,the postoperative day of flatus passage reached a relatively low value,4.8 d.PN,parenteral nutrition;EN,enteral nutrition;β,effect size;95% CI,95% confidence interval.

Table 5 Results of two-piecewise linear regression model
Subgroup analysis
As shown inTable 6,the test for interactions was significant for radical operations (P for interaction was 0.026).The odds ratio of preoperative nutritional therapy type on the postoperative day of flatus passage was larger in patients who did not undergo radical operation (-1.06,-2.02 to-0.10,P=0.037) than in those who underwent radical operation (-0.84,-1.47 to -0.22,P=0.010).This indicated that EN was a more effective protect factor for non-radical operations.The test for interactions was not statistically significant for other factors (Supplementary Table S1,S2).
Discussion
This study suggests that: 1) EN shortened the postoperative day of flatus passage in gastric cancer patients with GOO,which is a protective factor,especially in patients who underwent non-radical operations and 2) the postoperative day of flatus passage reduced when the preoperative PN therapy was up to 3 d and a longer PN therapy (>3 d) did not accelerate the postoperative recovery of gastrointestinal functions.
Persistent vomiting,resulting in an excessive loss of digestive juices and difficulty absorbing nutrients,can lead to dehydration and electrolyte imbalance in the body.Previous reports have shown that the direct cause of death in >20% of patients with tumors is malnutrition (13).Surgery is an important intervention for the treatment of gastric cancer with GOO,with symptom remission rates as high as 72% (14).For patients undergoing surgery,preoperative malnutrition not only weakens muscle activity and the immune system,delays healing of incisions (15),and directly affects postoperative recovery and prognosis but also delays the best opportunity for gastric cancer patients with GOO to receive postoperative chemotherapy(16,17).
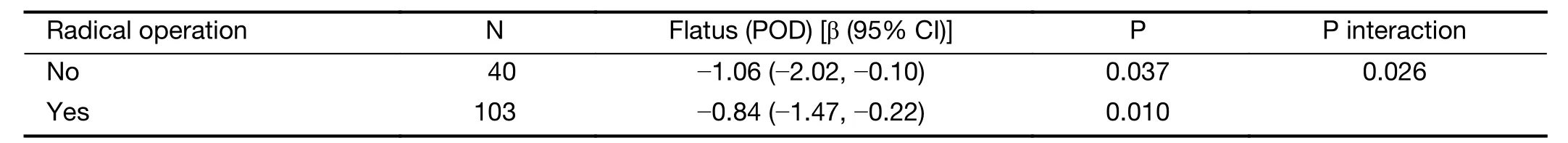
Table 6 Interaction of different preoperative nutritional therapy type (PN vs.EN) on postoperative day of flatus passage in prespecified and exploratory subgroups in each subgroup
Therefore,most GOO patients need peri-operation nutrition therapy.PN has been an indispensable nutrition treatment for these patients,but lack of enteral feeding significantly increases infectious complications (18).EN can support patients with a variety of amino acid digestion and absorption problems,improve protein utilization to accelerate wound healing,activate the gastrointestinal nerve endocrine system,promote intestinal peristalsis,accelerate nutrient absorption,improve intestinal physiological and ecological balance,and protect the intestinal mucosa to maintain normal gastrointestinal tract functions and avoid intestinal mucosal atrophy and intestinal bacterial translocation,which cause ectopic perioperative infections.Maintenance of the gut barrier is key to preventing severe insult-induced systemic inflammation and infection (19,20).
Similar to our results,Dinget al.proved that preoperative EN improved postoperative nutritional status and immune function,alleviated inflammatory response,and facilitated recovery for gastric cancer patients (21).Recently,novel modified techniques of enteral access have shown high success rates,low complication rates,and provided the benefits of minimal invasion even in patients with GOO (22-24).Endoscopic guidance and radiology help to traverse a compressed segment to deliver nutrients directly to the functional distal bowel (25).EN therapy is safe,effective,economical,and convenient,and has a wide range of applications in clinics (26,27).
PN is a necessary treatment for malnourished patients with absolute obstruction and may also prove useful to“top-up”nutrition in patients who cannot tolerate sufficient intake via the enteral route (28).Our study also assessed the length of preoperative PN therapy and found that after 3 d of preoperative PN treatment,the postoperative day of flatus passage reached to a relatively low value,4.8 d.With the prolongation of preoperative PN treatment,there is no association with time of postoperative flatus passage.Therefore,we propose that once patients can tolerate general anesthesia and surgery,there is no need to prolong the perioperative PN therapy.
The study is limited by its retrospective design and nonrandomized grouping.Another limitation is that the sample size was relatively small.Therefore,large-scale samples from multiple centers are required to confirm our findings.
Conclusions
Preoperative EN therapy would benefit gastric cancer patients with GOO by accelerating postoperative recovery.For patients with absolute obstruction,no more than 3-day PN therapy is recommended if patients can tolerate general anesthesia and surgery.
Acknowledgements
This work was funded by the Special Funding for Clinical Research of Wu Jieping Medical Foundation (No.320.2710.1848),the Clinical Research Supporting Project of PLA Genenral Hospital (No.109310),and the Beijing Municipal Science and Technology Project (No.D171100006517002 and No.D171100006517004).
Footnote
Conflicts of Interest:The authors have no conflicts of interest to declare.
杂志排行
Chinese Journal of Cancer Research的其它文章
- Landscape of cell heterogeneity and evolutionary trajectory in ulcerative colitis-associated colon cancer revealed by single-cell RNA sequencing
- Combined detection and subclass characteristics analysis of CTCs and CTECs by SE-iFISH in ovarian cancer
- Multicenter phase II study of apatinib single or combination therapy in HER2-negative breast cancer involving chest wall metastasis
- Novel therapies targeting hypoxia mechanism to treat pancreatic cancer
- Laparoscopic surgery for gastric cancer:Current status and future direction
- Clinical challenges in neoadjuvant immunotherapy for non-small cell lung cancer