Acute cardiogenic liver injury caused by heart failure in an adolescent
2021-05-19ChunHongXieJieShenQingZhangJianHuFangQiGong
Chun-Hong Xie,Jie Shen,Qing Zhang,Jian Hu,Fang-Qi Gong
Department of Cardiology, Children’s Hospital, Zhejiang University School of Medicine, National Clinical Research Center for Child Health, Hangzhou 310052,China
TotheEditor:
Heart failure is a systemic clinical syndrome characterized by multiple organ systems involvements [1].With the progression of heart failure,patients may present with liver-related symptoms.However,these symptoms may be misdiagnosed as primary gastrointestinal diseases which lead to treatment delay and aggravation of conditions.We retrospectively reviewed the liver function changes in an adolescent with heart failure,which will help clinicians better understand acute cardiogenic liver injury.
A 13-year-old girl was admitted to a local hospital because of cough for longer than 10 days and chest pain for 3 days.On admission,she also had shortness of breath when climbing stairs and could be relieved after rest.She complained of decreased appetite and vomiting.Physical examination showed edema in the lower limbs.Chest computed tomography (CT) showed multiple infiltrates,right pleural effusion and cardiomegaly.Cardiac ultrasound revealed enlargement of the entire heart,an atrial septal defect,moderate mitral valve and tricuspid valve regurgitations and pulmonary hypertension.Her left ventricular ejection fraction (LVEF)was 17%.Primary diagnosis in the local hospital is pneumonia and cardiomyopathy.She was administered with cefotaxime and cimetidine,however,her conditions exacerbated after one day of treatment.She was then referred to our hospital.
On admission to our hospital,her heart rate was 134 bpm and respiratory rate was 28 bpm.Past medical history enquiry revealed that she had congenital absence of the right kidney.Physical examination revealed moist rales in both lungs.The liver was enlarged about 1 cm below the right costal margin with medium tenderness.Pitting edema was found in the lower limbs.Blood tests revealed increased brain natriuretic peptide of 9430 pg/mL (reference:<135 pg/mL).Electrocardiogram showed sinus tachycardia,left atrial enlargement,low limb lead voltage and ST-T wave alteration.Chest X-ray showed increased pulmonary blood volume and cardiomegaly.Abdominal ultrasound showed sediment deposits in the gallbladder,right kidney absence and left kidney enlargement.Cardiac ultrasound in our hospital revealed an LVEF of 15% and a secundum atrial septal defect (diameter:4 mm),minor mitral valve,tricuspid valve and pulmonary valve regurgitations.She was diagnosed with dilated cardiomyopathy,chronic heart failure,pleural effusion,atrial septal defect,acute pneumonia and right kidney absence.
Continuous intravenous vitamin C,milrinone,fructose sodium diphosphate oral solution,hydrochlorothiazide,spironolactone,captopril and digoxin were administered for treating heart failure.Intravenous ceftriaxone was given for 5 days to control infection.Ten days later,she was discharged with symptoms improved.Fructose sodium diphosphate oral solution,hydrochlorothiazide,spironolactone,captopril,propranolol,coenzyme Q10 and digoxin were prescribed for her after her discharge.During the follow-up,she complained of occasional shortness of breath and fatigue.Five months later,conditions got worse.She had recurrent attacks of chest distress,abdominal pain,vomiting,shortness of breath,fatigue and paleness without any fever or cough.She was admitted several times to our hospital because of acute onset of chronic heart failure.Physical examination revealed puffiness,pitting edema in the lower limbs,low cardiac sound,liver enlargement for about 4 cm below the right costal margin,moist rales in both lung bases,significant cardiomegaly and 2/6 systolic murmur in cardiac apex.Blood tests revealed increased brain natriuretic peptide of more than 350 0 0 pg/mL.Liver function tests showed significantly increased serum alanine aminotransferase (ALT) and aspartate aminotransferase (AST) levels in the past six months.The highest levels for ALT and AST were 634 U/L and 698 U/L,respectively (reference:<50 U/L for ALT and 15–60 U/L for AST).LVEF was about 20% −30%.Acute cardiogenic liver injury was diagnosed.Fluid restriction,diuresis and milrinone were given for treating acute cardiogenic liver injury.Her liver function improved after treatment and then she was referred to another hospital for heart transplantation.
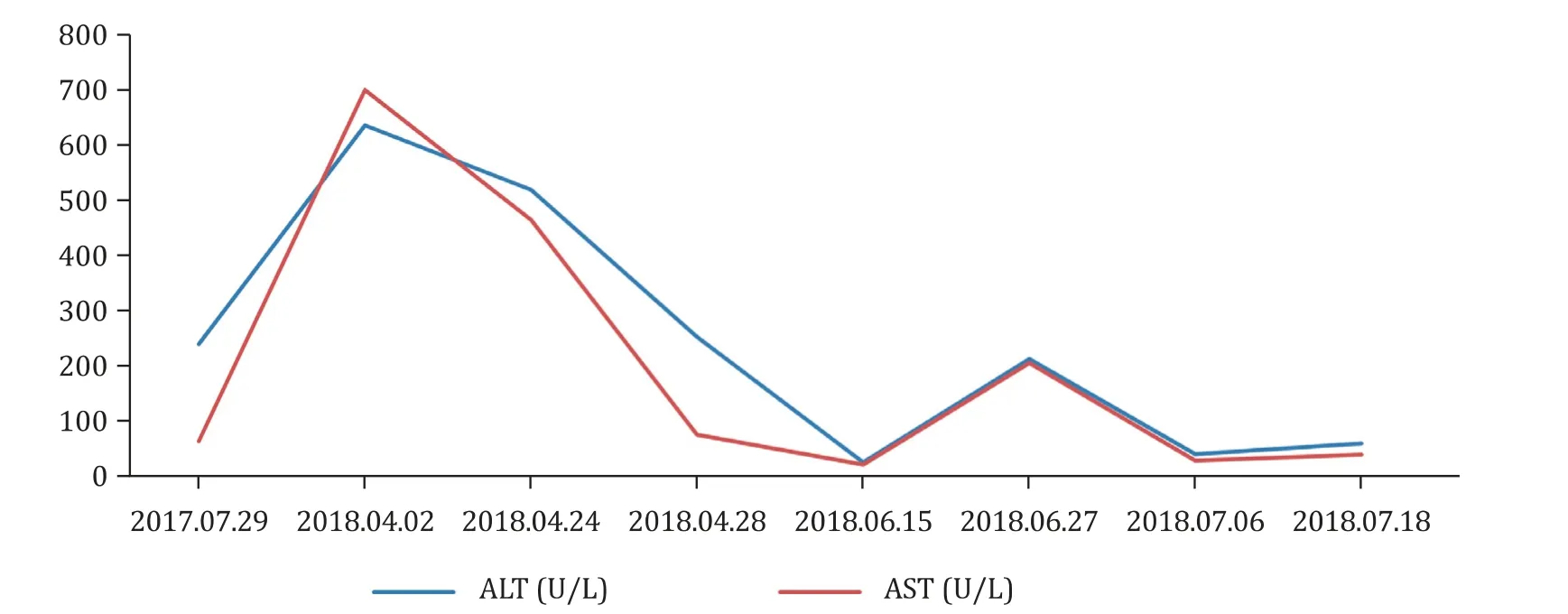
Fig.1.Serum alanine aminotransferase (ALT) and aspartate aminotransferase (AST) levels significantly increased after aggravation of acute onset of chronic heart failure.
Heart failure is a major public health problem,with frequent hospitalizations,impaired quality of life,and shortened life expectancy.In the United States,11,0 0 0–14,0 0 0 children are admitted with heart failure annually,with a high hospital mortality (7.4%)compared with 0.4% in those without heart failure [2].Because of heart failure,the heart cannot deliver oxygen at a rate proportionate to the demands of the metabolizing tissues that may result in damage to other organs such as the kidney,bone marrow,or liver [ 3,4 ].Abnormalities in liver function tests are common findings in patients with heart failure.Chronic liver damage secondary to heart failure has its distinct features [5].The changes of the livers are caused by hepatic venous congestion,often called“congestive hepatopathy”,resulting from increased central venous pressure due to prolonged right heart failure (sometimes referred to as“backward failure”),which can occur in congestive heart failure,congenital heart disease,and corpulmonale,among others [6].Although there is no consensus on terminology,“cardiac hepatopathy”has generally been used to describe any liver damage caused by cardiac disorders in the absence of other possible causes of liver damage.The primary pathophysiology of cardiac hepatopathy is either“congestive hepatopathy”caused by passive venous congestion or“acute cardiogenic liver injury”caused by low cardiac output and arterial hypoperfusion [3].The typical laboratory finding of acute cardiogenic liver injury is the presence of a striking elevation in aminotransferases and lactate dehydrogenase levels (generally to 10–20 times of the normal values,even up to 20 0 0 folds).Aminotransferases and lactate dehydrogenase levels reach their peak 1–3 days after the acute event and return to normal limits within 7–10 days if the patient’s hemodynamics recover [3].In our case,ALT and AST significantly increased after aggravation of acute onset of chronic heart failure (Fig.1).Liver function can be improved after improving hemodynamics by fluid restriction,diuresis and milrinone.In our case,the causes of toxin,chemicals or virus-related liver damage was excluded.The recognition and understanding of liver lesions in heart failure is essential for the treatment and prognosis.Diuretics are mainly used to manage the signs and symptoms of congestion and may improve clinical outcomes.However,if the ischemic symptoms are dominant,inotropics such as phosphodiesterase inhibitor (milrinone) could be administered to increase the perfusion and oxygenation.
Liver function test is a simple and convenient examination.In case of abnormality,the treatment plan of heart failure should be adjusted and intervention should be carried out as soon as possible to avoid aggravation of heart failure and poor prognosis,so as to reduce the readmission rate and mortality.Improving organ function before transplantation is also important for reducing perioperative complications and improving postoperative survival.
Acknowledgments
None.
CRediT authorship contribution statement
Chun-Hong Xie:Conceptualization,Writing -original draft.Jie Shen:Conceptualization,Writing -original draft.Qing Zhang:Data curation.Jian Hu:Data curation.Fang-Qi Gong:Conceptualization,Writing -review &editing.
Funding
None.
Ethical approval
This study was approved by the Ethics Committee of Children’s Hospital,Zhejiang University School of Medicine (2020-IRB-127).Informed consent for publication was obtained from the parents of the case.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Practice of precision surgery in primary liver cancer
- Reporting of longitudinal pancreatojejunostomy with partial pancreatic head resection (the Frey procedure) for chronic pancreatitis:A systematic review
- Hepatobiliary&Pancreatic Diseases International
- Presentation and surgical management of xanthogranulomatous cholecystitis
- Transjugular intrahepatic portosystemic shunt is effective in patients with chronic portal vein thrombosis and variceal bleeding
- Long-term follow-up of HCV patients with sustained virological response after treatment with pegylated interferon plus ribavirin