Reporting of longitudinal pancreatojejunostomy with partial pancreatic head resection (the Frey procedure) for chronic pancreatitis:A systematic review
2021-05-19MinsBlttzisSnthlingmJegtheeswrnAjithSiriwrden
Mins Blttzis ,Snthlingm Jegtheeswrn ,Ajith K Siriwrden ,
a Regional Hepato-Pancreato-Biliary Surgery Unit, Manchester Royal Infirmary, Oxford Road, Manchester M13 9WL, UK
b Faculty of Biology, Medicine and Health, University of Manchester, Manchester, UK
Keywords:Chronic pancreatitis Frey procedure Reporting Longitudinal pancreatojejunostomy
ABSTRACT Background: Longitudinal pancreatojejunostomy with partial pancreatic head resection (the Frey procedure) is accepted for surgical treatment of painful chronic pancreatitis.However,conduct and reporting are not standardized and thus,making comparisons difficult.This study assesses the reporting standards of this procedure.Data sources: A systematic literature review was performed between January 1987 and January 2020.The keyword and Medical Subject Heading“chronic pancreatitis”was used together with the individual operation term“Frey pancreatojejunostomy”.Reports were included if they provided original information on conduct and outcome.Thirty-three papers providing information on 1205 patients constituted the study population.Risk of bias in included reports was assessed.Results: Etiology of chronic pancreatitis (alcohol) was reported in 26 of 28 (93%) studies,duration of symptoms prior to surgery in 19 (58%) studies and pre-operative opiate use in 12 (36%) studies.In terms of morphology,pancreatic duct diameter was reported in 17 (52%) studies and diameter of the pancreatic head in 13 (39%) studies.In terms of technique,three (9%) studies reported weight of excised parenchyma.There were 9 (0.7%) procedure-related deaths.Post-operative follow-up ranged from 6 to 82.5 months.No studies reported post-operative portal hypertension.Conclusions: There is substantial heterogeneity between studies in reporting of clinical baseline,morphology of the diseased pancreas,operative detail and outcome after longitudinal pancreatojejunostomy with partial pancreatic head resection.This critically compromises the comparison between centers and between surgeons.Structured reporting is necessary for clinicians to assess choice of procedure and for patients to make informed choices when seeking treatment for painful chronic pancreatitis.
Introduction
In 1987 Frey and Smith reported a new operation for treatment of painful chronic pancreatitis [1].The procedure comprised two components:1) the main pancreatic duct in the body and tail of the pancreas was opened longitudinally and drained into a Roux loop of jejunum.This is the longitudinal pancreatojejunostomy reported by Partington and Rochelle [2];2) the pancreatic parenchyma in the head of the gland was“cored”out leaving a rim of pancreatic tissue along the inner aspect of the duodenum–partial pancreatic head resection [1].Frey and Smith’s report acknowledged that the second component of their procedure derived from the contemporaneously reported duodenum-preserving pancreatic head resection (DPPHR;Beger procedure) [ 1,3 ].The Frey and Smith operation differed from the original description of the Beger procedure in three aspects.Firstly,the Frey and Smith operation undertook a longitudinal pancreatojejunostomy which was not a component of the initial report of the duodenum-preserving pancreatic head resection;secondly,the Frey and Smith operation avoided transection of the neck of the pancreas [4];and thirdly,difference in the extent of removal of pancreatic parenchyma from the head of the gland:the Beger procedure undertook a subtotal pancreatic head removal whereas the Frey and Smith operation was a partial pancreatic head resection.

Fig.1.PRISMA flowchart.
Since the publication of Frey and Smith procedure,it has been widely adopted and reported [ 5,6 ].With hindsight,although the extent of partial pancreatic head resection is clearly reported in Frey and Smith’s original paper,subsequent dissemination of the technique has not required adoption of a standard operative approach.As the procedure“cores out”the pancreatic head,descriptions of the operation incorporating various amounts of head resection have been described.It is also not clear whether there is an optimal extent of“coring”of the pancreatic head or whether the procedure is effective because the parenchymal resection in the head decompresses the main duct.
In order to improve the quality of description of surgery for chronic pancreatitis,the International Study Group for Pancreatic Surgery (ISGPS) recently published standards for reporting on surgery for chronic pancreatitis [7].The eponymous term“Frey procedure”was replaced by the anatomical descriptive term“longitudinal pancreatojejunostomy with partial pancreatic head resection”[7].The aim of this report is to assess standards of reporting of the longitudinal pancreatojejunostomy with partial head resection with specific reference to the reported clinical baseline at the time of surgery,the morphology of the diseased gland,operative detail including extent of pancreatic parenchymal resection and outcome.The data will provide what is thought to be the first comprehensive assessment of the reporting of this procedure.This should lead to better standardization of reporting of this important operative procedure.
Methods
Information sources
A systematic review of the literature was performed using the Scopus database for publications between January 1987 and January 2020.The Scopus database was selected as it provides broader coverage of publications than other search databases.The search was cross-checked with PubMed and Embase databases and no additional articles were retrieved.The keyword and Medical Subject Heading“chronic pancreatitis”was used together with the individual operation term“Frey pancreatojejunostomy”.The search yielded 83 records.The PRISMA flowchart of the search strategy is shown in Fig.1 .A PRISMA checklist is provided in Table S1.Inclusion criteria were manuscripts providing original information on the conduct and outcome of the longitudinal pancreatojejunostomy with partial pancreatic head resection.Papers were excluded if they were case reports,reviews without original information and were not in English.After removing irrelevant articles,42 unique citations were screened for eligibility and 36 papers met the inclusion criteria.Three reports were further excluded as they were either long-term or early reports of substantially the same patient groups as other reports in the series.In each case,the report providing the most data was retained.Thirty-three reports constitute the final dataset.
Data extraction and synthesis of results
Data were extracted independently by two authors (Baltatzis M and Jegatheeswaran S).Data were extracted in compliance with the current reporting standards for surgery for chronic pancreatitis [7].First,information was sought on clinical baseline at the time of surgery.This included information on the etiology of chronic pancreatitis,median duration of symptoms,opiate use prior to surgery,diabetes mellitus prior to surgery and whether or not there had been an elective surgical intervention on the pancreas prior to the longitudinal pancreatojejunostomy with partial pancreatic head resection.Second,information was sought on reported morphology of the diseased gland.This included information on the maximum diameter of the main pancreatic duct,the antero-posterior diameter of the pancreatic head,whether or not the main portal veinwas patent prior to surgery and information on the presence of a concomitant biliary stricture or duodenal stricture.Third,information was collected on reported technical conduct of the operation including weight of excised pancreatic parenchyma and the use of concomitant biliary bypass and/or gastrojejunostomy.Finally,data were sought on reported outcome.Specific information was sought on re-operation,operative mortality,follow-up,post-operative diabetes mellitus,post-operative opiate use and post-operative portal hypertension.

Table 1 Clinical baseline in patients undergoing longitudinal pancreatojejunostomy with partial pancreatic head resection.
Assessment of risk of bias in individual studies
The risk of bias was assessed using the Cochrane collaboration’s tool for assessing risk of bias in non-randomized studies of interventions [8].
Ethics assessment
The NHS Health Research Authority (HRA) questionnaire(http://www.hra-decisiontools.org.uk/research/ ;accessed 20th March 2020) was consulted to assess whether this study should be regarded as research.The NHS HRA deemed that this study was not research as the participants were not randomized to different groups,there was no change in treatment or patient care and the findings could not be regarded as wholly generalizable [9].
Results
Final study population
The final dataset provides information on 1205 patients with a median of 33 (range:6-141) cases per report (Table 1) [10–42].
Reporting of clinical baseline in patients undergoing longitudinal pancreatojejunostomy with partial pancreatic head resection ( Table 1 )
Etiology of chronic pancreatitis (alcohol) was reported in 26 of 28 (93%) studies.Alcohol-induced chronic pancreatitis was the most common etiological agent in adult populations.Duration of symptoms prior to surgery was reported in 19 (58%) studies.Of those studies which reported delay from onset of symptoms to surgery,the median delay was 60 months.Opiate use prior to surgery was reported in 12 (36%) studies.Twenty-seven (82%)studies reported diabetes mellitus status prior to surgery.Of these,30% of patients had diabetes mellitus prior to surgery.Prior surgical intervention was reported in 11 (33%) studies with 3 (9%)further reporting that there had been no surgery on the pancreas prior to intervention.
Reporting of morphology of the diseased gland ( Table 2 )
Main pancreatic duct diameter was reported in 17 (52%) studies.In all series in adult patients,the median main duct diameterwas greater than 5 mm.Antero-posterior diameter of the pancreatic head was reported in 13 (39%) studies.Patency of the main portal vein was discretely reported in three (9%) studies.The presence of a concomitant extra-hepatic biliary stricture was reported in 22 (64%) studies while a concomitant duodenal stricture was reported in 12 (36%) studies.
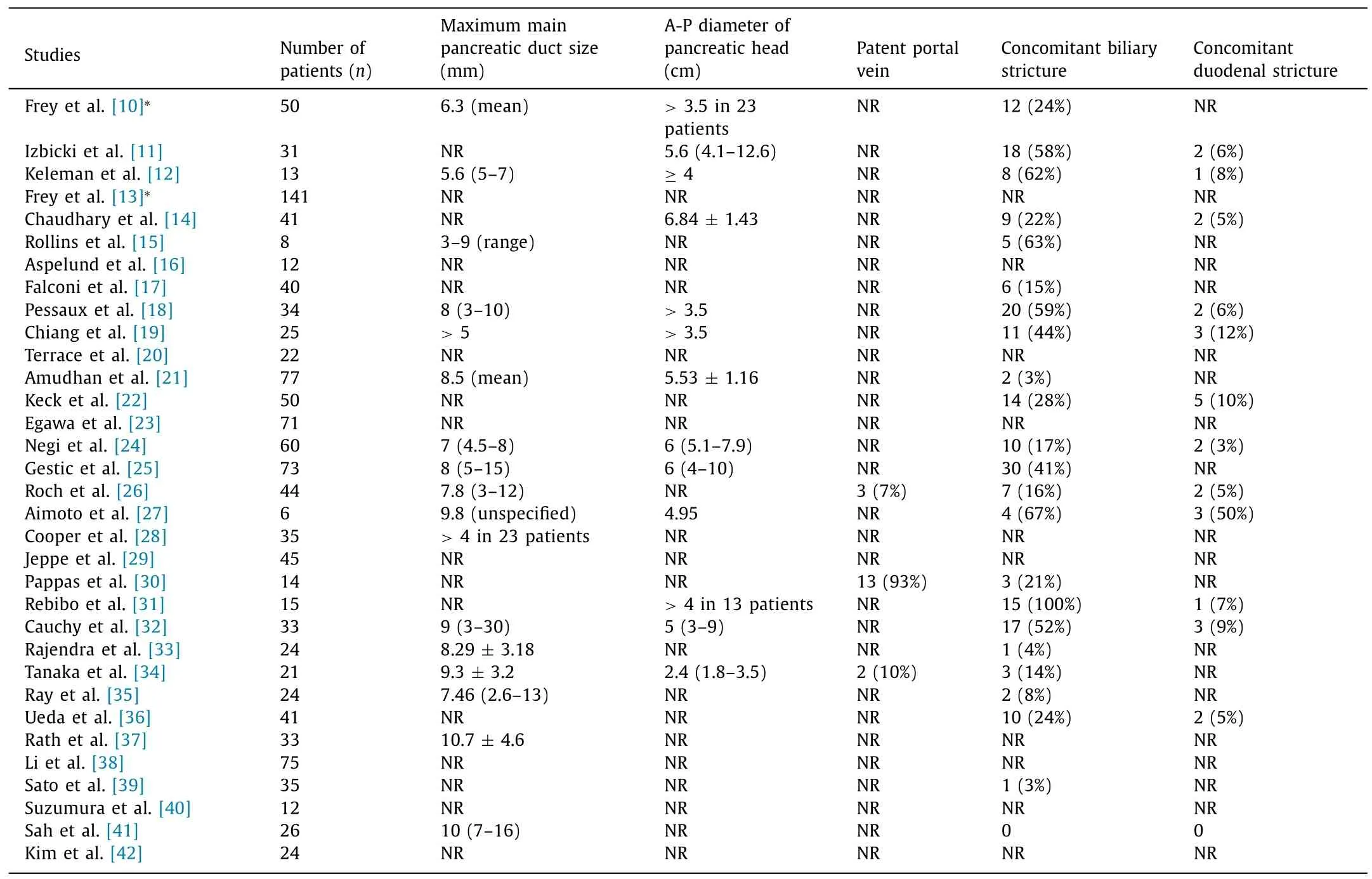
Table 2 Pancreatic gland morphology in patients undergoing longitudinal pancreatojejunostomy with partial head resection.
Reporting of operative detail ( Table 3 )
Three (9%) studies reported the weight of excised pancreatic parenchyma in all patients,which was 5.7 (2–11) g,14.8 (7–78)g and 24 (17–36) g,respectively.Fourteen (42%) studies reported on the use of concomitant biliary bypass.Utilization of biliary bypass during longitudinal pancreatojejunostomy with partial head resection in those studies reporting this ranged from 0 to 80%.Five studies (15%) reported on concomitant gastrojejunostomy with six(18%) further categorically reporting no requirement for gastric bypass at the time of surgery.
Reporting of outcome ( Table 4 )
There were 9 (0.7%) procedure-related deaths.Post-operative follow-up ranged from 6 to 82.5 months.Twenty-four (73%) studies reported on post-operative diabetes mellitus.Ten (30%) studies reported on post-operative opiate use.No studies reported occurrence of post-operative portal hypertension.
Risk of bias
Data were likely to be influenced by both sample and case selection bias as indications for surgery and choice of specific procedure (longitudinal pancreatojejunostomy with head coring) were not available.Data were also likely to be influenced by reporting bias as procedure and outcome reporting was incomplete.A ROBINS-I chart illustrating risk of bias in non-randomized studies is provided in Supplementary material [43].
Discussion
To the best of our knowledge,this is the first study to assess the standards of reporting of the longitudinal pancreatojejunostomy with partial pancreatic head resection.As with all reports based on summation of case cohort series,data are likely to be influenced by multiple sources of bias and this limitation should be borne in mind when interpreting the results [43].
What then does this study add to knowledge? First,it is generally accepted that the outcome of the procedure will be influenced by the baseline condition at the time of surgery [44].In this regard,reporting of etiology (alcohol) was present in 26 (93%) of 28 studies.Given that there is evidence to suggest that duration of symptoms prior to surgery influences outcome,this is important to know but was reported in only 19 (58%) of the studies [44].Patients who are on opiates may have less favorable outcome than those who are not,yet opiate use prior to surgery was reported in only 12 (36%) studies [ 24,45 ].Thus,the first key finding is thatthere is substantial heterogeneity between reports on the clinical baseline at the time of surgery.
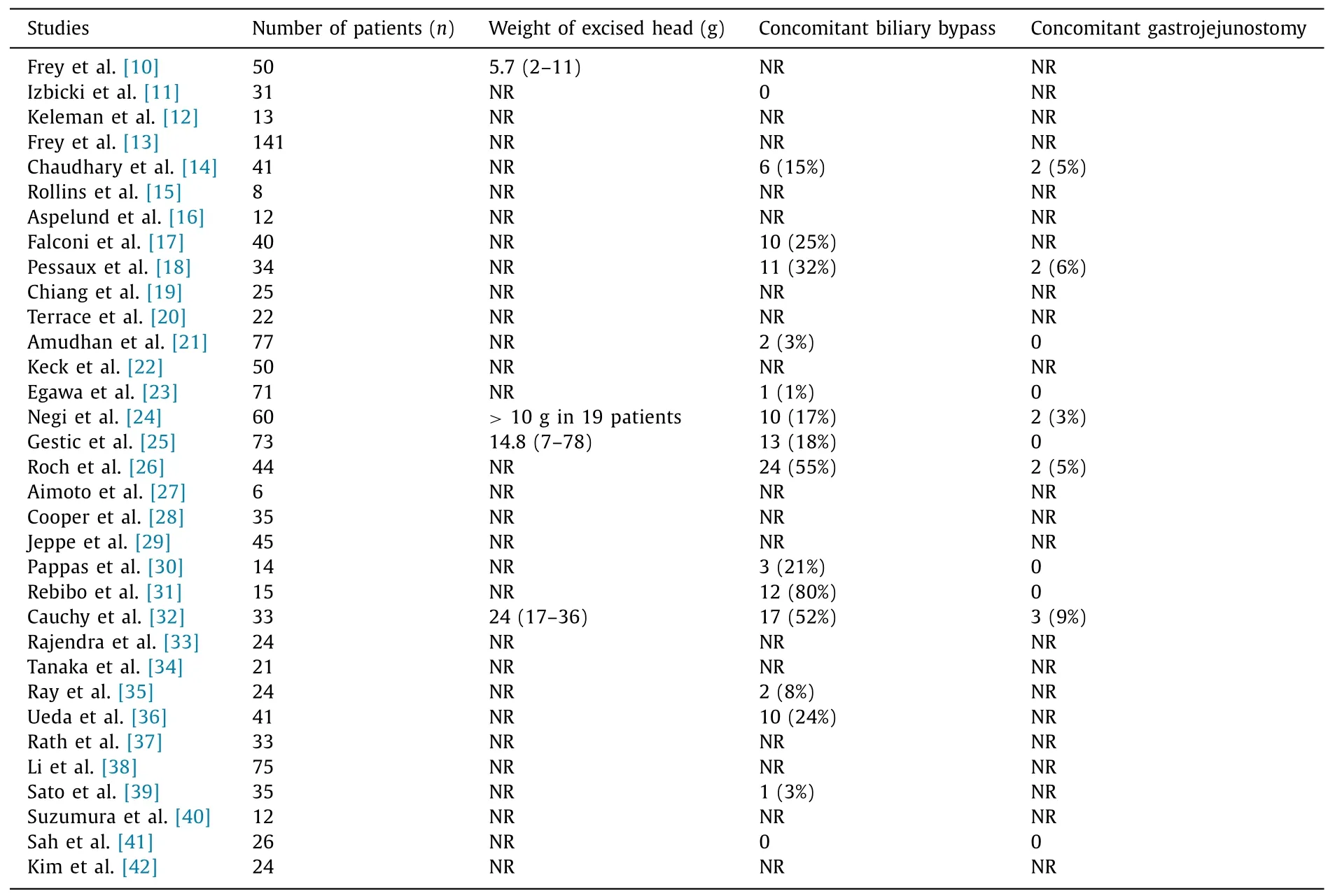
Table 3 Operative detail in patients undergoing longitudinal pancreatojejunostomy with partial head resection.
Second,the morphology of the diseased gland will most likely have an influence on the procedure.In this regard,in all series in adult patients,the main pancreatic duct was greater than 5 mm in diameter.In relation to“coring”of the parenchyma in the head of the gland,it is necessary to know the antero-posterior diameter of the head and this was reported in 13 (39%) studies [46].Patency of the portal vein was only reported in 3 (9%) studies,and this is likely to be because this procedure would be undertaken only in patients without portal hypertension from an occluded portal vein.
In order to assess the effectiveness of the procedure,in addition to information regarding the presence or absence of a pancreatic head mass,it is important to know how much pancreatic parenchyma was excised.In this regard,3 (9%) of the studies reported the weight of excised pancreatic parenchyma.
These provide the second key finding of this report,that information on duct diameter,pancreatic head mass and,critically,information on excised parenchyma (and ratio of extent of head resection to remnant) is limited.The final component of the study was assessment of outcome.In this regard,reporting of early and late operative outcomes appears relatively complete.There were 9(0.7% of 1205) post-operative deaths indicating that this is an acceptably safe procedure.The importance of post-operative diabetes mellitus is indicated by the fact that 24 (73%) of the studies reported on this.Interestingly,in light of the premise of the proponents of the Beger operation that transection of the neck of the pancreas is important to prevent subsequent portal vein occlusion and extra-hepatic portal hypertension,it is of note that no studies reported portal vein occlusion after longitudinal pancreatojejunostomy with partial head resection.
In summary,this study undertakes the first comprehensive assessment of reporting of the longitudinal pancreatojejunostomy with partial pancreatic head resection (the Frey procedure).It is stressed that the data must be interpreted with caution as they likely incorporate a range of biases.Nonetheless,our study shows that there is substantial heterogeneity between reports on the clinical baseline at the time of surgery.Details on technical conduct of the operation are limited and likely to compromise comparison between centers and surgeons but also between types of procedure.This point has not been adequately appreciated in the published literature to date.Finally,these limitations notwithstanding,longitudinal pancreatojejunostomy with partial pancreatic head resection for chronic pancreatitis is a safe procedure with a post-operative mortality rate of 0.7% and seemingly acceptable outcomes.In order to present a balanced perspective,it should be noted that Sakata et al.reported outcome in a series of 57 patients undergoing longitudinal pancreatojejunostomy with partial pancreatic head resection [47].In this small series they found no correlation between weight of excised parenchyma and outcome,suggesting that the key component is adequate decompression of the main pancreatic duct in the head of the gland.
In modern surgery it is also likely that this procedure can be undertaken using minimal access techniques [48].The requirement for standardized reporting applies regardless of whether open,laparoscopic or robotic approaches are used.
In conclusion,this study demonstrates that the reporting of case selection,gland morphology,operative detail and outcome after longitudinal pancreatojejunostomy with partial pancreatic head resection is inconsistent.This inconsistency critically compromises the ability to compare reports between surgeons,centers and dif-ferent types of surgical operation for chronic pancreatitis.More structured reporting of outcome is necessary both for clinicians to assess the choice of procedure and for patients in order to make informed choices when seeking treatment for painful chronic pancreatitis.
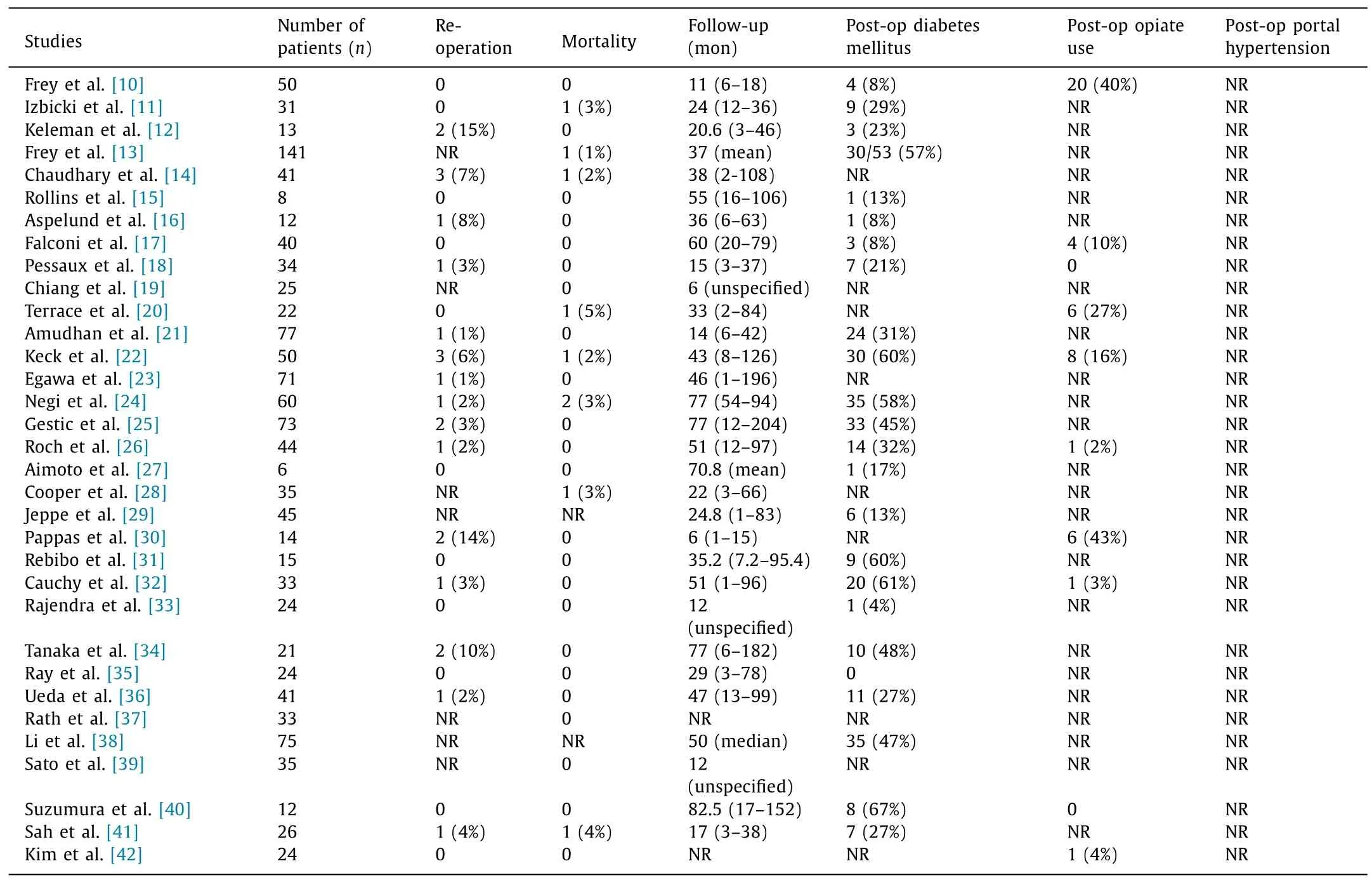
Table 4 Outcome after longitudinal pancreatojejunostomy with partial head resection.
Acknowledgments
None.
CRediT authorship contribution statement
Minas Baltatzis:Data curation,Formal analysis,Investigation,Writing -original draft.Santhalingam Jegatheeswaran:Formal analysis,Writing -original draft.Ajith K Siriwardena:Conceptualization,Supervision,Writing -review &editing.
Funding
None.
Ethical approval
Not needed.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Supplementary materials
Supplementary material associated with this article can be found,in the online version,at doi:10.1016/j.hbpd.2021.02.004 .
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Practice of precision surgery in primary liver cancer
- Hepatobiliary&Pancreatic Diseases International
- Presentation and surgical management of xanthogranulomatous cholecystitis
- Transjugular intrahepatic portosystemic shunt is effective in patients with chronic portal vein thrombosis and variceal bleeding
- Long-term follow-up of HCV patients with sustained virological response after treatment with pegylated interferon plus ribavirin
- Laparoscopic hepatectomy is superior to open procedures for hepatic hemangioma