Transjugular intrahepatic portosystemic shunt is effective in patients with chronic portal vein thrombosis and variceal bleeding
2021-05-19XioYnSunGungChunWngJingWngGungJunHungChunQingZhng
Xio-Yn Sun ,Gung-Chun Wng ,Jing Wng ,Gung-Jun Hung ,Chun-Qing Zhng ,
a Department of Gastroenterology, Shandong Provincial Hospital Affiliated to Shandong First Medical University, Jinan 250021, China
b Department of Infectious Diseases, Shandong Provincial Hospital Affiliated to Shandong First Medical University, Jinan 250021, China
Keywords:Chronic portal vein thrombosis Transjugular intrahepatic portosystemic shunt Variceal bleeding Hepatic encephalopathy
ABSTRACT Background: Studies about treatment of patients with chronic portal vein thrombosis (CPVT) are still limited,especially in different types of CPVT.This study aimed to evaluate the effect of transjugular intrahepatic portosystemic shunt (TIPS) in all types of CPVT with variceal bleeding.Methods: Patients with CPVT who received TIPS treatment between January 2011 and June 2019 were divided into four types according to the extent of thrombosis.All patients had a history of variceal bleeding.The characteristics and clinical parameters were collected and recorded.Data on procedure success rate,variation in portal vein pressure,rebleeding,hepatic encephalopathy (HE),stent stenosis,and overall mortality were analyzed.Results: A total of 189 patients were included in this study (39 in type 1,84 in type 2,48 in type 3,18 in type 4).The TIPS procedure success rate was 86.2%.The success rate was significantly different among the four types (89.7% vs.88.1% vs.83.3% vs.77.8%,P=0.001).In the TIPS success group,portal vein pressure was significantly reduced from 27.15 ± 6.59 to 19.74 ± 6.73 mmHg after the procedure(P < 0.001) and the rebleeding rate was significantly lower than that of the fail group (14.7% vs.30.8%,P=0.017).In addition,there were no significant differences in HE rate (30.7% vs.26.9%,P=0.912) or overall mortality (12.9% vs.19.2%,P=0.403) between the TIPS success group and the fail group.In the TIPS success group,we found that the occurrence of HE was significantly different (P=0.020) among the four types,while there were no significant differences in rebleeding rate (P=0.669),stent stenosis rate(P=0.056),or overall mortality (P=0.690).Conclusions: TIPS was safe and effective in decreasing portal vein pressure and rebleeding rate in patients with CPVT.
Introduction
Chronic portal vein thrombosis (CPVT) occurs mainly in liver cirrhosis,portal vein hypertension,bone marrow hyperplastic tumors,malignant tumors,acute abdominal inflammation,abdominal surgery and other basic diseases [ 1,2 ].CPVT rate is 10% −23% in cirrhotic patients [3].CPVT in non-cirrhotic patients is due mainly to congenital or acquired thrombosis [ 4,5 ].After embolization of the portal vein,collateral circulation is built up around the venous thrombus,then cavernous transformation of the portal vein is generated.CPVT has a variety of clinical manifestations,ranging from asymptomatic to life-threatening,such as gastroesophageal variceal bleeding,ascites and splenomegaly with hypersplenism [6].Gastroesophageal variceal bleeding is very common and acute massive bleeding can be life-threatening,and effective treatment reduces the bleeding and mortality.Up to now,there is no gold standard for the prevention of recurrent variceal bleeding in patients with CPVT [7-9].
The current therapeutic strategies for CPVT include conservative managements,interventional treatment,and surgery.Previous studies [10-12]have shown that although non-selectiveβblockers reduce portal hypertension through decreasing heart rate,the risk of recurrent bleeding cannot be controlled effectively.Surgery usually is not feasible because of mesenteric or splenic vein thrombosis,a history of splenectomy,and risk of bleeding.Compared to surgery,interventional therapy such as transjugular intrahepatic portosystemic shunt (TIPS) is less invasive and more reliable.To our knowledge,TIPS is currently used widely in patients with CPVT,especially in those who do not respond to nonselectiveβ-blockers and anticoagulation treatments [13-15].TIPS decreases portal vein pressure and restores portal vein blood flow,which effectively prevent recurrent bleeding and relieve refractory ascites [16-18].
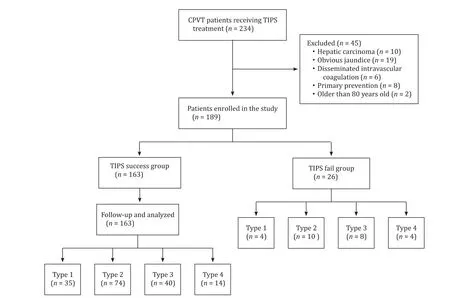
Fig.1.Study design and flow diagram.CPVT:chronic portal vein thrombosis;TIPS:transjugular intrahepatic portosystemic shunt.
Although CPVT was considered a contraindication for TIPS in the past,recent studies have demonstrated the effectiveness of TIPS for CPVT [ 19,20 ].Senzolo et al.[14]reported that cavernous transformation of the portal vein should not be seen as a contraindication of TIPS,but it does increase the technical difficulty of the procedure.TIPS has been recently improved significantly.The percutaneous transhepatic or transsplenic puncture can be adopted according to the patient’s situation [ 21,22 ].Up to now,there has been only limited research on CPVT [ 19,20 ],and especially little is known about the effect of TIPS in different types of CPVT.The present study was to investigate the application of TIPS in different types of CPVT with variceal bleeding.
Patients and methods
Patients
From January 2011 to June 2019,234 patients with CPVT received TIPS treatment in our hospital (Fig.1).CPVT was previously diagnosed PVT,with cavernous changes in portal vein,signs of portal hypertension,and without high density thrombus on imaging,by B-ultrasound,computerized tomography (CT),magnetic resonance (MR) or digital subtraction angiography (DSA) [23].Indication for TIPS was CPVT with risks of variceal bleeding or rebleeding.
Exclusion criteria including:(i) hepatocellular carcinoma or other malignancy;(ii) hepatic encephalopathy (HE) above grade 2;(iii) obvious jaundice,total bilirubin ≥3 upper limit of normal;(iv)coagulation dysfunction,prothrombin time>25 s;(v) no history of variceal bleeding;(vi) severe hypertension,cardiopulmonary insufficiency or cerebrovascular diseases;(vii)<18 or>80 years old;(viii) patients with missing clinical data.Using these exclusion criteria,45 patients were excluded from the study (10 with liver cancer,19 with obvious jaundice,6 with disseminated intravascular coagulation,8 with no history of variceal bleeding,and 2 aged over 80 years).
Patients with CPVT were classified into four clinical types according to the extent of thrombosis based on the previous study with modification [24].Type 1:thrombosis occurs only in the main portal vein.Type 2:thrombosis occurs in the main portal vein,and in one of the intrahepatic branches,left or right.Type 3:thrombosis occurs in the main portal vein,and in both the left and right intrahepatic branches,whether extending to the superior mesenteric vein or not.Type 4:thrombosis occurs in the main portal vein,left and right intrahepatic branches,the superior mesenteric vein and splenic vein.The computed tomography images are shown in Fig.2 .
A total of 189 patients with CPVT were included in this study,including both cirrhosis and non-cirrhosis patients.Non-cirrhosis CPVT was associated with diseases such as myeloproliferative disease,ankylosing spondylitis,antiphospholipid syndrome,systemic lupus erythematosus,Wilson disease and leucoderma.The clinical characteristics of all these patients are presented in Table 1 .This study was approved by the Ethics Committee of our hospital.The requirement for written informed consent was waived because of the retrospective nature of the study.

Fig.2.Computed tomography (CT) images of the four types of chronic portal vein thrombosis (CPVT).A:type 1,thrombosis in the main portal vein only;B:type 2a,thrombosis in the main portal vein and the left intrahepatic branches;C:type 2b,thrombosis in the main portal vein and the right intrahepatic branches;D:type 3a,thrombosis in the main portal vein and in both the left and right intrahepatic branches;E:type 3b,thrombosis in the main portal vein,the left and right intrahepatic branches,and the superior mesenteric vein;F:type 4,thrombosis in the main portal vein,the left and right intrahepatic branches,the superior mesenteric vein,and splenic vein.MPV:main portal vein;LPV:the left intrahepatic branches of portal vein;RPV:the right intrahepatic branches of portal vein;SMV:superior mesenteric vein;SV:splenic vein.
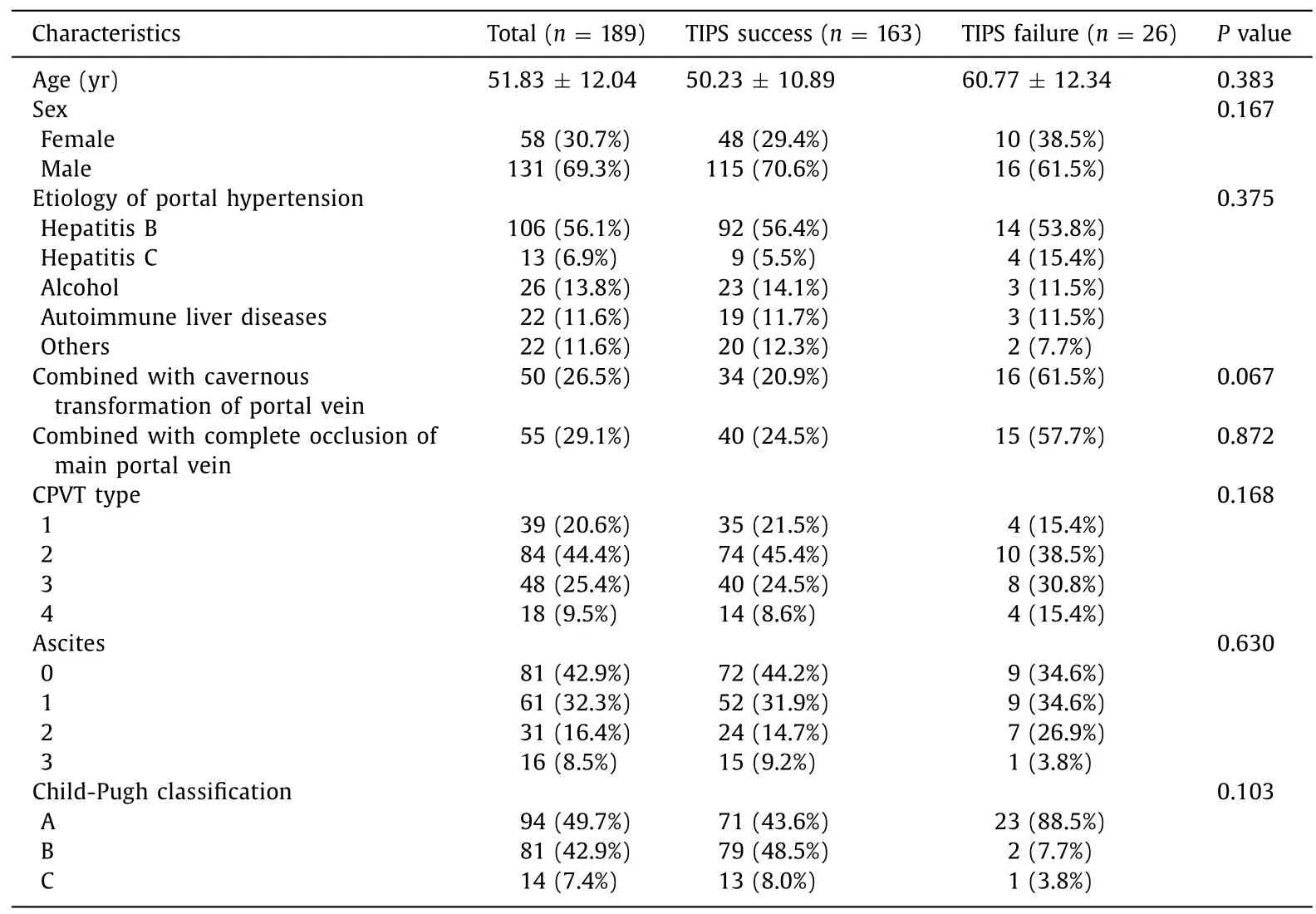
Table 1 Clinical characteristics of patients.
TIPS procedure
Under local anesthesia,the portal vein angiography was performed.In brief,a catheter was placed through the jugular vein to the inferior vena cava or hepatic vein,then portal vein angiography was performed and portal vein pressure was measured.A balloon was used to dilate the intrahepatic parenchyma;then a stent was placed to establish the intrahepatic portal shunt,and the portal vein pressure was measured again.If intrahepatic portal vein branches were observed through indirect portography,the conventional transjugular puncture approach could be used.

Fig.3.Procedures of transjugular intrahepatic portosystemic shunt.Preoperative CT indicated that thrombus was found in the main,left and right branches of portal vein and superior mesenteric vein,which made direct puncture difficult.The right internal jugular vein was punctured using the Seldinger technique,then the right femoral artery was punctured,the right hepatic artery branch was superselect,and the mark was retained.A:the left branch of the portal vein was successfully punctured from the right hepatic vein with a Rups-100 puncture needle and the guide wire successfully entered the superior mesenteric vein;B:angiography showed that the portal vein root sends out large collateral circulation to participate in the blood supply of esophageal and gastric varices,and the direct portal vein pressure was measured (35 mmHg);C:surgical glue and iodized oil (1:3) were used to embolize varicose vessels through the catheter;D:the thrombus was drawn out repeatedly;a 10 × 80 mm TIPS special covered stent was implanted first,and then a 10 × 80 mm BARD bare stent was extended downward;E:angiography showed that stent blood flow was unobstructed and the collateral vessel embolism was satisfactory,then the direct portal vein pressure was measured (18 mmHg).
In type 1,we preferred the conventional transjugular approach first,but a percutaneous transhepatic or transsplenic approach was required if indirect portal vein angiography could not show the main portal vein and intrahepatic branches.In the other three types,the portal vein and its branches were largely invisible through indirect portal angiography;thus,a percutaneous transhepatic or transsplenic approach under CT guidance was required.After the PVT was visualized,standard TIPS procedure was used to reconstruct the portal vein blood flow.After inserting the guide wire,we managed the catheter to pass through the blocked portal vein segment to arrive at the superior mesenteric vein or splenic vein,then angiography was performed,portal vein pressure was measured and recorded.During the TIPS procedure,we placed a covered stent combined with a bare stent as usual [25].Distal end of the placed stent was required to pass completely through the thrombus.Additional stent was needed to ensure complete coverage of the stenosis or thrombus segment if the thrombus was large,which is consistent with the previous studies [ 25,26 ].The stents (10 mm diameter) commonly used in TIPS included the covered stent (BARD,Murray Hill,New Jersey,USA),bare stent (ev3 Protege GPS,Minneapolis,Minnesota,USA or BARD) and TIPS covered stent system (Viatorr,Gore,Flagstaff,Arizona,USA).If varices were still observed after stent placement,transcatheter embolization of the varices was needed using surgical glue and iodized oil(1:3) (Fig.3).Technical success was defined as angiography after stent placement showing the stent in good position and smooth blood flow.
Postoperative treatment
After a successful TIPS procedure,patients received a subcutaneous injection of low-molecular-weight heparin 50 0 0 U for 7 days,followed by anticoagulant therapy with oral aspirin.
Follow-up
All patients were followed up by telephone and clinic visit.They were evaluated at 1,2,3 months after the TIPS procedure,and then every 3 months or whenever the patients’ condition changed.Data on clinical parameters were collected and recorded at each followup,including rebleeding,HE,stent patency and survival.Rebleeding was defined by clinical symptoms and laboratory indicators.HE was diagnosed by routine nervous system examination and laboratory tests according to the West Haven criteria [27].Stent patency was detected by B-ultrasound or CT.
Endpoints
The primary endpoint of this study was rebleeding,which was defined by Baveno IV consensus [8](hematemesis and hematochezia;hemoglobin decrease>30 g/L;systolic blood pressure<100 mmHg or decrease>20 mmHg and/or pulse rate>100/min).The secondary endpoint was the survival time of the patients.
Statistical analysis
The software package SPSS 22.0 (SPSS Company,Chicago,IL,USA) was used for statistical analysis.Numerical data were expressed as mean ± SD or median (IQR);qualitative variables wereexpressed as number (percentage).Quantitative variables were analyzed by the Student’st-test or nonparametric test,and qualitative variables were analyzed by the Fisher’s exact test or the Chi-square test.Kaplan-Meier estimates and log-rank test were used to compare the time-event data.AP<0.05 was considered statistically significant.
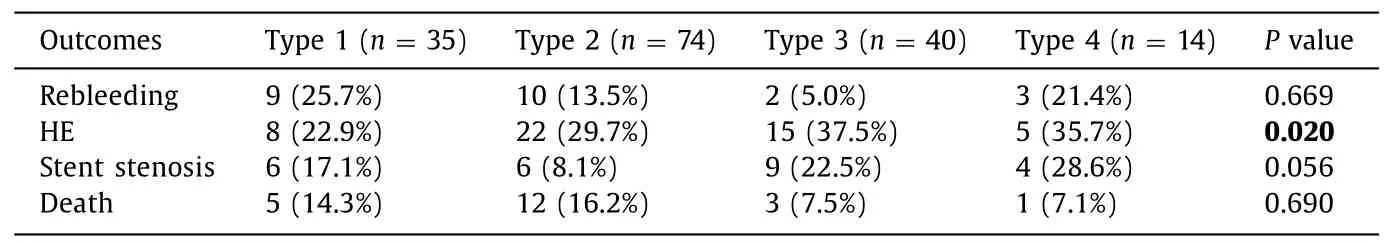
Table 2 Follow-up outcomes of patients in TIPS success group.
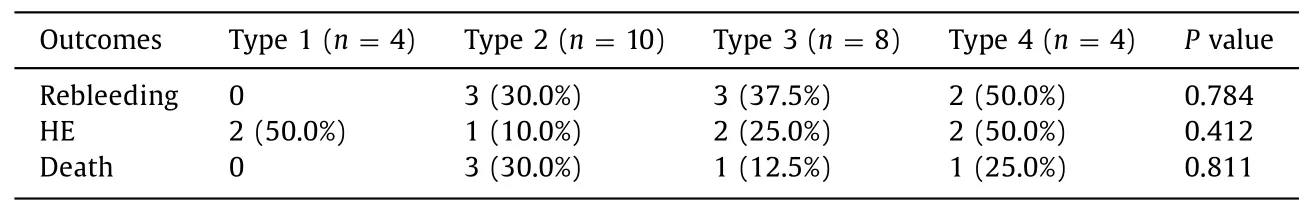
Table 3 Follow-up outcomes of patients in TIPS fail group.
Results
Characteristics of the participants
A total of 189 patients with CPVT who had a history of variceal bleeding received TIPS treatment were analyzed (Fig.1).There was no significant difference in baseline demographics and clinical findings between the TIPS success and fail groups (Table 1).The median follow-up period was 14 (3–31) months in the TIPS success group,and 18 (7–25) months in the TIPS fail group.There was no significant difference in the follow-up time between the two groups (P=0.673).The number of patients with type 1,type 2,type 3 and type 4 CPVT was 39,84,48 and 18,respectively.The follow-up outcomes of patients in the TIPS success and fail groups are shown separately in Tables 2 and 3 .
Technique outcomes
The TIPS procedure success rate was 86.2% (163/189) and the median duration of the procedure was 170 (130–225)minutes.Specific procedures included simple conventional TIPS(n=45),TIPS combined with a percutaneous transhepatic approach (n=86),and TIPS combined with a percutaneous transsplenic approach (n=58).No procedure-related complications were observed in any of the patients in our study.The success rate was significantly different among the four subtypes (89.7%in type 1,88.1% in type 2,83.3% in type 3,and 77.8% in type 4)(P=0.001).The success rate in patients with the main portal vein completely blocked (72.7%,40/55) was significantly lower than in those without complete blockage (91.8%,123/134) (P<0.001).The success rate in patients with cavernous transformation of portal vein (68.0%,34/50) was significantly lower than in those without(92.8%,129/139) (P<0.001).
Portal vein pressure
Portal vein pressure was significantly reduced from 27.15 ± 6.59 to 19.74 ± 6.73 mmHg in the TIPS success group (P<0.001).We also found that the portal vein pressure in all the types of CPVT was significantly reduced after the successful TIPS procedure,from 28.53 ± 7.31 to 21.21 ± 6.96 mmHg in type 1 (P=0.031),from 26.82 ± 5.93 to 20.03 ± 6.54 mmHg in type 2 (P=0.001),from 26.60 ± 7.08 to 17.50 ± 6.54 mmHg in type 3 (P<0.001),and from 28.14 ± 7.44 to 19.07 ± 5.48 mmHg in type 4 (P=0.025).However,in the TIPS fail group,there was no significant change in portal vein pressure (P=0.187).
Rebleeding
During the follow-up,rebleeding rate in the TIPS success group was significantly lower than that in the fail group (14.7% vs.30.8%,P=0.017,Fig.4 A).In the TIPS success group,there was no significant difference among the four types in rebleeding (P=0.669,Fig.5 A).Also,the rebleeding rate was not significantly different among the four types in the TIPS fail group (P=0.784).
HE
HE might be the most common complication after the TIPS procedure.There was no significant difference in HE occurrence between the TIPS success and fail groups (30.7% vs.26.9%,P=0.912,Fig.4 B).In the TIPS success group,HE occurred in 50 patients (8 in type 1,22 in type 2,15 in type 3,and 5 in type 4).The occurrence was significantly different among the four types (P=0.020,Fig.5 B).In the TIPS fail group,HE occurred in 7 patients (2 in type 1,1 in type 2,2 in type 3,and 2 in type 4),and there was no significant difference among the four types (P=0.412).All patients who suffered from HE recovered after conventional treatments.
Stent stenosis
Stent stenosis occurred in 25 patients after TIPS success during the follow-up period:6 in type 1 (17.1%,6/35),6 in type 2 (8.1%,6/74),9 in type 3 (22.5%,9/40),and 4 in type 4 (28.6%,4/14).There was no significant difference among the four types (P=0.056,Fig.5 C).In the 25 patients,an additional stent was inserted in 14 patients.
Survival
There was no significant difference in survival rate between the TIPS success and fail groups (12.9% vs.19.2%,P=0.403,Fig.4 C).In the TIPS success group,21 patients died during the follow-up period (7 died of uncontrolled recurrent bleeding,9 died of liver failure,and 5 died of cardiopulmonary failure).There was no significant difference among the four types (5 in type 1,12 in type 2,3 in type 3,and 1 in type 4) (P=0.690,Fig.5 D).In TIPS fail group,5 patients died during the follow-up period (3 died of uncontrolled recurrent bleeding,2 died of liver failure).There was no significant difference among the four types (P=0.811).

Fig.4.Follow-up outcomes in the transjugular intrahepatic portosystemic shunt success and fail groups.A:rebleeding rate;B:hepatic encephalopathy rate;C :survival.
Discussion
Development of CPVT usually increases the portal vein pressure and decreases the blood flow to the liver,leading to increased risk of variceal bleeding and ascites,decreased liver function.Because variceal bleeding is life-threatening,prevention of rebleeding is very important.Up to now,the use of anticoagulants in treatment of CPVT is still controversial.Sarin et al.[28]suggested that anticoagulation is effective and safe for primary prevention of PVT in patients with cirrhosis;but another study [3]recommended that thrombolytic therapy for patients with extensive PVT should be carefully considered.Application of TIPS was limited in the past because the procedure was technically difficult in patients with cavernous transformation of portal vein.Over the last 10 years,the TIPS technique was improved significantly and its use has been expanded [29].For example,PVT used to be a relative contraindication for TIPS,but it has now become an indication.Several studies showed that the success rate of TIPS procedure in patients with cavernous transformation of portal vein varied from 20% to 75% [ 14,30,31 ].The wide variation in success rate of TIPS among these patients might be due to the wide variation of PVT.Previous studies have shown that maintenance of TIPS patency can be achieved using an expanded-polytetrafuoroethylene (ePTFE)-covered stent [ 25,26,32 ],which is applied to patients with portal hypertension.TIPS can enable recanalization of the obstructed portal vein and then alleviate the symptoms of portal hypertension.However,there has been limited research in this field in recent years.To our knowledge,study about TIPS as a treatment for different types of CPVT is even rare.
We divided CPVT into four types according to the extent of the thrombosis.Previous studies showed that the wider the extent of PVT,the lower the procedure success rate [33-35].In this study,we found that the TIPS success rate in patients with a completely blocked main portal vein (72.7%) was significantly lower than in those without complete blockage (91.8%);and that the success rate in patients with cavernous transformation of portal vein (68.0%) was significantly lower than in those without(92.8%).Consistent with previous research,we found that complete occlusion of the main portal vein or cavernous transformation of the portal vein was significantly associated with reduced success rate of TIPS in patients with CPVT.Several investigations found that transjugular approach combined with transhepatic or transsplenic approach were valuable in the puncture of the portal system [36-39].
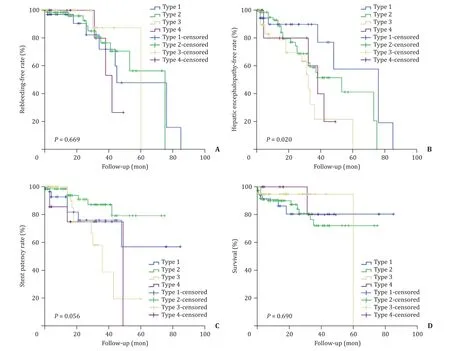
Fig.5.Postoperative differences of the four types in the transjugular intrahepatic portosystemic shunt success group.A:rebleeding rate;B:hepatic encephalopathy rate;C:stent patency rate;D:survival.
Shunt dysfunction occurring after TIPS was usually due to thrombosis in the stent [ 39,40 ].In this study,the stent patency rate was 84.7% (138/163) during the follow-up period.An additional stent was inserted in 14 of 25 stent dysfunction patients.Because previous studies showed that covered stents could effectively reduce the in-stent stenosis rate after stent implantation [ 26,40 ],we attempted to implant a covered stent.We recommend the use of an ePTFE-covered stent to maximize long-term efficacy,as demonstrated by a preliminary study in cirrhotic patients [40].Selection of stent diameter has been studied previously.Some studies indicated that a 12-mm diameter stent can achieve full shunt,but the high rate of HE led many researchers to conclude that 10-mm and 8-mm diameter stents were more suitable [ 40,41 ].However,studies of 8-mm diameter stents showed insufficiently shunt,suggesting that a 10-mm diameter stent may be a more appropriate choice [41-43].In our study,10-mm diameter TIPS stents were commonly used,including covered stent 10 × 80 mm (BARD) and bare stent 10 × 80 mm (ev3 Protege GPS or BARD),which were consistent with findings of the previous research.In recent years,use of TIPS covered stent system,a combination of covered stent and bare stent,have made stent placement more convenient.Research has also found that postoperative anticoagulant therapy can reduce the rate of stent dysfunction [44].Thus,anticoagulant treatment was used after TIPS to prevent recurrent thrombosis.Lowmolecular-weight heparin and aspirin were administered to all the CPVT patients after a successful TIPS procedure.Because anticoagulant therapy was administered to all patients after a successful TIPS procedure,its effect on patient outcomes was not evaluated in this study.In further research,we will evaluate the effect of anticoagulant therapy on stent patency.
A previous research demonstrated the clinical effects of TIPS in preventing recurrent esophageal variceal bleeding in patients with cavernous transformation of portal vein [45].Consistent with earlier research,our study found that rebleeding rate in the TIPS success group was significantly lower than that in the fail group.This might be due to the significant decrease of portal vein pressure.The lack of a significant difference in rebleeding rate among the four types in the success group suggested that TIPS can effectively prevent rebleeding in all types of CPVT.Our study found that TIPS procedure did not improve patient survival in any type of CPVT.However,the small sample size in our study,especially in type 3 and type 4,indicated the need for a randomized controlled trial of larger patient samples to confirm the reduction of rebleeding after TIPS and to evaluate whether TIPS improves patient survival or not.
Previous studies [ 25,46 ]have shown that patients were at risk for HE after TIPS treatment,and that the incidence of HE was higher in patients treated with TIPS than that in patients receiving other treatments such as endoscopic variceal ligation and percutaneous transhepatic variceal embolization.Several studies also found that TIPS does not increase the incidence of HE in patients with progressive cirrhosis and PVT [ 16,45 ].Our study found that there was no significant difference in the incidence of HE between the TIPS success and fail groups.A previous study has shown that portal perfusion might decrease or even disappear because of significantly increased arterial perfusion before the TIPS procedure [47].That might explain the lack of difference in HE rate between the TIPS success and fail groups in our study.
In conclusion,TIPS can be considered a viable,safe,and effective interventional treatment for all types of CPVT patients with a history of variceal bleeding.
Acknowledgments
None.
CRediT authorship contribution statement
Xiao-Yan Sun:Data curation,Formal analysis,Methodology,Writing -original draft.Guang-Chuan Wang:Funding acquisition,Investigation,Software,Validation.Jing Wang:Funding acquisition,Methodology,Project administration,Resources.Guang-Jun Huang:Investigation,Visualization.Chun-Qing Zhang:Conceptualization,Supervision,Writing -review &editing.
Funding
This study was supported by grants from Shandong Province Key Research and Development projects (2017GSF218026 and 2016GSF201001),and Health and Family Planning Commission of Shandong Province (2017WS199).
Ethical approval
This study was approved by the Ethics Committee of Shandong Provincial Hospital (No.2017447).The requirement for written informed consent was waived because this was a retrospective study.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Practice of precision surgery in primary liver cancer
- Reporting of longitudinal pancreatojejunostomy with partial pancreatic head resection (the Frey procedure) for chronic pancreatitis:A systematic review
- Hepatobiliary&Pancreatic Diseases International
- Presentation and surgical management of xanthogranulomatous cholecystitis
- Long-term follow-up of HCV patients with sustained virological response after treatment with pegylated interferon plus ribavirin
- Laparoscopic hepatectomy is superior to open procedures for hepatic hemangioma