Complete resection of the gastric antrum decreased incidence and severity of delayed gastric emptying after pancreaticoduodenectomy
2021-05-19YuLingSunJinJunGouKiMingZhngWenQiLiXiuXinLinZhouRongToZhuJinLi
Yu-Ling Sun , ,Jin-Jun Gou ,Ki-Ming Zhng ,Wen-Qi Li ,Xiu-Xin M ,Lin Zhou ,Rong-To Zhu ,Jin Li
a Institute of Hepatobiliary and Pancreatic Diseases, Department of Hepatobiliary and Pancreatic Surgery, the First Affiliated Hospital of Zhengzhou University, Zhengzhou 450052, China
b Department of Digestive, the First Affiliated Hospital of Zhengzhou University, Zhengzhou 450052, China
Keywords:Delayed gastric emptying Gastric antrum Gastric electrophysiology Histological morphology Pancreaticoduodenectomy
ABSTRACT Background: Delayed gastric emptying (DGE) is the main complication after pancreaticoduodenectomy(PD),but the mechanism is still unclear.The aim of this study was to elucidate the role of complete resection of the gastric antrum in decreasing incidence and severity of DGE after PD.Methods: Sprague-Dawley rats were divided into three groups:expanded resection (ER group),complete resection (CR group),and incomplete resection (IR group) of the gastric antrum.The tension (g) of remnant stomach contraction was observed.We analyzed the histological morphology of the gastric wall by different excisional methods after distal gastrectomy.Moreover,patients underwent PD at our department between January 2012 and May 2016 were included in the study.These cases were divided into IR group and CR group of the gastric antrum,and the clinical data were retrospectively analyzed.Results: The ex vivo remnant stomachs of CR group exhibited much greater contraction tension than others (P < 0.05).The contraction tension of the remnant stomach increased with increasing acetylcholine concentration,while remained stable at the concentration of 10 × 10 −5 mol/L.Furthermore,174 consecutive patients were included and retrospectively analyzed in the study.The incidence of DGE was significantly lower (3.5% vs.21.3%,P < 0.01) in CR group than in IR group.In addition,hematoxylin-eosin staining analyses of the gastric wall confirmed that the number of transected circular smooth muscle bundles were higher in IR group than in CR group (8.24 ± 0.65 vs.3.76 ± 0.70,P < 0.05).Conclusions: The complete resection of the gastric antrum is associated with decreased incidence and severity of DGE after PD.Gastric electrophysiological and physiopathological disorders caused by damage to gastric smooth muscles might be the mechanism underlying DGE.
Introduction
Pancreaticoduodenectomy (PD) is a routine surgical procedure for patients with periampullary or pancreatic neoplasms.However,the morbidity of this procedure remains high and a major complication is delayed gastric emptying (DGE) or gastroparesis (accounted from 20% to 70%),which leads to prolonged hospitalization,increased costs,and greater numbers of hospital readmissions [ 1,2 ].
In recent decades,surgeons have drawn great attention to DGE after PD.Some suggest that standard pancreaticoduodenectomy is associated with a lower rate of DGE than pylorus-preserving pancreaticoduodenectomy (PPPD) [ 3,4 ],but others yield contrary results [ 5,6 ].Nevertheless,the incidence of this complication is equivalent among above surgical techniques [7].Therefore,which method yields a lower rate of DGE remains a matter of debate,and the mechanism of DGE remains unclear.
Normal gastric emptying is controlled by the autonomic nervous system,smooth muscle cells,and enteric neurons [8].Gastroparesis is a motility disorder of the stomach without evidence of mechanical obstruction,and this etiology is multifactorial.A number of novel insights have demonstrated that histological abnormalities include injury and the loss of interstitial cells of Cajal(ICC),a reduction in the number of enteric nerve fibers,smooth muscle fibrosis and gastric arrhythmias [9-11].Acetylcholine (Ach)is the neurotransmitter that is most commonly used to induce gastrointestinal smooth muscle contractions.In the gastrointestinal tract,Ach is released from excitatory enteric motor neurons that express choline acetyltransferase and vesicular Ach transporters and mediate immediate smooth muscle contraction [ 12,13 ].
Postsurgical gastroparesis usually occurs after injury to the vagus nerve following upper abdominal operations [14].In sixty patients who developed stasis after gastric surgery,80% had received a partial gastrectomy [15].Considering recent developments in the field,we postulated that (i) the method of gastrectomy is important for the occurrence of DGE after PD;(ii) injury to smooth muscle may be the mechanism underlying dysfunctional gastric emptying;(iii) complete resection of the gastric antrum is probably associated with decreased incidence and severity of DGE after PD.Therefore,this study set out to assess the effect of complete resection of the gastric antrum in decreasing incidence and severity of DGE after PD.First,we investigated the effect of three methods of distal gastrectomy on remnant stomach contraction in rats.Then,we studied the effect of the Ach concentration on the tension of stomach contractions in rats.Finally,we analyzed the effect of different distal gastrectomy techniques during PD for patients on the incidence and severity of DGE.
Methods
Animals
Healthy male Sprague-Dawley rats (weighing 280–300 g) were obtained from the Experimental Animal Center of Shanxi Medical University.The experiments were approved by the Laboratory Animal Care and Use Committee of Zhengzhou University.
Grouping and rat distal gastrectomy ex vivo
These rats were divided into three groups according to the excisional lines (n=10 for each group).After fasting for 12 to 16 h,the rats were quickly sacrificed by cervical dislocation.The abdominal cavity was then opened,the stomach was exposed and harvested,and the specimens were flushed with saline until no further stomach contents flowed out.The cardia was cleared of gastric-surrounding fat and connective tissue.The incisura angularis was identified as the cut-off point between the gastric antrum and the corpus in lesser curvature.From this point,three excisional lines were decided,and distal gastrectomy was performed.The first line (OA) was perpendicular to the horizontal line (incomplete resection of the gastric antrum,IR group),the second line (OB) was vertical to the longitudinal axis of the stomach (complete resection of the gastric antrum,CR group),and the third line (OC) was horizontal (expanded resection of the gastric antrum,ER group)(Fig.1).
Measurement of remnant stomach contraction
After distal gastrectomy,the tension (g) of the remnant stomach contraction was measured as described previously [ 16,17 ].A preload of 1.8 g was applied to the isolated stomachs,which were then stabilized in the perfusion tank for 60 to 80 min.Ach (concentration of 7.5 × 10−5mol/L) was then added to the perfusion tank,and the maximum contraction was recorded;after 5 min of stabilization,the tension-effect curves were recorded for 20 min using an Iox-2 biological signal acquisition system (Emkabath 2,Emka Technologies,Paris,France).

Fig.1.Excisional lines for distal gastrectomy and the location of control gastric species.Lines OA,OB,and OC illustrate the resection lines used for distal gastrectomy of incomplete resection (IR group),complete resection (CR group) and expanded resection of the gastric antrum (ER group),respectively.Line DE refers to the gastric longitudinal axis.Areas F and G indicate the samples got from stomach.
After observing the effects of the different excisional methods on remnant stomach contraction,the rats were divided into five groups (n=8 for each group),and distal gastrectomy was performed using the method that resulted in the strongest contraction.Ach was added at concentrations of 2.5 × 10−5,5.0 × 10−5,7.5 × 10−5,10 × 10−5 and 15 × 10−5 mol/L,and the tension-effect curves were recorded as described above.
Hematoxylin-eosin staining of human gastric specimens
Gastric specimens of ten patients with gastric cancer who underwent subtotal or total gastrectomy were used.The exact locations from which these samples were taken are shown as areas F and G in Fig.1 .After formalin fixation,the gastric specimens were harvested from the anterior or posterior wall,avoiding the cancerous side.Hematoxylin-eosin staining was performed,and the histology of the gastric smooth muscle was investigated.
Patients
This part of study was conducted with approval from the Ethics Committee of Zhengzhou University (2016062).From January 2012 to May 2016,patients underwent PD in our department were included and retrospectively analyzed.Of these patients,complete resection of the gastric antrum (CR group,n=85) and incomplete resection of the gastric antrum (IR group,n=89) for distal gastrectomy during PD were performed as described above.Patients with distant metastases tumor were judged to be contraindicated for PD.Patients receiving neoadjuvant chemoradiation and preoperative endoscopic or percutaneous transhepatic biliary drainage were also excluded from the study.
All patients underwent preoperative physical examination and biochemical testing.Preoperative clinical data were collected regarding age,sex,diabetes,total bilirubin and serum albumin.Operative and postoperative data were collected,including operative time,blood loss,incidence of DGE and postoperative pancreatic fistula (POPF),pathological diagnosis,length of hospital stay,abdominal infection,and new-onset diabetes.The postoperative complications of DGE,POPF and postpancreatic surgery hemorrhage were assessed according to the International Study Group of Pancreatic Surgery (ISGPS) and the International Study Groups on Pancreatic Fistula (ISGPF),respectively [ 4,18 ].

Fig.2.The different gastrointestinal anastomoses in the patients who underwent PD.A:The method used for gastrojejunostomy in the patients in the IR group.The excisional direction is perpendicular to the horizontal line.B:The method used for gastrojejunostomy in the patients in the CR group.The excisional line is vertical to longitudinal axis of the stomach.
Operative treatment
The area resected during PD was performed as described previously [9].Lymph nodes were dissected according to the standard of Whipple’s procedure.If necessary,combined portal vein resection or dissection of the para-aortic lymph nodes was performed to accomplish a complete tumor resection [19].All procedures were the same for patients in both groups,except for the resection of distal stomach.After identification of the anatomic point of incisura angularis in the lesser curvature,complete resection of the gastric antrum (CR group) and incomplete resection of the gastric antrum (IR group) for distal gastrectomy were performed.After complete resection of the specimens,the proximal jejunal stump was brought posteriorly through the mesenterium.Pancreaticojejunostomy was performed using a total closure of the pancreatic section for end-to-side anastomosis with 4–0 Prolene running sewing [20].Finally,an end-to-side gastrojejunostomy 4 cm in length was performed approximately 45 cm distal to the hepaticojejunostomy via the antecolic route.A schema of the reconstruction for gastrojejunostomy in both groups is shown in Fig.2 .All reconstructions were performed by hand-sewn anastomosis.Two closed drains were placed around the pancreatic and biliary anastomoses.
Postoperative management
The nasogastric tube was removed within 24 h postoperatively.Reinsertion of the gastric tube was performed if the patient complained of severe nausea,vomiting and severe distension of the abdomen.A prescribed postoperative oral diet protocol was followed,and drinking water was allowed after the nasogastric tube was removed.The diet began with liquefied rice on the next day;on the third day,rice-rich gruel was allowed,and regular rice was allowed on the 4th and 5th days.The dietary format was modulated according to the digestive symptoms.An enema was used for patients presenting abdominal distension during the course of the oral diet.Usually,a patient’s normal diet began on the 4th to 5th day after surgery.After the oral diet began,prokinetic agents were prohibited unless the patients presented with digestive symptoms.
Patients were considered for discharge or the start of adjuvant chemotherapy when they could eat satisfactorily and the performance status recovered to approximately the preoperative level.This level generally refers to the ability to routinely eat and to no longer require any supplemental nutrition.
Statistical analysis
Statistical analyses were performed using SPSS version 13.0(SPSS Inc.,Chicago,IL,USA).Categorical variables were expressed as group percentages and were compared using either Pearson Chi-square or Fisher exact tests.Continuous data were presented as mean ± standard deviation (SD) and compared using independent analysis of variance for normally distributed variables,and presented or as median (interquartile range) and compared with Mann-WhitneyUtest for non-normally distributed variables.APvalue<0.05 was considered statistically significant.
Results
Impact of different excisional methods on remnant stomach contraction after distal gastrectomy in rats
To determine whether different excisional methods after distal gastrectomy affected remnant stomach contraction,we first used three excisional lines for distal gastrectomy in rats and assessed the tension of remnant stomach contraction.We found that the remnant stomach contraction in CR group was much stronger than in ER and IR groups (CR vs.ER:2.67 ± 0.10 vs.2.06 ± 0.06 g,P<0.05;and CR vs.IR:2.67 ± 0.10 vs.2.05 ± 0.05 g,P<0.05).The tension of remnant stomach contraction was not significantly different between the ER and IR groups (Fig.3 A).The representative tension-effect curves for different groups are shown in Fig.3 C.These results indicate that different resection methods strongly influence the tension of residual gastric contraction after distal gastrectomy,and the residual gastric contraction in the CR group was the strongest.
Impact of the exogenous Ach concentration on stomach contractions after distal gastrectomy in rats
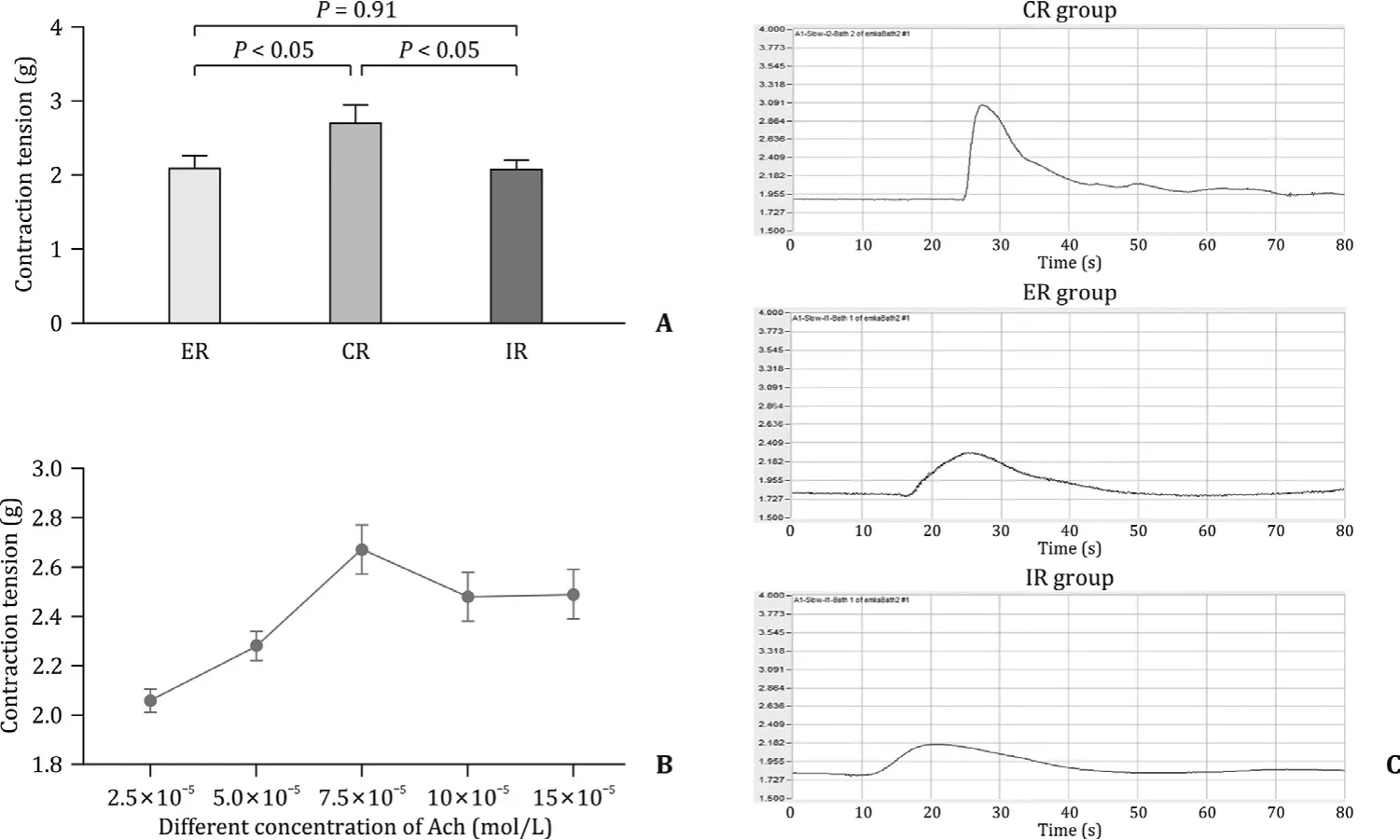
Fig.3.Effects of the different excisional methods and Ach concentrations on the contraction of remnant stomach after distal gastrectomy in rats.A:The remnant stomach contractions of rats in the CR,IR and ER groups;B:the contraction of gastric smooth muscle in different Ach concentration;C:representative tension-effect curves for different groups of rats.
We next focused on the effect of vagal fibers on stomach contraction after the complete resection of the gastric antrum by applying exogenous Ach at various concentrations.With the induction of contraction by the various concentrations of Ach,the average tensions of the remnant stomach after the complete resection of the gastric antrum were 2.06 ± 0.05 g,2.28 ± 0.06 g,2.67 ± 0.10 g,2.48 ± 0.10 g and 2.49 ± 0.10 g (Fig.3 B).Based on these results,we found that Ach contraction affected stomach contraction and that the tension was the highest at an Ach concentration of 7.5 × 10−5mol/L.However,the Ach concentration at 7.5 × 10−5mol/L reached plateau response,increasing Ach concentration did not increase the stomach tension.There was no significant difference of stomach tension between 7.5 × 10−5mol/L and 10 × 10−5mol/L (P>0.05).In addition,the proximal vagal innervation of the lesser curvature was transected in IR group (OA),and the smooth muscle cells of the greater curvature were denervated,as presented in Fig.1 .These findings indicated that the greater destruction of the gastric wall vagal nerve fibers,the weaker gastric contraction.Compared with IR and ER groups,CR group had less damage of vagus nerve,more orderly broken ends of muscles,and more consistent direction of force during muscle contraction,thus producing greater tension.
Histology of the gastric wall by different excisional methods after distal gastrectomy in patients underwent PD
To investigate whether the interruption of smooth muscle cells at the cut edge of the remnant stomach after distal gastrectomy differed as the excisional lines varied,we examined the gastric wall of patients in CR and IR groups.In gastric specimens,HE staining analyses confirmed that the numbers of circular smooth muscle bundles transected in IR group were much higher than those in CR group (8.24 ± 0.65 vs.3.76 ± 0.70,P<0.05) (Fig.4 A-D).Conversely,fewer longitudinal smooth muscle bundles were damaged in IR group than in CR group (40.15 ± 2.63 vs.46.32 ± 9.42,P<0.05) (Fig.4 E and F).The results suggested that circular smooth muscle bundles were more important in maintaining gastric tension.
Comparison of patient demographics and perioperative status
The patient demographics and preoperative data in CR and IR groups are shown in Table 1 .No significant difference was found between the two groups about age,sex,body mass index,the presence of diabetes mellitus,preoperative nutritional biochemical parameters,pancreatic endocrine and exocrine function and type of disease (benign or malignant).The duration from disease presentation to operation was also not significantly different between the two groups.
Operative outcomes,including operative time,blood loss,soft pancreas,incidence of blood transfusion,and lymph node dissection,were similar between the two groups (Table 2).Six patients underwent extended lymphadenectomy in pancreaticoduodenectomy in IR group,and 5 patients in CR group.
The overall incidence of DGE was 12.6% (22 of 174 patients)(Table 3).The DGE grades of these patients were as follows:A in 8 patients,B in 10 and C in 4.In CR group,the incidence of DGE was 3.5% (3 of 85 patients),and the grades were A in 2 patients,B in 1.In IR group,the incidence of DGE was 21.3% (19 of 89 patients),and the grades were A in 6 patients,B in 9 and C in 4.The incidence of DGE was significantly higher in IR group than in CR group(21.3% vs.3.5%,P<0.001).The incidence of clinically relevant DGE(grades B and C) was 1.2% (1 patient) in CR group and 14.6% (13 patients) in IR group (P<0.001).
Other postoperative clinical data
Table 4 showed other postoperative clinical data in the two groups.No significant difference was observed between the groups in terms of the length of hospital stay,the incidence of wound infection,the duration of gastroenterostomy,POPF,biliary leakage,abdominal abscess,cholangitis,postoperative hemorrhage,anastomostic bleeding,pulmonary infection.One patient in CR group died of multiple organ failure.Postoperative prokinetic use was much higher in IR group than in CR group (31.5% vs.4.7%,P=0.001) because of more cases of DGE in IR group.The overall rate of pancreatic fistula in this study was 7.5% (13 of 174 patients).Of the 13 patients,7 were classified as grade A (4.0%),6 grade B(3.4%).In addition,three cases in IR group and one in CR group were readmitted due to poor gastric function.
Discussion
In this study,we demonstrated in rat that the remnant stomach had greater tension after complete resection than after incomplete or expanded resection of the gastric antrum and the contraction tension of the remnant stomach was related to Ach concentration.In our study,human gastric wall by different excisional methods after distal gastrectomy analyses showed that fewer circular smooth muscle cells were transected in CR group than in IR group.Finally,compared with incomplete gastric antrum resection,the incidence of DGE after gastric antral resection was significantly reduced in CR group.These results demonstrated the importance of gastric smooth muscle injury in DGE after PD.

Fig.4.Hematoxylin-eosin staining of human gastric specimens.Representative images of the different interruptions of smooth muscle cells at the cut edge of the remnant stomach after distal gastrectomy using the methods applied to the CR and IR groups.A and B showing the full thickness of the gastric wall (original magnification × 100).C and D showing circular smooth muscle bundles for the CR and IR groups,respectively (original magnification × 200).E and F showing longitudinal smooth muscle bundles for the CR and IR groups,respectively (original magnification × 200).
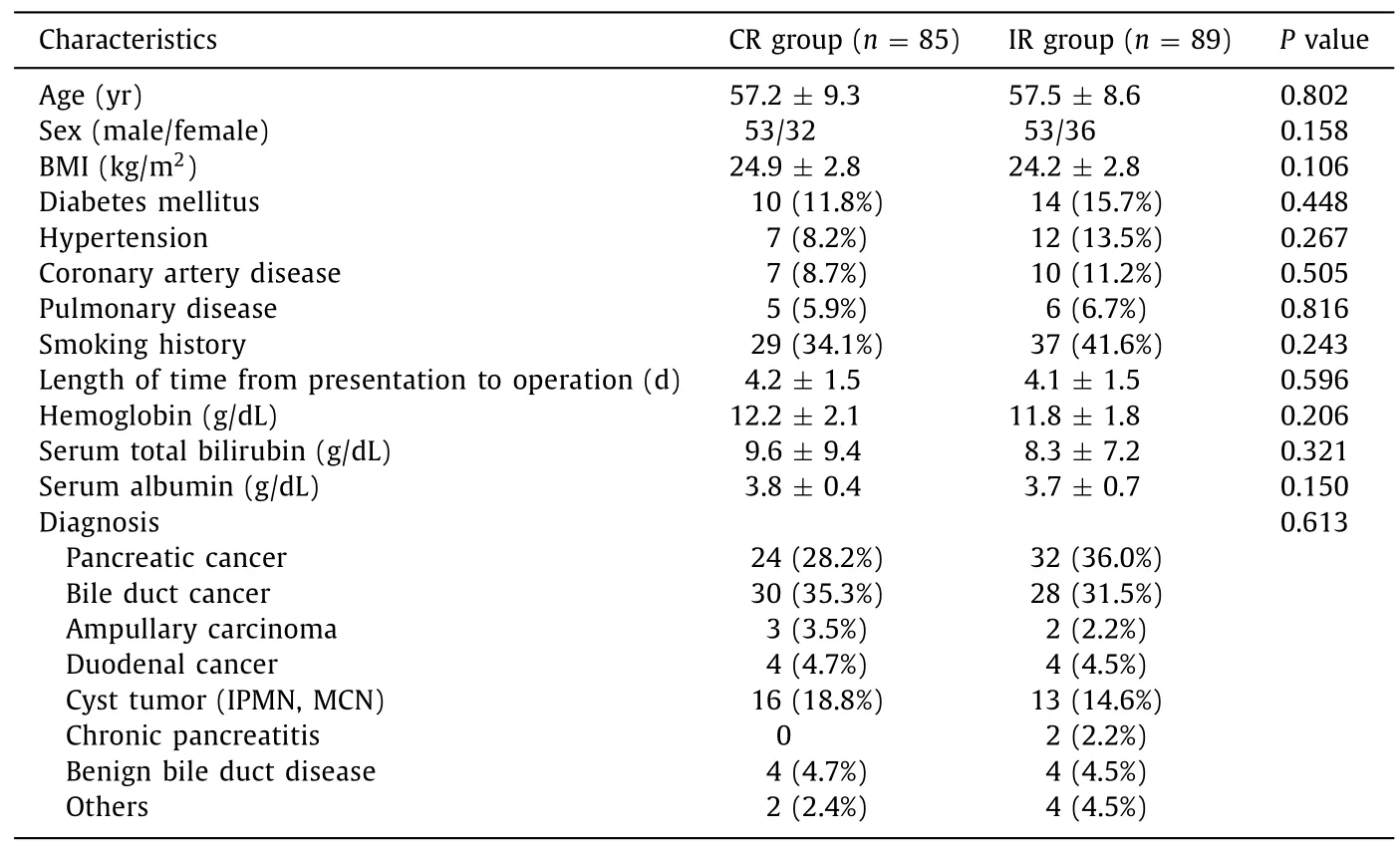
Table 1 Characteristics of patients.
Table 2 Operative parameters of the patients in two groups.

Table 3 The incidence of DGE in CR and IR groups.
Recently,reducing the incidence of DGE after PD has been the focus for surgeons.It has been discovered that pylorus ring resection PD could reduce the incidence of DGE compared with PPPD [21].Other studies demonstrated that the antecolic routeof duodenojejunostomy reduces DGE after PPPD [ 22,23 ].However,another study argued that the route of gastroenteric reconstruction after PD does not influence the postoperative incidence of DGE [24].Some surgeons have even hypothesized that the use of a stapler has advantages in decreasing the incidence of DGE compared with the hand sewing of anastomosis in PD [25].

Table 4 Postoperative complications of the 174 patients.
These conflicting results mean that more attention should be paid to the underlying mechanism of DGE after PD,which preferably based on a multidisciplinary approach including gastroenterological motility [24].Resection of the duodenum could be a factor for DGE because this removal decreases level of motilin,which speeds gastric emptying [ 26,27 ].Other potential causes of DGE include mechanical obstruction from torsion or angulation of the small bowel after reconstruction [28].Although various theories have been proposed,the precise mechanism of DGE after PD is not well known.
Gastric motility is regulated by a series of coordinated events influenced by autonomic nervous system,smooth muscle cells and intestinal neurons.Any interference of these control pathways may lead to DGE or gastric stasis [8].Smooth muscle cells are responsible for the contraction of the whole stomach,and the intestinal nervous system provides the stimulation of the patterned electrical activities and synaptic connections of smooth muscle cells [29].The combination of vagotomy,distal gastric resection,and gastrojejunostomy predisposes the patient to slow emptying of the gastric remnant [30].In the musculature of the stomach wall,differences of the vagal innervation in the smooth muscle decided the function of the stomach.The longitudinal muscles in the stomach are related to the special function of the stomach as a storage organ,while the circular muscles are responsible for gastric emptying [31].
The proportion of neurons receiving vagal input is highest at the lesser curvature (98%) and decreased gradually towards the greater curvature.In addition,the cell bodies of the circular muscle motor neurons are more frequently located in the lesser gastric curvature and project from greater gastric curvature [32].In this study,the use of different excisional methods for distal gastrectomy resulted in different contraction patterns in rat.Incomplete resection of the gastric antrum perhaps resulted in transection of vagal fibers of the lesser gastric curvature.Meanwhile,the smooth muscles of the remnant gastric antrum in the greater gastric curvature were denervated.Simultaneously,we found that the number of the circular smooth muscle bundles transected in IR group were higher than those in CR group.Conversely,fewer longitudinal smooth muscle bundles were damaged in IR group.These factors greatly decreased peristaltic ability in the remnant gastric antrum,even causing atony.Therefore,incomplete resection of the gastric antrum is more likely to cause DGE.Nevertheless,CR group had a much lower incidence of DGE after PD than IR group.These differences may be due to different extents of damage to circular smooth muscle.
During normal cycles,wave fronts are oriented orthogonally to the gastric curvatures and propagate along the longitudinal organ axis [33].In addition,the leading edges of the active slow-wave fronts in the corpus and antrum are oriented perpendicular to the central axis of the stomach;thus,the slow-wave activity is organized as a circumferential band propagating in the organoaxial direction (down the longitudinal axis of the organ) towards the pylorus [34].Therefore,the vertical excision to the longitudinal axis required for the complete resection of the gastric antrum is beneficial for gastric emptying.Otherwise,the superfluous gastric antrum in the greater curvature causes the conduction and contraction to lose coordination with that of the lesser curvature,which would affect gastric emptying.
Human gastric electrophysiological research proposed that antral slow-wave propagation is continuous with corpus wave propagation.However,the amplitude and velocity of slow wave activity changed significantly in the antrum,and multiple wave fronts propagated in the direction of the organic axis [34-36].Previous studies [ 37,38 ]showed that damage to the nerves and smooth muscle might cause gastric dysrhythmia.Abnormal slowwave activity promoted motility disorders,and slow waves accorded with gastric motility.In a study of gastroparesis,aberrant slow-wave initiation commonly occurred at variable locations across the stomach;propagated retrogradely,causing wave collisions;and was more pronounced when the initiation sites were more distal,diffuse,or irregular [ 33,39 ].Further research indicated that abnormal slow-wave initiation occurs across a wide range of frequencies and occurs more frequently in the gastric antrum than in the corpus [33].These results demonstrate that gastric antrum might act as an independent unit of the stomach.In the present study,we performed complete resection of the gastric antrum;the possible motility disorders induced from ectopic slow-wave initiation were eliminated,and the patients developed much fewer instances of DGE than patients with incomplete resection of the gastric antrum.Therefore,gastric dysrhythmia,ectopic slow-wave initiation and abnormal slow-wave activity are probably the mechanisms underlying DGE after PD.
In addition,previous studies have suggested that mechanical torsion and angularity of gastrojejunostomy could cause DGE following PD [ 40,41 ].In the present study,we successfully avoided possible torsion and angularity in the anastomosis between the stomach and jejunum due to the use of a suitable excisional direction.Thus,this anastomosis was adapted to food emptying by gravity,which is an important factor of DGE.
In this study,we retrospectively analyzed clinical data and inferred the possible mechanism of DGE following PD.Our animal data and clinical analyses indicated that complete resection of the gastric antrum greatly decreases the incidence and severity of DGE after PD.According to these results,we propose that the possible mechanisms underlying DGE include (i) the disruption of vagal innervation and gastric smooth muscle,leading to weakened contraction;(ii) gastric dysrhythmia and ectopic slow-wave initiation causing motility disorders of the stomach;(iii) remnant gastric antrum decreasing peristalsis,greatly leading to gastric atony;(iv)the loss of coordination of conduction and contraction between the greater curvature and the lesser curvature affecting gastric emptying;and (v) adapting the gastrointestinal anastomosis to food emptying by gravity.However,because of the lack of efficient and prospective clinical methods,further research is needed for confirming our suggestion.
Acknowledgments
None.
CRediT authorship contribution statement
Yu-Ling Sun:Conceptualization,Funding acquisition,Project administration,Writing -original draft,Writing -review &editing.Jian-Jun Gou:Investigation,Methodology,Writing -review &editing.Kai-Ming Zhang:Data curation,Writing -original draft.Wen-Qi Li:Formal analysis,Software,Writing -review &editing.Xiu-Xian Ma:Resources,Writing -review &editing.Lin Zhou:Resources,Writing -review &editing.Rong-Tao Zhu:Writing -review &editing.Jian Li:Software,Writing -review &editing.
Funding
This study was supported by a grant from the National Natural Science Foundation of China (No.81870457).
Ethical approval
This study was conducted with approval from the Ethics Committee of Zhengzhou University (2016062).And this study protocol was approved by the Laboratory Animal Care and Use Committee of Zhengzhou University.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Practice of precision surgery in primary liver cancer
- Reporting of longitudinal pancreatojejunostomy with partial pancreatic head resection (the Frey procedure) for chronic pancreatitis:A systematic review
- Hepatobiliary&Pancreatic Diseases International
- Presentation and surgical management of xanthogranulomatous cholecystitis
- Transjugular intrahepatic portosystemic shunt is effective in patients with chronic portal vein thrombosis and variceal bleeding
- Long-term follow-up of HCV patients with sustained virological response after treatment with pegylated interferon plus ribavirin