Laparoscopic hepatectomy is superior to open procedures for hepatic hemangioma
2021-05-19ChenYnBingHuLiXiTiSunDeCiYu
Chen Yn ,Bing-Hu Li ,Xi-Ti Sun ,De-Ci Yu ,∗
a Department of Hepatobiliary Surgery, Nanjing Drum Tower Hospital, The Affiliated Hospital of Nanjing University Medical School, Nanjing 210 0 08, China
b Department of General Surgery, Taikang Xianlin Drum Tower Hospital, The Affiliated Hospital of Nanjing University Medical School, Nanjing 210046, China
Keywords:Hepatic hemangioma Open hepatectomy Laparoscopic hepatectomy Prognosis
ABSTRACT Background: Laparoscopic hepatectomy (LH) has become increasingly popular for liver neoplasms,but its safety and effectiveness remain controversial.Hepatic hemangiomas are the most common benign liver neoplasm;the main approaches to hepatic hemangiomas include open hepatectomy (OH) and LH.In this study,we compared early outcomes between patients undergoing OH and those with LH.Methods: Patients underwent OH or LH in our hospital for hepatic hemangiomas between December 2013 and December 2017 were enrolled.All patients underwent comprehensive preoperative evaluations.The clinicopathological index and risk factors of hemangioma resection were assessed.Results: In total,41 patients underwent OH while 53 underwent LH.There was no significant difference in any preoperative clinical variables,including liver function,prothrombin time,or platelet count.Hepatic portal occlusion time and operative time were 39.74 vs.38.35 minutes (P=0.717) and 197.20 vs.203.68 minutes (P=0.652) in the OH and LH groups,respectively.No mortality nor significant perioperative complications were observed between the two groups.In LH group,two cases were converted to OH,one for an oversized tumor and the other for hemorrhage.Compared with OH patients,those with LH had less blood loss (361.69 vs.437.81 mL,P=0.024),shorter postoperative hospital stay (7.98 vs.11.07 days,P=0.001),and lower postoperative C-reactive protein (43.63 vs.58.21 mg/L,P=0.026).Conclusions: LH is superior to OH in terms of postoperative recovery and blood loss for selected patients with hepatic hemangioma.
Introduction
Hepatic hemangioma is the most common benign neoplasm of the liver;it is often asymptomatic and discovered incidentally [1].It is a slow-growing,indolent neoplasia that can occur in all ages,and is more frequent in females.Hormone treatments,especially estrogen as a contraceptive or replacement treatment for menopausal disorders,are associated with hepatic hemangiomas.The prevalence of hepatic hemangiomas ranges from 0.7% to 7%,and up to 20% in autopsied cases [2,3].Most hemangiomas are asymptomatic and require no treatment.However,as the tumor grows,it may become symptomatic,with a sensation of fullness,loss of appetite,and right epigastric discomfort.Clinically,giant hemangiomas are defined as those measuring greater than 5 cm in diameter [4].Therapies for hemangiomas include enucleation,hepatectomy,radiofrequency ablation,and hepatic artery embolization/ligation.Based on clinical results,resection is the most effective treatment [5].
The main surgical procedures for hepatic hemangiomas are open hepatectomy (OH) and laparoscopic hepatectomy (LH).Conventional OH for hepatic hemangioma is traumatic and has some complications [6,7].With the recent progress in laparoscopic techniques and instruments,laparoscopic surgery has gradually supplanted traditional open surgery in some areas [8].However,laparoscopic techniques are challenging to apply in patients with liver disease [9].Several factors may hinder the implementation of LH,such as tumor-free margins,bleeding control,difficult tumor location,and parenchymal transection [10].Several studies [11–13]demonstrated the advantages of LH over OH in terms of blood loss,postoperative morbidity,and hospital stay.
In this study,we compared the surgical outcomes of patients who had OH with those of patients who had LH in our department.It is speculated that LH may not differ from OH,and will probably become the gold standard technique for hepatic hemangiomas.
Methods
Clinical setting and patient enrollment
This was a single-center retrospective study.All patients with hepatic hemangiomas treated from December 2013 to December 2017 at our department were recruited,and all hepatic hemangiomas were diagnosed using contrast-enhanced computed tomography (CT) or magnetic resonance imaging (MRI) before hepatectomy.Patients who underwent other therapies simultaneously were excluded.Patients from 2013 to 2015 (n=41) served as the OH group,and those from 2016 to 2017 (n=53) served as the LH group.This study was approved by the Institutional Review Board of the Nanjing Drum Tower Hospital (2018-085-01).Data collection and analysis followed the institutional guidelines,which conform to the ethical standards oftheDeclarationofHelsinki.During the study,clinical and laboratory data were collected,including age,sex,number and size of tumors,prothrombin time,platelet count,and preoperative liver function.Parameters related to the operation were analyzed,such as operation difficulty,operative time,hepatic portal occlusion time,estimated blood loss,postoperative hospital stay,postoperative liver function,and C-reactive protein (CRP).
Perioperative management
Before surgery,all patients underwent liver and kidney function tests,routine blood tests (including clotting function),and an electrocardiogram.Those aged over 60 years also underwent cardiac ultrasonography and pulmonary function tests.
A simple,practical scoring system [14]was used to evaluate the surgical difficulty based on the total points for tumor location,extent of hepatectomy,tumor size,proximity to major vessels,and liver function.The tumor locations S2,S3,S4,S5,S6,S7,and S8 correspond to scores of 2,1,3,3,2,5,and 5,respectively.The type of hepatectomy was scored as follows:partial resection,0;left lateral sectionectomy,2;segmentectomy,3;and not less than a sectionectomy,4.If the tumor was<3 cm,it was scored as 0;otherwise,it was scored as 1.When the tumor was near a major vessel,it was scored as 1;otherwise it was scored as 0.For factor in preoperative liver function,Child-Pugh A and B were scored as 0 and 1,respectively.
The liver was transected with an ultrasonic scalpel.The Pringle maneuver was performed during liver transection to control intraoperative blood loss if necessary.In the OH group,exploratory surgery was performed via a 25 cm incision at approximately the right mid-upper abdomen line.In the LH group,the patient was placed in the supine position for a left or middle hepatectomy or the left recumbent position for right posterior or right hepatecomy.The senior surgeon stood on the left side of the patient,and two assistants stood on either side of the patient.Pneumoperitoneum was created with a pressure of 12–14 mmHg.Six trocars were used in all procedures:three 12 mm ports and three 5 mm ports.The trocar positions were determined by the type of operation and tumor location (Fig.1).During hepatectomy,a 12 mm trocar was placed in the umbilicus (port S) for introducing a 10 mm,30 ° angled laparoscopes.One 12 mm trocar (port C) was inserted into the right midclavicular line parallel to the umbilicus.One 5 mm trocar (port D) was inserted into the right anterior axillary line.Ports C and D were used by the assistants.One 5 mm trocar (port P;Nelaton catheter with vessel tape) was used for the Pringle maneuver.Ports A (12 mm) and B (5 mm) were used by the operator.For left hepatectomy,port A is on the left midclavicular line just below the costal margin and port B is 5 cm along the left of the midabdominal line above umbilicus.For right hepatectomy or right posterior sectionectomy,port A is 2 cm to the left of the midabdominal line below the costal margin;port B is midpoint betweenthe xiphoid process and umbilicus.For a mesohepatectomy,port A is 2 cm below the xiphoid process and port B is midpoint between the xiphoid process and umbilicus [15].
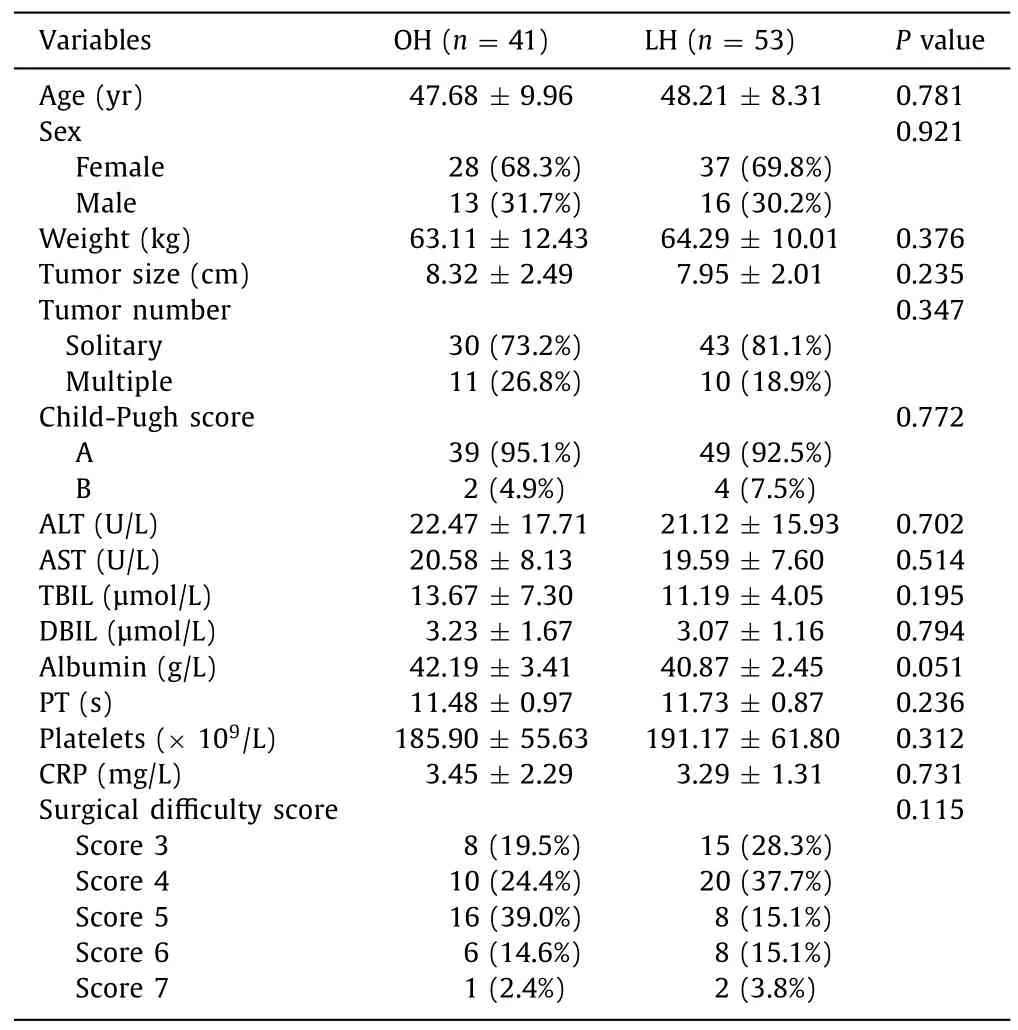
Table 1 Preoperative clinical characteristics of the patients undergoing OH or LH.
We implemented Glissonian approach combined with dorsal approach for LH;the surgical procedure was as follows.The ligaments were divided,such as the falciform,left,or right coronary ligaments to expose the left,right,and middle hepatic roots.Then,the Arantius duct was divided to expose the dorsal aspect of the left or middle hepatic vein.A tourniquet was placed for Pringle maneuver.Glissonian approach served to isolate and dissect the hepatic pedicles corresponding to the tumor resection.The liver parenchyma was transected through a dorsal approach along the demarcated plane and the corresponding hepatic vein,and then along the demarcated plane through ventral approach.Finally,we dissected the vein root,extracted the specimen,and performed hemostasis and drainage.
Statistical analysis
Statistical analyses were performed using SPSS for Windows software (version 22.0;SPSS Inc.,Chicago,IL,USA).Data were expressed as percentage,or as mean ± SD.Continuous variables were compared using Student’st-test;categorical variables were compared using the Chi-square test or Fisher’s exact test as appropriate.APvalue<0.05 was considered statistically significant.
It was a minor2 surgical3 procedure. Laparoscopic. Nothing serious. He seemed to come through it fine and would be home the next day. One more day, I thought while getting ready for bed.
Results
Therewasnosignificantdifferenceinpatientdemographicsbetween OHandLH

Fig.1.Trocar placement for laparoscopic hepatectomy.Capital letters served as one trocar.S:1st port is mainly used as a camera port;A,C:12 mm port;B,D:5 mm port;P:a Nelaton catheter with vessel tape inside Pringle maneuver was directly inserted through this 5 mm port size hole.The operator mainly used A and B,and the assistants used C and D.

Table 2 Intraoperative clinical index of the patients undergoing OH or LH.
This study included 94 patients with 41 for OH group and 53 for LH group.Two (3.77%) LH patients were converted to laparotomy:one for bleeding control and the other for the big size tumor.The baseline characteristics of the OH and LH groups were summarized in Table 1 .The mean patient age was 47.95 ± 9.01 years and 65 (69.1%) patients were women.There were no significant differences between the two groups in age,sex,weight,tumor size or number,alanine aminotransferase (ALT),aspartate aminotransferase (AST),total bilirubin,direct bilirubin,serum albumin,prothrombin time,platelet count,nor preoperative CRP(P>0.05).Also,the surgical difficulty score did not differ significantly (P>0.05).
LH has much better early outcomes than OH for hepatic hemangioma
In the OH group,the patients underwent different sur gical procedures,including 15 (36.59%) partial resections or segmentectomies,5 (12.20%) left lateral sectionectomies,3 (7.32%) sectionectomies excluding the left lateral section,16 (39.02%) bisectionectomies or hemihepatectomies,and 2 (4.88%) trisectionectomies,while the above mentioned procedures were performed in the LH group with 7 (13.21%),20 (37.74%),7 (13.21%),18 (33.96%),and 1 (1.89%) patients,respectively (Table 2).The perioperative outcomes of the two groups were also summarized in Table 2 .The mean operative time was 197.20 and 203.68 minutes,respectively(P=0.652);the mean hepatic portal occlusion time was 39.74 and 38.35 minutes,respectively (P=0.717);and the average estimated blood loss was 437.81 and 361.69 mL,respectively (P=0.024).
The postoperative index was summarized in Table 3 .The ALT,AST,total bilirubin,and direct bilirubin levels the day after hepatectomy did not differ between the two groups (P>0.05).However,postoperative hospital stay was shorter in the LH group(7.98 ± 2.94 vs.11.07 ± 9.51 days;P=0.001).The postoperative CRP in the LH and OH groups was 43.63 ± 15.35 and 58.21 ± 18.74,respectively (P=0.026).Postoperative complications occurred infour (7.55%) in the LH group and three (7.32%) patients in the OH group (P=0.248).The complications included bile leakage (n=2),incision fat liquefaction (n=1) or incision infection (n=1) in the LH group,and bile leakage (n=1) or incision infection (n=2)in the OH group.Three cases of bile leakage were resolved after 4 weeks with complete drainage.No perioperative mortality occurred after the 6-month follow-up.
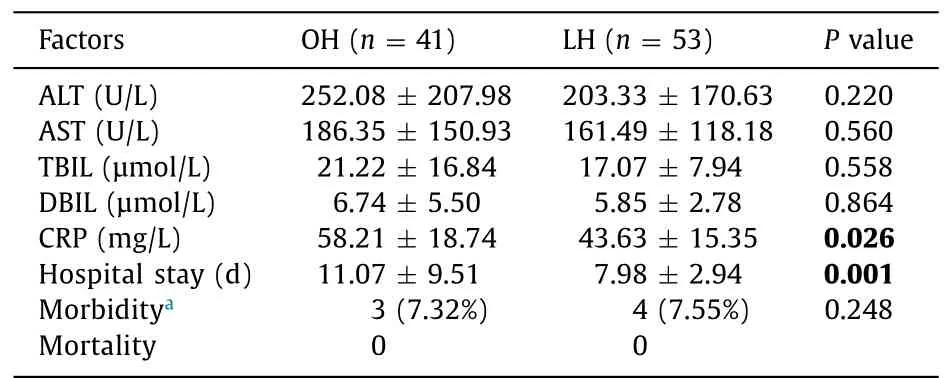
Table 3 Postoperative clinical index of the patients undergoing OH or LH.
Discussion
Although hepatic hemangiomas are usually asymptomatic,they may be accompanied by early satiety,nausea,or abdominal pain due to pressure on the liver capsule or adjacent organs [9,16].When a hepatic hemangioma is symptomatic,surgical resection is the optional therapy [17,18].To obtain a good operative view,surgeons frequently select a 25–30 cm long L-shaped right upper abdominal incision;the right rectus often needs to be cut.A large incision also causes great trauma.Several studies reported increasing recovery time and high morbidity rates with OH or enucleation [7,11,13].
In the last two decades,laparoscopic surgery has become widely accepted as a feasible alternative to traditional open procedures [19].However,LH remains one of the last procedures to be fully implemented in laparoscopic surgery [20].Several factors have hindered the popularity of LH,including (i) the technical demands associated with parenchymal resection;(ii) the difficulty exposing tumors,especially tumors of segments VI–VIII;(iii) the difficulty of determining tumor-free margins;and (iv) the possibility of uncontrolled bleeding.Bleeding control is the challenging procedure during LH because pressure hemostasis cannot be used.Once bleeding starts,it is often difficult to control despite clamping of the hepatic vein,hepatic artery,or portal vein.However,with technological innovation and increasing experience,LH has emerged as an option for liver neoplasms,hepatic hemangiomas,or hepatolithiasis at major tertiary care centers [21,22].
Most studies of the learning curve effect showed improved outcomes with increasing experience;such studies aimed to identify the number of procedures to overcome the learning curve effect [23–25].We first performed an LH in 2009,beginning with a minor LH,but were also very experienced in open liver surgery at the same time.With increasing experience with LH,we extended our indications for LH from peripherally located tumors to posterosuperior lesions and from wedge to major resections.Bearing in mind the diverse operative techniques for various types of LH,more experience is needed to overcome the learning curve [26].
In this study,no significant difference in preoperative indicators was found between the LH and OH groups,which was consistent with the previous research [27].Yu et al.[27]also demonstrated that there was no significant difference in estimated intraoperative blood loss between the LH and OH groups,but the operative time of the LH group was longer than that of the OH group.However,in our study,the estimated blood loss in the LH group was significantly less compared with the OH group.However,the mean operative time did not differ between the two groups.We found that laparoscopy enables a clear operative field and a magnified local view,which ensures that the blood vessels can be well identified.Under the laparoscopic view in pneumoperitoneum,veinlets can be occluded.In our study,the postoperative hospital stay was shorter in the LH group compared with that in the OH group.Our results are in accordance with the reports showing the advantages of LH over OH in terms of blood loss and hospital stay [13,28–30].In addition,morbidity and mortality did not differ between the groups,which constitute more evidence for the safety and feasibility of laparoscopic major hepatectomy.
The ALT and AST levels are the biomarkers of liver injury.Several factors interact in complex ways to influence the ALT and AST levels,including the extent of hepatectomy,intraoperative stretching and compression of the liver,and injury due to the thermoelectric effect of high-frequency electrosurgery on the bile ducts.In our study,the ALT and AST levels did not differ between the LH and OH groups.CRP is an acute-phase plasma protein that is synthesized by hepatocytes after infection or trauma [31].As a biochemical marker of the acute systemic inflammatory response,CRP is also closely related to surgery.Spath et al.[32]found that CRP is a negative predictor of infectious complications in the first postoperative week after major elective upper gastrointestinal surgery.Adamina et al.[33]reported the negative predictive value of the serum CRP concentration at day 4 after surgery for excluding postoperative infectious complications.We found no significant difference in preoperative CRP between the LH and OH groups,while the postoperative CRP was significantly higher in the OH group.Increasing CRP after OH was attributed to the surgical trauma associated with OH.
Many surgeons are reluctant to perform LH in patients with giant hemangiomas because of the risk of bleeding [34].With the development of interventional radiology,transcatheter arterial embolization (TAE) has become a viable alternative to surgery.Recent studies have used TAE alone to treat cavernous hepatic hemangiomas successfully [35–37].However,most reports used TAE to convert inoperable hemangiomas into operable one [38,39].In our study,two hemangiomas in the LH group were over 18 cm in diameter and no TAE was performed preoperatively;one was located in the left liver lobe far from the intermediate hepatic vein,so we performed LH directly with success,and the other,located in the right lobe,was difficult to expose so conversion to open surgery was performed without delay.However,the estimated blood loss was low,the operative time was not prolonged,and the postoperative recovery was normal.Therefore,the patients with giant hemangiomas may undergo LH.Meanwhile,literatures also demonstrated that giant hemangiomas can be performed entirely by laparoscopic surgery [40,41].
There were several limitations to our study.First,these cases were treated by two different surgeons,where the operative time and estimated blood loss are influenced by the surgeon’s skill.Moreover,this study was conducted in a single institution and the results might not be comparable to those obtained in other centers.Another limitation is that this was a retrospective study covering a long-time period during which the surgical technique evolved;this may have affected the outcomes.
To summarize,LH results in less blood loss,shorter hospital stay and lower postoperative CRP,and also allows for quick recovery.Therefore,LH represents the future of liver surgery and will probably become the gold standard technique for selected patients with hepatic hemangiomas.As experience accumulates,LH may become the first-line therapy for hepatic hemangioma.
Acknowledgments
We thank Mr.Ya-Wen Zhu for drawing the schemas (Fig.1).
CRediT authorship contribution statement
Chen Yan:Data curation,Investigation,Writing -original draft.Bing-Hua Li:Formal analysis,Software,Validation.Xi-Tai Sun:Methodology,Resources,Supervision.De-Cai Yu:Conceptualization,Funding acquisition,Writing -review &editing.
Funding
This study was supported by grants from the National Natural Science Foundation of China (81201621 and 81372455) and Key Clinical Departments and Outstanding Physicians in Jiangsu Province.
Ethical approval
This study was approved by the Ethics Committee of Nanjing Drum Tower Hospital (2018-085-01).Written informed consent was obtained from all participants.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Practice of precision surgery in primary liver cancer
- Reporting of longitudinal pancreatojejunostomy with partial pancreatic head resection (the Frey procedure) for chronic pancreatitis:A systematic review
- Hepatobiliary&Pancreatic Diseases International
- Presentation and surgical management of xanthogranulomatous cholecystitis
- Transjugular intrahepatic portosystemic shunt is effective in patients with chronic portal vein thrombosis and variceal bleeding
- Long-term follow-up of HCV patients with sustained virological response after treatment with pegylated interferon plus ribavirin