The robot-assisted ureteral reconstruction in adult: A narrative review on the surgical techniques and contemporary outcomes
2021-03-26KultheRmeshSeethrmBhtMrcioCovsMoschovsVipulPtelYoungHwiiKo
Kulthe Rmesh Seethrm Bht , Mrcio Covs Moschovs Vipul R.Ptel Young Hwii Ko
a Department of Urology, AdventHealth Global Robotics Institute, Celebration, FL, United States
b Department of Urology, Yeungnam University, Daegu, Republic of Korea
Abstract Despite the rapid increase in the use of robotic surgery in urology,the majority of ureteric reconstruction procedures are still performed using laparoscopic or open approaches.This is primarily due to uncertainty regarding the advantages of robotic approaches over conventional ones,and the unique difficulty in identifying the specific area of interest due to the lack of tactile feedback from the current robotic systems.However,with the potential benefits of minimal invasiveness,several pioneering reports have been published on robotic surgery in urology.By reviewing the literature on this topic,we aimed to summarize the techniques,considerations,and consistent findings regarding robotic ureteral reconstruction in adults.Robotic applications for ureteral surgery have been primarily reported for pediatric urology,especially in the context of relieving a congenital obstruction in the ureteral pelvic junction.However,contemporary studies have also consistently demonstrated that robotic surgery could be a reliable option for malignant,iatrogenic,and traumatic conditions,which generally occur in adult patients.Nevertheless,the lack of comparative studies on heterogeneous hosts and disease conditions make it difficult to determine the benefit of the robotic approach over the conventional approach in the general population;thus,qualified prospective trials are needed for wider acceptance.However,contemporary reports have demonstrated that the robotic approach could be an alternative option for ureteral construction,even in the absence of haptic feedback,which can be compensated by various surgical techniques and enhanced three-dimensional visualization.
KEYWORDS Robotic reconstructive surgery;Ureteric reconstruction;Surgical techniques;Robotic pyeloplasty
1.Introduction
The widespread use of robotic surgery has motivated urologists to apply robotics in typical surgical settings where open and laparoscopic approaches have long been the standard of care [1].Ureteral reconstruction encompasses a wide spectrum of diseases with different etiologies,including iatrogenic, congenital, and malignant conditions,across the upper and lower ureter, each requiring unique approaches for surgical correction.Owing to their minimal invasiveness and high dexterity, robotic ureteral reconstruction procedures for the upper tract were initially applied in the field of pediatric urology.As such, there are limited data on the outcome of robotic surgery for the repair of the upper urinary tract in adults.
In the case of lower ureteral disease, there has been increasing interest regarding robotic ureteral surgery as a kidney-sparing procedure for distally located upper tract urothelial carcinoma(UTUC),including distal ureterectomy and segmental ureterectomy [2].Both procedures,concomitant with or without a psoas hitch or Boari flap,are recommended in recently available guidelines as reliable alternatives to replace the standard radical nephroureterectomy [3].Nevertheless, the lack of comparative studies based on heterogeneous conditions makes it difficult to perform a meta-analysis and establish a solid conclusion on the unique benefit of the robotic approach over the open approach and conventional laparoscopy in the general population.Thus, by reviewing contemporary published articles, we sought to establish consistent findings regarding robotic ureteral reconstruction in adult patients.Given the retrospective,single-arm design of the majority of reported studies, we also aimed to investigate the feasibility and benefit of robotic surgery in different etiologies and provide a summary of the suggested surgical techniques.
1.1.Identification of the area of interest in a robotic environment
Despite recent technological advances,the absence of tactile feedback in currently available robotic surgical systems is a significant drawback that makes it difficult to identify an area of interest[4].Therefore,conducting imaging studies before robotic ureteral procedures is a pivotal step in planning surgery.Because of the variety in the location and size of tumors in UTUC,each robotic ureteral procedure is performed in an individualized fashion.Computed tomography imaging is currently the gold standard technique for the identification and localization of the lesion.If the area of interest is narrow,pre-insertion of a ureteral catheter up to the area of interest before surgery could provide additional information.In a patient with a pre-existing percutaneous nephrostomy(PCN)tract,a ureteral access sheath can be inserted under general anesthesia,enabling the insertion of a flexible ureteroscope in an anterograde fashion.
One of the unique benefits of robotic technology is the use of indocyanine green (ICG), which can be visualized under near-infrared fluorescence(NIRF)to identify lesions.A ureteral catheter and/or a PCN tract can be used to inject 10 mL of ICG into the diseased ureter,above and below the stricture point.Intraoperatively, NIRF is activated to assist in the identification of the ureter and localize the margins of ureteral strictures [5].
1.2.General principles in patient positioning and trocar configuration
The position of the patient should be tailored according to the area of interest.In general,the patient position depends on the type of procedure and the location of the area of interest.For procedures on upper tract lesions,including the renal pelvis and upper ureter,lateral decubitus or modified decubitus position can be recommended.For procedures on lower counterparts,the patients usually placed in the dorsal lithotomy position and steep Trendelenburg position, and the robot is brought into position between the patient’s legs,as with conventional prostatectomy.In cases that require additional ureteral or bladder procedures by cystoscopy or ureteroscopy, the lithotomy position may be used, albeit with great caution, owing to possible collisions of the instrument arm with the patient’s leg or the bedside assistant.However, this conventional position limits access to the bladder, which is mandatory in many cases, especially for retrograde placement of a ureteral stent.Slater et al.[6]performed 14 distal ureteral reconstructions, including three Boari flap procedures using the da Vinci Si system,and suggested side-docking of the robotic patient cart.The da Vinci Xi series has an additional advantage that it provides a wider range of motion and minimizes external collisions between each robot arm[7].Moreover,side-docking helps to provide adequate access to the perineum, and its interchangeable camera trocars help in placing the camera in any trocar, thus providing various angles and enhancing the visualization.The latest da Vinci SP system has been demonstrated to be safe and feasible in a small single surgeon series [8,9].Trocar placement for robotic ureter reconstruction should be individualized depending on the area of interest,workload of the procedure,type of robotic system,and patient positioning.
2.Robotic pyeloplasty
Ureteropelvic junction obstruction (UPJO) is the most common condition that is treated robotically by pediatric urologists.The major case reports of adult patients are summarized in Table 1.
Anderson-Hynes pyeloplasty is considered the standard procedure of care for UPJO as it is widely applicable in different UPJO scenarios, with the exception of cases with lengthy or multiple proximal ureteral strictures and patients with anintrarenal pelvis.This procedure involves dismembering the ureter from the pelvis, excising the obstructed segment and redundant renal pelvis, and anastomosis of the ureter to the redundant pelvis after adequate spatulation.Flap procedures are particularly useful in patients with abnormal anatomy.Popular flap procedures include Foley Y-V plasty, which is usually performed for high insertion in the ureters,and Culp-DeWeerd spiral flap and Scardino-Prince vertical flap procedures for long segment proximal ureteral strictures [10,11].The key to good repair is a widely patent, watertight, tensionless anastomosis that allows dependent drainage [12].This procedure can be performed transperitoneally or retroperitoneally [13,14].Moreover, the use of the transmesenteric approach has also been described, particularly on the left side, which avoids reflection of the colon [15].
Robotic pyeloplasty has been popularized by many centers for over a decade,with success rates from 95%to 100%[16-19].However,the definition of success in each study is not identical; although the commonly applied definition of success was relief of radiologic obstruction assessed by diuretic renogram or intravenous urography, some authors also consider the absence or improvement of the symptoms as a successful outcome [10,16].
In the US, from 2003 to 2015, the number of robotic cases increased annually by 29%, with robotic pyeloplasty used in 40%of all pyeloplasty cases in 2015[20].The use of robots in redo pyeloplasty can significantly reduce surgical time, with a success rate of 100% [21].Compared to open and laparoscopic pyeloplasty, robotic pyeloplasty has been shown to have the highest operative success rate and a lower incidence of complications[22,23].A recent systemic review demonstrated that robotic pyeloplasty had a 27-min shorter operative time and 1.2-day shorter hospital stay than the laparoscopic approach stay [24].

Table 1 Summary of articles on robotic pyeloplasty in adults (n >50).
2.1.Pyeloplasty in difficult anatomy
Horseshoe kidney is the most common renal congenital anomaly and is seen in approximately 0.25% of the general population [25].One-third of horseshoe kidneys have UPJO[26],and the challenges faced in horseshoe kidneys are due to anomalous lower pole vessels, presence of a renal isthmus, and altered lower pole anatomy [26,27].The success rates of open pyeloplasty in horseshoe kidneys vary from 50%to 80%,and success rates of 78%-100%have been reported in different studies of robotic pyeloplasty in horseshoe kidneys [28-30].Furthermore, the surgical technique varies because of anatomic complexities, which further justifies the use of robots as versatile tools in the surgical management of UPJO in horseshoe kidneys.
A graft flap could be an alternative option in cases of deteriorated remnant ureteral tissue.The buccal mucosa is an excellent graft to substitute the diseased ureter, as it has a thick epithelium, thin lamina propria, and extensive blood supply that helps the process of inosculation and imbibition.Zhao et al.[31] first described robotic buccal ureteroplasty in four patients with intractable ureteric strictures, particularly ones longer than 3 cm, with a 100%success rate and a median follow-up of 15.5 months.Zhao et al.[31] pioneered the use of NIRF imaging with intravenous ICG to evaluate stricture margins.The reconstructed segment can be supported using either omental or perirenal fat, depending on the site of the strictures.Lee et al.[32] reported the largest study using buccal mucosa to repair complex ureteral stricture, with a success rate of 83.3% confirmed both clinically and radiologically.
2.2.Robotic distal ureterectomy with ureteral reimplantation
Distal ureterectomy with various ureteral reimplantation techniques was the most popularly highlighted area in robotic ureteral surgery in adults, since its first report in 2003[33].The series in this area published until the end of 2019 are summarized in Table 2.Identification of the affected ureteric segment, followed by meticulous dissection without compromising the tissue vascularity of the ureter and obtaining the maximal healthy ureteral length,are key to a successful procedure.In the cases of malignant stricture, especially by UTUC, tumor spillage can be prevented by placing a clip just above and below the affected ureter before transection of the ureter.
Among the numerous publications on robotic ureteral surgery in adults, almost all were retrospective studies from heterogeneous institutions with small sample sizes,and were focused mainly on safety and feasibility.Moreover, the definition of success was not clarified in the majority of the studies, which made comparison between techniques difficult.Nevertheless, for strictures with benign etiology, the reported success rate appears reasonable,despite the absence of long-term outcomes.In the 10 years since the first case, only a single case of anastomotic stricture has been reported[34].In the largest study of 55 patients, Fifer et al.[35] reported three cases of recurrence during short-term follow-up.Inspired by these positive results, robotic distal ureterectomy was applied for UTUC, carefully expanding its indication from pT1 to beyond pT2 disease.However, the reported tumor recurrence rate was not negligible, implying that its oncologic safety remains to be established.Among nine patients with UTUC, Glinianski et al.[36] reported five intravesical and one ipsilateral renal pelvic recurrences.Furthermore,Eandi et al.[34], McClain et al.[37], and Musch et al.[38]reported a single systemic, intravesical, and ipsilateral pelvic and bladder tumor recurrence within 3 years of follow-up.
Because a relatively small incision was required, even with an open procedure, the actual benefit of the robotic approach can be only determined using a comparative study.However, the low incidence of UTUC presents another challenge in prospectively studying the robotic approach.Three studies have retrospectively compared robotic approaches with other approaches.When comparing 10 patients with benign stricture for robotic and open approaches, Kozinn et al.[39] reported significantly reduced estimated blood loss (30.6 mL vs.327.5 mL) and lengths of hospitalization (2.4 days vs.5.1 days) in the robotic group, with similar operative time between approaches(306.6 min vs.270.0 min,p=0.130).During 24 and 30 months of follow-up, respectively, none of the patients in either group experienced a clinical or radiologic recurrence of stricture.Moreover, Isac et al.[40] compared 25 robotic cases with 41 open procedures, and reported a shorter hospital stay (3 days vs.5 days), less narcotic pain requirements (104.6 mg vs.290.0 mg) and less blood loss(100 mL vs.150 mL) with the robotic approach.Furthermore, they reported similar reoperation rates of 7.6% (robotic) vs.9.7% (open) for each group, although the followup period was approximately four times as long in the open group (11.6 months vs.44.5 months), with a significantly shorter operative time (279 min vs.200 min, p=0.0008).Elsamra et al.[41] compared 105 minimally invasive cases(20 robotic, 85 laparoscopic) with 25 open cases and demonstrated a similar trend with shorter hospital stays and less blood loss in minimally invasive approaches.However, besides the heterogeneity in procedures and follow-up periods of each study, no distinct differences were seen between the laparoscopic and robotic groups.Thus, the unique advantages of robotic approaches over conventional open or laparoscopic approaches are uncertain, despite their potential benefit of being minimally invasive.
3.Robotic Boari flap
In an attempt to cram the resected length of the affected ureter, a psoas hitch or Boari flap has been used as a component of distal ureterectomy, in which the main principle is to bridge the large gap between the healthy ureter and the bladder with a tubularized L-shaped bladder flap.A preoperatively low-capacity bladder is likely to be associated with inadequate Boari flap creation, leading to several voiding symptoms.
The first report on the use of a Boari flap in robotic ureteral reconstruction was published in 2008 for treating a benign stricture [42].The published data on robotic ureteral reimplantation using a Boari flap are summarized in Table 3.Despite the limited number of patients, the feasibility and safety of the robotic approach have been reported consistently.However, in most cases, the followup after surgery was only over 1 year, with more complications than other ureteral reconstructive procedures.Among 33 reported cases of patients with short-term outcomes, a single patient required an additional robotic procedure owing to external iliac vein injury, and two experienced anastomotic leaks [42-44].In a large study,Fifer et al.[35] reported three recurrent stricture cases within a median follow-up of 6 months,among nine cases of robot-assisted reconstruction with a Boari flap.In malignant conditions,special care with close follow-up should be provided,given that five among 33 patients had UTUC, and one of them had ipsilateral tumor recurrence within 1 year of surgery [42].
4.Robotic ureteroureterostomy
Ureteroureterostomy is the simplest way to deal with the narrowing of the affected ureter; however, it is contraindicated for long ureteral strictures that do not allow a tension-free end-to-end anastomosis.Robotic ureteroureterostomy was initially reported in 2006 for two adult patients with benign strictures, but recently gained popularity in the pediatric population (Table 4).Lee et al.[5]reported the advantages of a robotic platform in 25 pediatric patients compared with 19 patients who underwent open surgery.They showed comparable operative time,estimated blood loss, and complication rate, but the robotic group had slightly shorter hospitalization and higher rates of improved hydronephrosis or drainage in initial follow-up imaging than the open group.
Port placement for adults is usually performed in the modified flank position, which differs from that in the pediatric population [45].The first robotic ureteroureterostomy for mid-to-distally located UTUC with intermediate-term outcomes was reported by McClain et al.[37],in which two cases of robotic ureteroureterostomy for the mid ureteral tumor were performed safely with no recurrence 3 years after surgery.In a recently reported large series of 15 patients with UTUC, Campi et al.[46]reported one patient with surgical margins and three (20%)patients with ipsilateral upper tract recurrence in a median of 21 months.Robotic surgery has an advantage in that it is minimally invasive,which facilitates surgery even in fragile patients.Maximizing this potential,Raheem and colleagues[47] reported the case of an 80-year-old man with pT3 disease and severe medical co-morbidities who was successfully treated using robotic segmental ureterectomy.However, when this procedure is used for UTUC, surgeons need to consider that evidence supporting long-term oncologic outcomes is still lacking.

Table 2 Summary of articles on distal ureterectomy with reimplantation during robot-assisted ureteral reconstruction.

Table 2 (continued)
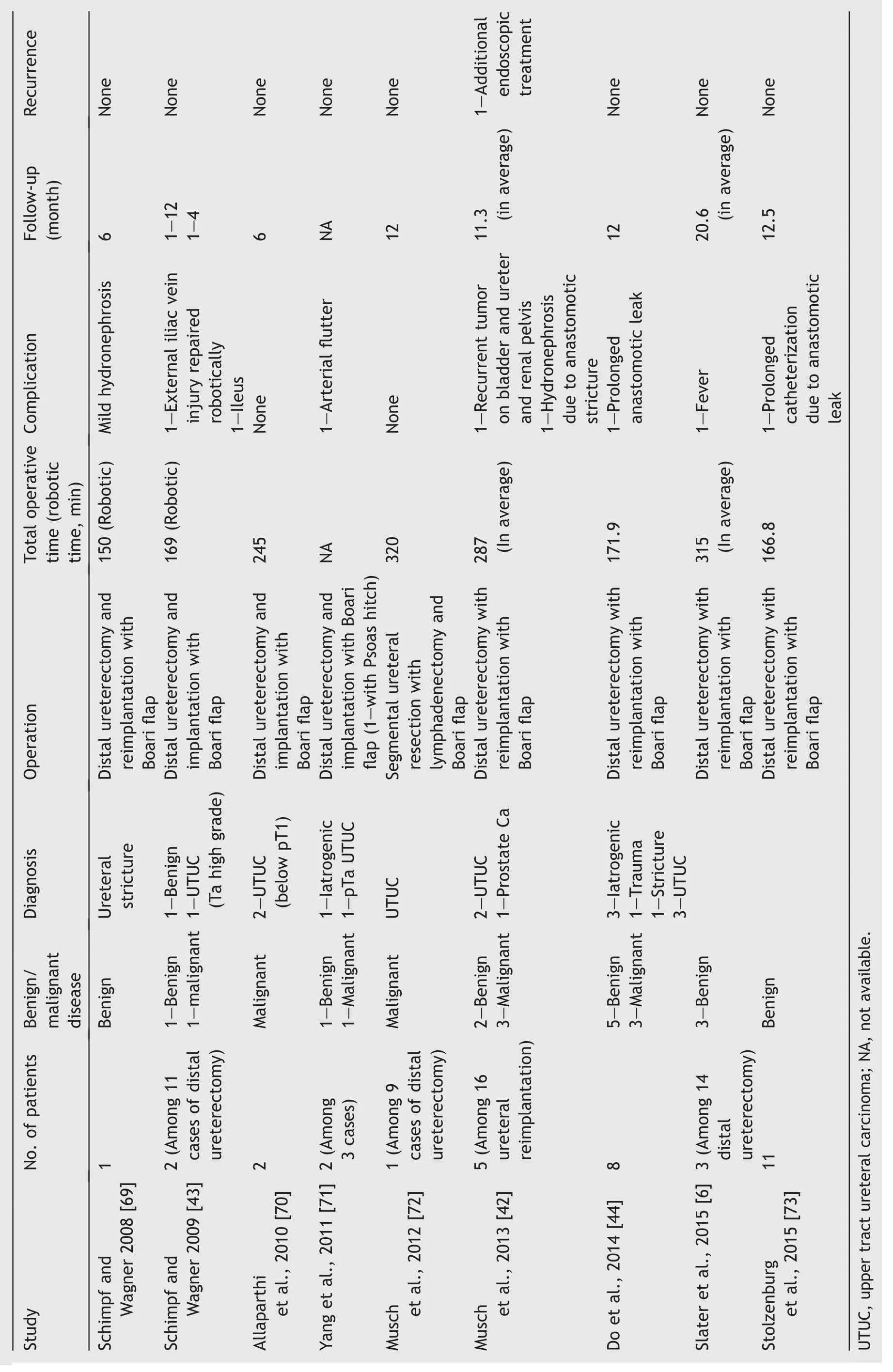
Table 3 Summary of articles on Boari flap during robot-assisted ureteral reconstruction.
Regarding benign stricture, the major concern after the procedure is recurrence of the stricture.In the largest study on using the robotic approach for cases of benign stricture, Buffi et al.[45] reported a multicenter experience of 183 men with benign strictures, including 17 who underwent ureteroureterostomy, and demonstrated a 2-year recurrence-free rate of 94.1% (n=16).While no intraoperative complications were reported, it should be noted that patients who underwent ureteroureterostomy had a higher complication rate (17.6%, n=3) than those who underwent pyeloplasty (8.3%, n=12).Although comprehensive data have not yet been reported, the first case of robot-assisted transureteroureterostomy was reported for an adult woman with bilateral congenital ureteral obstruction [48].
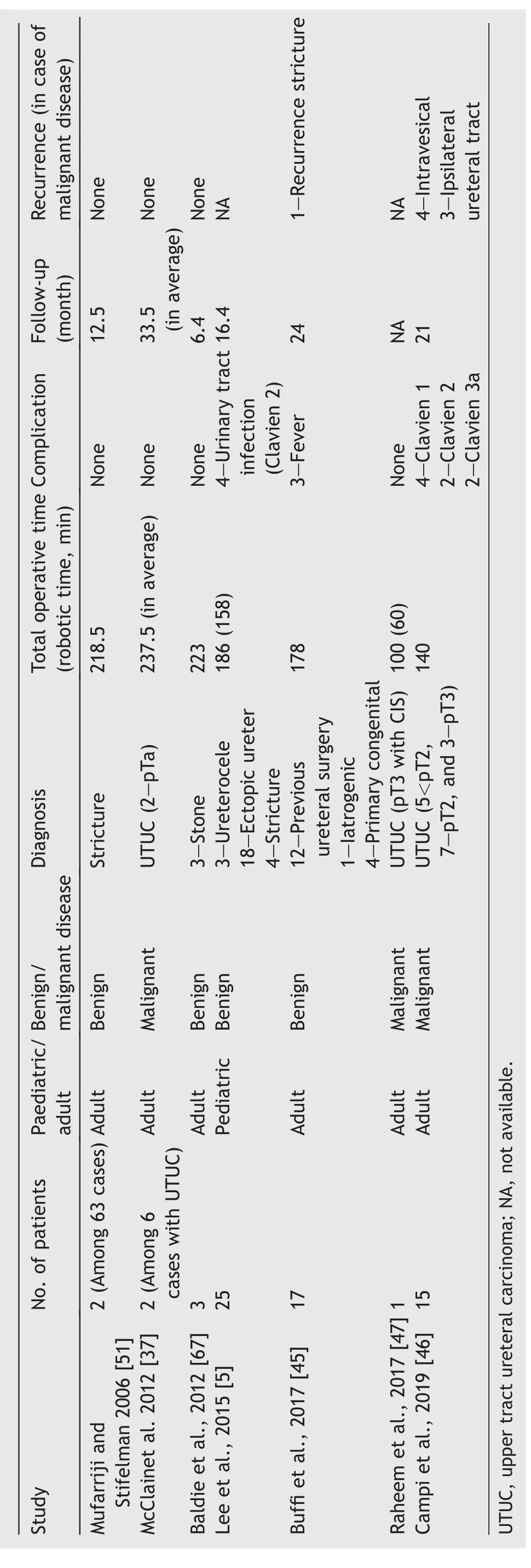
Table 4 Summary of articles on ureteroureterostomy during robot-assisted ureteral reconstruction.
5.Robotic ileal ureter substitution
Ileal ureter substitution has long been a valuable procedure and the last resort for patients with problems encompassing the entire ureter,despite recurrent repair attempts.Due to the complexity and rarity of ileal ureter substitution, open surgery has been the standard approach,as it demonstrates good and durable results.The robotic team should be adept at changing positions during the operation, and high surgical dexterity is required for success when using a robotic device in ileal ureteral substitution [49].In the reported cases, patients were first placed in a flank position to remove the affected ureter, repositioned to the supine lithotomy position to harvest an approximately 20-cm segment of the ileum (usually performed intracorporeally with an Endo-GIA stapler, with a cystotomy performed at the bladder dome after mobilization of the bladder), and finally repositioned to the original flank position for proximal pyeloileal anastomosis [50].On the left side, the harvested bowel segment is relocated behind the descending colon during the procedure by the mesenteric window to the left side.Due to these complexities and the requirement for several instances of redocking, the introduction of the daVinci Xi system,in which the surgical table can be integrated and allow change of motion without undocking the entire device, may reduce the procedure time.
Since the first report in 2008 [49], few further reports have been published (Table 5), with the initial few reporting on extraperitoneal ileal anastomosis.The first case of total intracorporeal ureteral reconstruction was reported in 2014 [50].As the experience in this approach increased, the operative time decreased; however, the reported complication rate remains high,with severe cases requiring additional procedures.

Table 5 Summary of articles on robot-assisted ileal ureteral reconstruction.
6.Robotic ureterolysis for retroperitoneal fibrosis
Retroperitoneal fibrosis is a rare condition that causes extrinsic compression of the ureter because of extensive fibrosis of the retroperitoneum from either benign or malignant conditions, although two-thirds of the cases are idiopathic.Mufarrij and Stifelman [51] described the first case of robotic ureterolysis,where in the flank position,the colon is mobilized and the entire length of the ureter is exposed.Segments encased by the fibrous capsule are released by splitting the capsule until the adventitia of the ureter is visible.Finally,the ureter is intraperitonealized by wrapping the omentum around it.Since its initial description, multiple reports of cases have been published that demonstrate the feasibility and safety of robotic ureterolysis [52,53].
7.Experimental technology and newer studies
Stem cells comprise the basic building blocks of tissue engineering, biomaterial scaffolding, and growth factor supplementation.Biomaterials used as scaffolds for inducing ureter regeneration include small intestinal submucosa,decellularized ureter, or synthetic grafts,such as Gore-Tex[54].A lack of animal models that can mimic human ureters is an important limitation that has prevented the further development of tissue engineering techniques.In addition,it is difficult to develop ureteral substitutes with peristalsis.In line with this, a collagen-based tubular scaffold with radial elasticity was recently developed by Versteegden et al.[55], which, in combination with a regenerated smooth muscle layer, was found to be ideal for restoring a neo-ureter.Moreover, the use of arteries as ureteral substitutes has also been described, as they have an intrinsic extracellular matrix ultrastructure, with collagenic composition similar to that of the ureters [56].Furthermore, venous grafts and porcine ureter grafts have also been used as scaffolds, and in some cases, may be lined with smooth muscle tissue and urothelium.In addition,Zhao et al.[57] proposed the use of extracellular matrix blood vessels with mesenchymal stem cells to bridge the ureteral graft.
8.Conclusion
While robotic applications for ureteral surgery have been reported prominently in the field of pediatric urology,especially for relieving congenital obstruction in the ureteral pelvic junction, contemporary studies across the world have consistently reported its potential for malignant, iatrogenic, and traumatic conditions, which are predominant in adults.Several pioneering reports have indicated that a robotic approach for ureteral reconstruction is both safe and feasible.However, urologists should keep in mind that robotic assistance in ureteral surgeries has been primarily reported in studies involving highly skilled surgeons, and its oncological safety for malignant etiologies remains debatable.The lack of comparative study design and low-level evidence generated from the retrospective small series without long-term follow-up makes it difficult to identify the unique advantage of the robotic approach over conventional treatment.Thus,there is a need for qualified prospective trials for wider acceptance,as well as for resolving the uncertainty regarding the advantages of robotic approaches over the conventional ones.However, contemporary reports have demonstrated that the robotic approach can be used as an alternative option for ureteral construction, even in the absence of haptic feedback, which can be compensated using various surgical techniques and enhanced three-dimensional visualization.
Author contributions
Study concept and design: Kulthe Ramesh Seetharam Bhat,Young Hwii Ko
Data acquisition: Kulthe Ramesh Seetharam Bhat
Data analysis: Marcio Covas Moschovas
Drafting of the manuscript: Kulthe Ramesh Seetharam Bhat, Young Hwii Ko
Critical revision of the manuscript: Vipul R.Patel
Conflicts of interest
The authors declare no conflict of interest.
杂志排行
Asian Journal of Urology的其它文章
- Nerve-sparing robot-assisted radical prostatectomy: Current perspectives
- Robtic-assisted radical cystectomy:Literature review
- Robot-assisted endoscopic inguinal lymphadenectomy: A review of current outcomes
- Robot-assisted retroperitoneal lymphadenectomy: The state of art
- Robotic surgery techniques to approach benign prostatic hyperplasia disease: A comprehensive literature review and the state of art
- Robotic renal and adrenal oncologic surgery:A contemporary review
