Nerve-sparing robot-assisted radical prostatectomy: Current perspectives
2021-03-26AnupKumarVipulPatelSridharPanaiyadiyanKultheRameshSeetharamBhatMarioCovasMoshovasBrusahanuNayak
Anup Kumar , Vipul R.Patel , Sridhar Panaiyadiyan ,Kulthe Ramesh Seetharam Bhat , Mario Covas Moshovas ,Brusahanu Nayak
a Department of Urology,Robotics and Renal Transplant, Vardhman Mahaveer Medical College and Safdarjang Hospital, New Delhi, India
b Department of Robotic Surgery, AdventHealth Global Robotics Institute, Celebration, FL, USA
c Department of Urology, All India Institute of Medical Sciences, New Delhi, India
Abstract Robotic-assisted radical prostatectomy(RARP)is the current standard of care with long term cure in organ-confined disease.The introduction of nerve-sparing (NS) to standard RARP has shown positive results in terms of functional outcomes in addition to the oncological outcomes.This article reviews the current perspectives of NS-RARP in terms of applied anatomy of the prostatic fascial planes,the neurovascular bundle(NVB),various NS techniques and postoperative functional outcomes.A non-systematic review was done using PubMed, Embase and Medline databases to retrieve and analyse articles in English, with following keywords“prostate cancer”, “robotic radical prostatectomy”, “nerve-sparing”.The Delphi method was used with an expert panel of robotic surgeons in urology to analyse the potency outcomes of various published comparative and non-comparative studies.The literature has shown that NS-RARP involves various techniques and approaches while there is a lack of randomized studies to suggest the superiority of one over the other.Variables such as preoperative risk assessments, baseline potency, surgical anatomy of individual patients and surgeons’ expertise play a major role in the outcomes.A tailored approach for each patient is required for applying the NS approach during RARP.
KEYWORDS Prostatectomy;Robot-assisted radical prostatectomy;Nerve-sparing
1.Introduction
Prostate cancer(PCa)is the second most common cancer and the sixth leading cause of cancer-related mortality in men.Owing to the routine prostate-specific antigen(PSA)screening,the highest rates of PCa are reported in Australia,New Zealand,North America, Western and Northern Europe [1].Robotassisted radical prostatectomy(RARP)forms a valuable therapeutic option for the management of localized PCa[2].
The outcomes of RARP have been reported in the form of trifecta results measuring the oncological outcome, continence,and potency[3].Although the oncological outcomes are the primary outcomes following RARP, with the acceptance of robotic-approach world-wide,improvement in the functional outcomes is widely reported.Taking into surgeons’ expertise and experience, decreased surgical complication and negative margins were also added to report the pentafecta outcomes [4,5].
First conceptualized by Walsh and Donker [6] in 1982,the anatomy and concepts of the nerve-sparing(NS)radical prostatectomy(RP)have ever been evolving.Moreover,the various mechanisms of injury to neurovascular bundle(NVB)lying in proximity to the prostate have further compounded the concept of NS in RP.This article aims to discuss the current concepts in neurovascular anatomy, various techniques of NS and functional results of NS RP in the current era of minimally invasive surgery.
2.Materials and methods
We performed a search of PubMed,Embase,Google Scholar and Medline databases for English literature to identify all the relevant studies using the following MeSH keywords:“prostate cancer”, “robotic radical prostatectomy” and“nerve-sparing robot-assisted radical prostatectomy”.Three authors (AK, SP and BN) independently reviewed the abstracts and articles including systematic review and meta-analyses.The Delphi method was applied with a panel of robotic surgeons to analyse the oncological and functional outcomes of various published studies and included in this review.Case reports,letters,editorials and articles in non-English language were excluded.
3.Neuroanatomy of prostate
The prostatic plexus of nerves along with vessels constitutes the NVB of Walsh.The NVB contained in the triangular space formed by the fascial planes, prostatic fascia in the medial,lateral pelvic fascia in the lateral and Denonvillier’s fascia in the posterior aspect.The triangular space is wide near the base and becomes narrow at the apex of the prostate.The cavernosal nerves responsible for the potency arise from the caudal portion of pelvic plexus, lying close to the tips of seminal vesicles and travel towards the posterolateral base of the prostate.From here, it runs towards the apex and membranous urethra enclosed within the fascial planes [7].
Based on this neurovascular anatomy, Walsh and Donker[6]described the first NS radical prostatectomy.Later various NS dissections were proposed.The plane of dissection betweentheprostatecapsule andtheprostaticfasciaisdenoted as intrafascial plane,whereas the plane between the lateral pelvic fascia and the prostatic fascia is denoted as the interfascial plane.The extrafascial plane of dissection is external to the Denonvillier’s fascia and the lateral pelvic fascia.Hence, a maximal NVB preservation is possible with either intrafascial or interfascial dissection[8,9].
In application to RARP, Tewari et al.[10] proposed the concept of the tri-zonal neural architecture of NVB based on cadaver experiments.The proximal zone is located 5-10 mm lateral to the seminal vesicles and contains the proximal neurovascular plate (PNP) covering the proximal part of the prostate and related to the bladder neck and seminal vesicles.The mid-zone is located in the posterolateral groove of the prostate and contains the predominant neurovascular bundles (PNB).In nearly half of the men, the bundle is well-formed while in others they found to be spread widely in the periprostatic space.Their identification is difficult sometimes as they are in close relation to the prostate pedicles and fascia.Also, they are at risk of injury in periprostatic inflammation and extracapsular extension.The distal zone contains the accessory and peri-apical nerves.The retro-apical nerves are particularly at risk of injury during the urethral transaction and vesicourethral anastomosis.This study also showed that the location of the accessory nerves may be variable.They may lie in the periprostatic fascia or between the prostate and the lateral fascia or the Denovillier’s fascia.
After oncological outcomes, functional outcomes after radical prostatectomy continued to evolve with refinement in the surgical techniques.One such modification is the NS hypothesized to improve the functional outcomes.With the evolution of robotics, nerve preservation techniques have been revolutionized.In this context, we describe the current status of various technical modifications of NS and its functional outcomes following NS-RARP.
4.NS surgical techniques during RARP
Numerous NS surgical techniques and approaches in RARP have been proposed concerning the periprostatic fascial anatomy [8,9,11-13].The NS technique in RARP is critical for the functional components of the trifecta and/or the pentafecta outcomes.Though there is little risk of positive margins after NS-RARP during the period of the learning curve, the results are mixed afterwards [8,9,14-16].To avoid positive margins, the surgeon has to be particularly careful during the posterolateral dissection at the base close to the prostate and the tumour.
4.1.Classification of NS techniques
Based on fascial dissections, the NS techniques can be intrafascial or interfascial:
4.1.1.Intrafascial
The working plane in the intrafascial dissection is remaining internally to the prostatic fascia at the anterolateral and posterolateral aspect of the prostate and anterior to the Denonvilliers’fascia.While allowing total preservationof NVB,the intrafascial dissection carries the greatest risk of iatrogenic capsular damage and positive surgical margin(PSM).
In the antegrade approach, the surgeon may develop an easier plane from the 6 o’clock position since the Denonvilliers’ fascia exists as a single thick layer at this level.However, during a high lateral approach, developing this plane could be more difficult due to the multilayered fasciae at the posterolateral side of the prostate [17].
4.1.2.Interfascial
In the interfascial dissection,the working plane is between the leaves of the prostatic fasciae at the anterolateral and posterolateral sides of the prostate and medial to the NVB.In contrast to the intrafascial dissection, the lateral prostatic fascia is left behind on the prostate specimen rather than on the NVB which allows greater safety margin decreasing the PSM [17].However, in the interfascial dissection, the estimation of NS extent is subjective.
Based on the surgical approach,the NS technique can be antegrade or retrograde:
4.1.2.1.The antegrade approach.In the antegrade approach, the direction of the dissection is from the prostatic base to the apex.A gentle upward traction of the vas and seminal vesicles reveals the posterior prostatic pedicle while avoiding undue traction on the NVB.The pedicles are clipped and divided close to the prostate.Avoiding energy devices at this step is critical to prevent thermal injury to the NVB.Gentle counter traction at the prostate delineates the lateral pelvic fascia and exposes the triangular space between the lateral pelvic fascia, the Denonvilliers’ fascia and the prostatic fascia,following which either interfascial or the intrafascial dissection is performed.
4.1.2.2.The retrograde approach.The direction of dissection is from the prostatic apex to the base.After the posterior plane is developed distally up to the apex, the prostate is slightly pushed to the left.The lateral pelvic fascia is incised sharply and the dissection is carried posteriorly to expose the NVB at the mid prostate level.Further dissection to the posterior plane releases the NVB from the prostate pedicle.The prostatic pedicles are controlled with Hem-o-lok clips at the base in a similar manner and the dissection is carried on to the apex to release the full NVB from the prostate.The NVB is released completely till the apex to avoid any positive margin during the apical dissection.
In a non-randomized prospective study, Ko et al.[18]reported a significant early return of the potency in the retrograde approach as compared to the antegrade approach in NS-RARP.The retrograde approach has the advantage of early identification and release of the NVB from the prostate before the posterior pedicle control,thus preventing any misplacement of the hemostatic clip.
As the cavernosal nerves have unmyelinated axons,they are prone to thermal damage.Ahlering et al.[16]proposed a cautery-free, clip-free NS-RARP using a combination of temporary occlusion of the posterior prostatic pedicles with bulldog clamps followed by application of FloSeal.
4.2.Different NS techniques
·Veil of Aphrodite technique (high anterior release)
·Super Veil technique
·Early retrograde release
·Hypothermic NS robot-assisted laparoscopic prostatectomy (hRLP)
·Modified clipless antegrade NS-RARP
·Flexible carbon dioxide(CO)laser fibre guided NS-RARP
·Potassium titanyl phosphate Laser NS RP
·Laparoscopic doppler ultrasound(LDU)probe in NS-RARP
·Transrectal ultrasound (TRUS) guided, energy free, NS laparoscopic RP
4.3.Veil of Aphrodite technique
Kaul et al.[19]reported a NS approach known as the Veil of Aphrodite technique.The initial plane of dissection is between the prostate fascia and lateral pelvic fascia from the base of the seminal vesicles using Harmonic shears.Following this, the interfascial dissection then proceeds in a “cold” manner between 1 and 5 o’clock and 6 to 11 o’clock in the right and left side,respectively.At the end of the dissection,the periprostatic tissue with NVB hung like a curtain from the pubourethral ligaments and hence the name, the veil of Aphrodite.
Menon et al.[14]showed the potency outcomes on 1 142 patients who underwent NS-RARP with this technique.At 1 year follow-up, 70% of men achieved the potency with or without phosphodiesterase 5 (PDE 5) inhibitors in patients who had preoperative sexual health inventory for men(SHIM) >21 and had a bilateral NS procedure [14].
4.4.Super Veil technique
The recognition that 25%of NVB can be found on the anterior surface, led Menon et al.[20] to modify the original Veil of Aphrodite technique.The modified technique includes an extension of the interfascial dissection more anteriorly.However,this step is challenging as the anterior surface has more fibromuscular component making the dissection difficult.
Ghani et al.[21]evaluated the postoperative potency in 85 patients undergoing super Veil NS-RARP.At a median follow-up of 18 months, 94% men on PDE 5 inhibitors had erections sufficient for vaginal penetration.In patients with a preoperative SHIM >17, 42% had SHIM scores between 18 and 25, 19% had SHIM 12-17, 14% had SHIM 8-11, and 25%had SHIM <7 at 18 months of follow-up [21].
4.5.Retrograde NS-RARP(early retrograde release)
Patel et al.[22]first described the early retrograde release of the NVB technique in an athermal manner.The key step in finding the correct plane is the identification of the“landmark prostatic artery”(LA).The assistant slightly rotates the prostate by grasping the lateral edge of the prostate at the base.With the help of the fourth arm,the bladder is retracted superiorly to align the prostate pedicle with the NVB and expose the lateral pelvic fascia.After incision on the lateral pelvic fascia,a distinctive tortuous LA can be found on the anterolateral aspect between the mid prostate and the base(Fig.1).A plane of dissection is then made between the LA and the prostate which is continued posteriorly.Then the plane is continued retrograde towards the base clipping the prostatic pedicles and distally towards the apex.This results in the detachment of the NVB including the more anteriorly distributed nerves(Fig.2).

Figure 1 Landmark artery on anterolateral aspect of prostate.
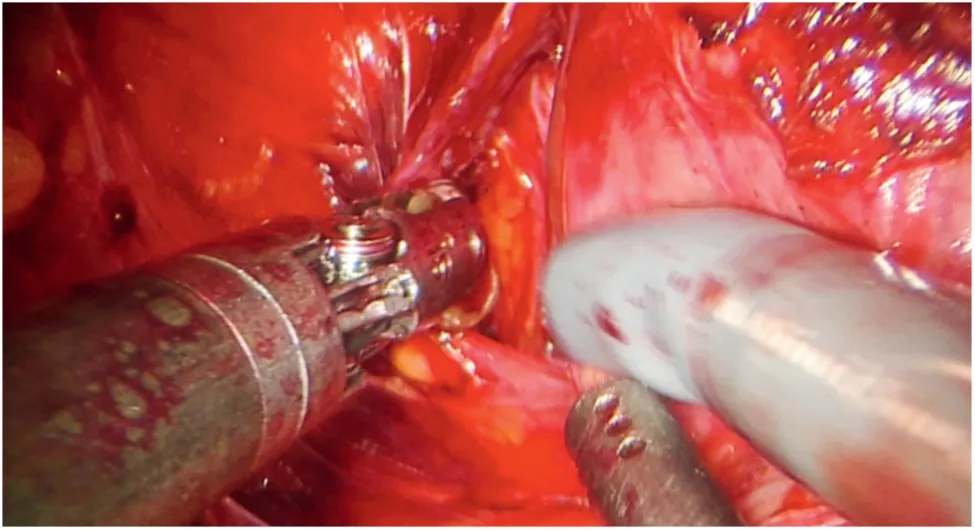
Figure 2 Left retrograde dissection towards the base of the prostate to completely detach the NVB from the prostatic pedicle.NVB, neurovascular bundle.
4.6.hRLP
Finley et al.[23]first reported the feasibility and the effect on early continence following pre-emptive local hypothermia during RARP.The hypothesis is that bladder and sphincter inflammation secondary to dissection of the prostate and the bladder can cause transient incontinence.They proposed that pre-emptive local hypothermia to the pelvis decreases the metabolic rate and attenuates the inflammation.The local hypothermia was achieved by an endorectal cooling balloon system (ECB) extending in the region of the prostate from the membranous urethra to the SV.A 24 Fr three-way Latex urethral catheter was placed inside the ECB,and the whole system was inserted into the rectum by inflating the latex balloon to 20 mL.By cold irrigation, pelvic cooling was then achieved with an ECB cycle of 40C.The 47 men,who underwent hRLP,had the 3 months 0-pad rate of 86.8% versus 68.6% in the controls.The return to continence was faster for hRLP than the controls (median: 39 vs.59 days) [23].
4.7.Modified clipless antegrade NS-RARP
Chien et al.[24]reported a technique of clipless antegrade NS which avoids the use of electrocautery.The authors first developed the posterior plane up to the apex in the midline of the prostate.Then by proceeding in a medial to the lateral direction, the pedicles and NVB are released on both sides.Neither clip nor monopolar electrocautery was used,however,the authors mentioned using bipolar device occasionally.Using as validated 36 item health survey questionnaire,they reported potency rates of 47%,54%,66%and 69%at 1,3,6 and 12 months respectively with or without PDE 5 inhibitors[24].
Anatomic grading of the proportion of NS was categorised by the Schatloff et al.[25,26] as given in Table 1.
4.8.Flexible carbon dioxide (CO2) laser fibre guided NS-RARP
The wide application of laser in endourology made Cheetham et al.[27] evaluate the feasibility of COlaser in NS-RARP.The property of minimal thermal spread with a maximal increase in the temperature of only 40C within 0.5 mm of the target area allowed researchers to explore its application during RARP.Ten patients underwent bilateral NS-RARP using OmniGuide®BeamPathTM URO-LG COlaser fibre.The laser fibre was inserted through the assistant port and manipulated by the robotic instruments.After the prostate pedicles are controlled, the laser fibre was used to develop the plane between the prostate and NVB.The authors showed that the laser system demonstrated a meticulous dissection of NVB and ease of fascial layer identification.One caveat was difficult to achieve effective coagulation in a large vessel.At 3 months follow-up 90%achieved continence[27].
5.Recent innovations in NS-RARP
5.1.Role of indocyanine green (ICG)
Kumar et al.[28] were the first to propose the application of near-infrared fluorescence (NIRF) and ICG in the identification of “landmark prostate artery” during RARP.The intravenously injected fluorescent molecule ICG is carried by the albumin.The ICG emits green fluorescence under infrared laser which is picked up by the endoscope signal detector and relayed to the surgeon console.This enables the console operator to appreciate the course of the prostate artery as a green fluorescent vessel over the lateral surface of the prostate (Fig.3).
On identifying the LA and the anatomy of NVB, an NS procedure was completed as described earlier.The authors reported identifying the landmark artery in 85% cases in a series of 10 men undergoing the RARP and concluded that identification of LA and its pathway helps both experienced and novice surgeons in NVB preservation [28].
5.2.Measures to check PSM during NS-RARP
5.2.1.Neurovascular structure adjacent frozen section examination (NeuroSAFE) in NS-RARP
The role of NeuroSAFE in NS RP was proposed by Schlomm et al.[29].After removal of the prostate specimen, the complete neurovascular structure adjacent to the prostate tissue is dissected.The specimen sent to the pathology department is cut into slices of 3-4 mm thick, resulting in 10-25 tissue blocks per patient.During this time,the surgeon completes bladder reconstruction, placement of anastomotic sutures, lymph node dissection and achieves adequate hemostasis.The whole process takes 35 min.A PSM is reported if at least one invasive malignant gland has reached the level of the inked surgical margin.If positive,an ipsilateral secondary neurovascular resection (SNR),including the rectolateral part of denonvilliers fascia(DF),is performed,before the completion of the anastomosis.

Table 1 Anatomic grading of the proportion of nerve-sparing.
In 5 392 men, the authors showed that the frequency of NS with NeuroSAFE procedure was significantly higher in all the pathological T stages as compared to the matched non-NeuroSAFE RPs.Also, the rate of PSMs was significantly lower in the NeuroSAFE group for all stages [29].
5.2.2.Ex vivo fluorescence confocal microscopy (FCM)
By extrapolating the promising role in the diagnosis of cutaneous malignancies, few researchers explored the feasibility of ex vivo FCM in the diagnostic discrimination of the prostatic adenocarcinoma from the surrounding noncancerous part compared to the standard histopathological examination.In their preliminary study, Puliatti et al.[30] showed a substantial level of agreement (k-value=0.75) between FCM and histopathological examination with an area under curve (AUC) of 0.884, an 83.3% sensitivity, 93.5% specificity and 91.0% accuracy compared to conventional histopathological evaluation [30].
Recently,Bertoni et al.[31]created an atlas and also evaluated the learning curve of FCM images interpretation of 80 fresh biopsy specimen obtained from the RP specimen evaluated by two pathologists using the FCM VivaScope®2500 M-G4(Mavig GmbH, Munich, Germany; Caliber I.D, Rochester,NY,USA).With the corresponding Hematoxylin and Eosin images, the authors created an atlas of FCM images into nonneoplastic tissue, high-grade prostatic intraepithelial neoplasia and prostatic acinar adenocarcinoma.The specimens were re-examined after 90 days by the two pathologists.They demonstrated a short learning curve.Also,the agreement between the FCM reading and the histopathological diagnosis increasedfrom86%to92%inthefirstreadingforthefirstandthe second pathologists, respectively, to reach 95% for both pathologists in the second reading[31].

Figure 3 dHAM placed over as right sided nerve wrap on NVB.dHACM, dehydrated human amnion/chorion membrane; NVB,neurovascular bundles.
5.3.Role of multiparametric magnetic resonance imaging (mpMRI) before NS-RARP
The mpMRI being a diagnostic tool in the PCa detection,also proved to be an optimal tool for local staging with an accuracy in the prediction of extracapsular extension(ECE)up to 80%.Schiavina et al.[32]evaluated the role of mpMRI to guide NS during RARP.On comparing 137 men with preoperative MRI with 166 men without MRI,the authors showed that the mpMRI revision altered theNS plan in 46.7%case onpatient-based and 56.2%on side-based analysis.The surgical plan change resulted equally between more radial and less radical approach both on patient-based side-based.Furthermore, men with preoperative mpMRI had significantly lower overall PSM as compared to the control group(12.4%vs.24.1%;p≤0.01)[32].In contrast, the results of the systematic review and meta-analysis showed that the preoperative MRI altered the initial surgical plane in only one-third cases, but increased with the increasing PCa risk category.Also,modification based on MRI did not affect the PSM rate[33].
5.4.Use of biological membranes during NS-RARP
Reduced ischemic nerve injury with diminished traction during RARP was shown by Tewari et al.[34].Apart from minimising the traction injury,researchers also explored various strategies to improve nerve regeneration.Many neurotrophic factors influence different phases of Wallerian degeneration and axonal regeneration.Conjugated neurotrophic factors(nerve growth factor, glial cell line-derived neurotrophic factor, and brain-derived neurotrophic factor) and drugs inhibiting phosphodiesterase to increase cGMP were found to induce neurogenesis,angiogenesis and synaptogenesis.More recently biological membranes with neurotrophic factors were proposed to alter the neuropraxia[35].
In a propensity-matched analysis,Patel et al.[36]evaluated the role of dehydrated human amnion/chorion membrane (dHACM) (AmnioFix) wrap around the NVB in 58 men compared with matched 58 men without the wrap.The wrap was placed bilaterally around fully preserved NVB after the completion of urethra-vesical anastomosis(Fig.4).Although the continence and potency rates at 8 weeks were not statistically significant, the dHACM placement significantly resulted in early return to continence(1.21 months vs.1.83 months,p=0.03)and potency(1.34 months vs.3.39 months,p=0.007).Also, the mean SHIM scores were higher in men with dHACM wrap(mean score 16.2 vs.9.1).
In a similar article by Ogaya-Pinies et al.[37], men with bilateral dHACM wrap around the NVB(n=235)after NS-RARP had significant early return to potency (2.37 months vs.3.94 months,p=0.0001)as compared to the control group(n=705).The potency rates were higher in the dHACM group at all intervals(1,3,6 and 9 months)except at 12 months follow-up.
Chitosan, a polysaccharide derived from chitin obtained from shellfish exoskeleton was found to have neurotrophic factors.Porpiglia et al.[38]evaluated the 1 year efficacy of the application of chitosan membrane(ChiMe)on NVB after NS-RARP.They have shown significant improvements in the potency rate at 1 month(36.76%vs.25.88%;p=0.02)and 2 months (52.2% vs.39.22%; p=0.01) in men with ChiMe application as compared to the control group.Beyond 2 months, though not statistically significant, the potency rates were higher in the intervention group.
5.5.Augmented reality (AR) RARP (AR-RAPP)
As an extension of robotics, three-dimensional (3D) reconstruction of the high resolution MRI prostate was integrated into the robotic console to perform“image guided surgery”called AR-RARP.In a preliminary study, Porpiglia et al.[39]showed the feasibility and the accuracy of AR-RARP.Men with cT2 PCa(n=16)underwentintrafascialdissectionforNS with a mark on the corresponding capsule with underlying intraprostatic lesion for virtual identification.In case of cT3 PCa(n=14), standard NS-RARP was performed along with ARguided biopsy of the suspected ECE region.With AR-RARP the authors reported 30% PSM.The final histopathology confirmed the underlying intraprostatic lesion in all cases of cT2 and in more than 3/4 cases in cT3 who underwent AR guided biopsyofsuspectedECE.When theprostatespecimens were scanned to assess the concordance, the mismatch between the 3D reconstruction and prostate scanning was only 1-5 mm[39].
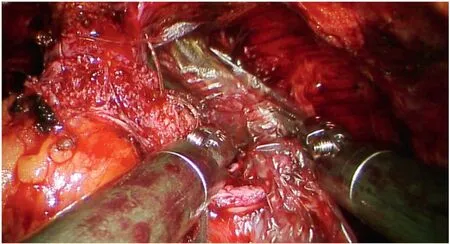
Figure 4 Landmark artery seen as green fluorescent structure over lateral surface of prostate in near infrared fluorescence mode.
To evaluate the true help of the AR-RARP in the image guided surgery,six expert robotic surgeons were made to use the technique during live surgery sessions in an academic meeting.A questionnaire was administered at the end of the surgeries to collect the insight of the expert surgeons especially during the four key steps of RARP namely bladder neck dissection, NS technique, apical dissection and tailoring of selective biopsies of prostate lodge after prostatectomy.In an ordinal ten-point likert scale(where 1=strong negative opinion and 10=strong positive opinion),the median score from the evaluation of each of the aforementioned steps of AR-RARP was 9(interquartile range[IQR]9-10)suggesting an increased interest for image-guided surgery[40].
Later, the updated data on assessing the use of hyperaccuracy 3D (HA3D) reconstruction and superimposed image during AR-RARP were published by the same group.Eleven and 19 men had PCa with and without suspicion of ECE on high resolution mpMRI, respectively.The final histopathology confirmed the underlying index lesion in all cases.The AR-guided selective biopsies at the level of NVBs confirmed the ECE location in 73% cases.The discordant between the 3D reconstruction and the 3D scanning of the whole mount specimen was <3 mm in 85%of the cases[41].
6.Unilateral versus bilateral NS-RARP: Does it matter?
The literature is scarce in addressing this issue.The only available study by Finley et al.[42] showed no significant difference with unilateral or bilateral NS in RARP.However,this study is limited with a lower number of patients in the unilateral group as compared to the bilateral group.Also,the comparison was between the application of with or without electrocautery precluding a firm conclusion to be drawn.In contrast,Greco et al.[43]reported men with bilateral NS had significantly higher rates of potency than the unilateral group on patients undergoing intrafascial NS laparoscopic RP(LRP).
In a population-based, prospective observational (the CEASAR) study, Avulova et al.[44] showed a better sexual and urinary function outcomes with bilateral NS than unilateral or non-nerve sparing.However, in men with low baseline sexual function, the difference was not significant.The study is limited with a lower number of men undergoing unilateral NS approach and also combining unilateral NS and non-nerve sparing as one group to compare with bilateral NS.
Although a maximum NS theoretically improves the functional outcomes following RARP, at the time of this writing, there is a lack of clear consensus regarding unilateral versus bilateral NS techniques and further prospective studies are needed.
7.The potency outcomes after RARP:Contemporary outcomes and evidence
The potency rates following RARP varied between 54.0%and 97.4% [2,8,9,14,18,45-48].The studies were confounded in the patient selection, preoperative potency evaluation,intraoperative techniques and approaches for NS, surgical experience and postoperative follow-up protocols.Table 2 highlights the major non-comparative RARP series reporting potency outcomes across the world.
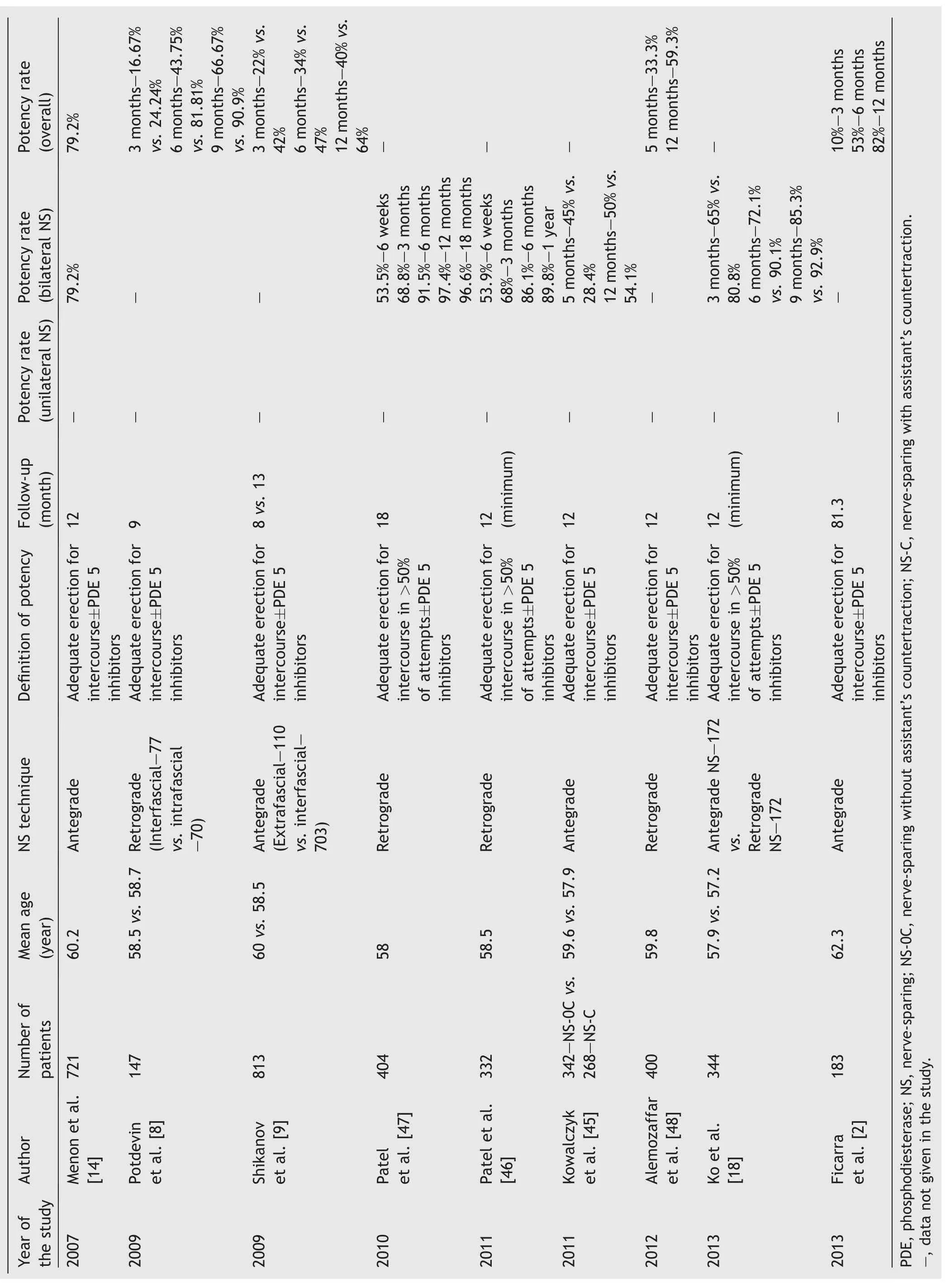
Table 2 Various non comparative studies reporting potency outcomes in patients undergoing robot-assisted radical prostatectomy.
Various studies have compared outcomes of RARP to open and/or LRP.Studies comparing RARP and open radical retropubic prostatectomy (ORP) showed mixed results.Most of them showed significant advantages of potency recovery in RARP while others did not find any differences in either functional or oncological outcomes [49-51].However,in a recent study,Haese et al.[52]compared the oncological,functional and surgical outcomes of OPR versus RARP in >10 000 men.The oncological outcomes and 12 months potency rate were comparable between the groups.The continence rates were significantly higher in RARP at 1 week(25.8%vs.21.8%,p<0.001)and 12 months(90.3%vs.88.8%,p=0.01).However,this difference was not obtained after age stratification.Although operation time was shorter in ORP, blood loss, transfusion rates and time to catheter removal were significantly lower in RARP.
On comparing RARP and the LRP, RARP was reported to have significant higher potency rates than the LRP or comparable results[53-55].Table 3 and Table 4 summarize the various studies comparing the outcomes of RARP with the open and laparoscopic approach of RP.Although the heterogeneity of these studies makes the interpretation difficult,the potency in NS-RARP series is determined to be higher in the short term as well as in the long-term results.
8.Trifecta and pentafecta outcomes following NS-RARP
The combined oncological and functional outcomes following RARP were traditionally reported as “Trifecta”.Later, the addition of negative surgical margins and early post-surgical complications to the trifecta is denoted as“pentafecta” outcomes to reflect the surgeons’ experience.Comparing the trifecta and pentafecta outcomes is challenging due to the heterogeneity of the published reports in terms of preoperative patient selection, postoperative time of assessment, the tool used to assess potency and definition of BCR.Particularly literature on trifecta and pentafecta outcomes following NS-RARP was limited.
Asimakopoulos et al.[55] compared RARP with LRP in terms of pentafecta after bilateral NS approach.There are 62 (45.6%) patients in 136 men, who achieved pentafecta following RARP as compared to 25 (27.5%) patients in 91 men,achieving pentafecta following LRP.Young age,lower pathological stage and undergoing robotic approach were significantly associated with pentafecta.Ou et al.[56] in a prospective study of 230 men undergoing bilateral NS-RARP showed achieving a trifecta and pentafecta rate of 81.7%and 60.4%, respectively.Pentafecta outcomes offer better functional and oncological outcomes than trifecta, however, future studies should follow uniformity in reporting the outcomes for better comparison.
In a retrospective study of 566 men with NS-RARP,Jazayeri el al.[57] showed the pentafecta and trifecta to be 73.9% and 64.1%, respectively.Men achieving pentafecta were significantly younger with fewer comorbidities,lower PSA, lower Gleason’s score and lower PCa risk category [57].
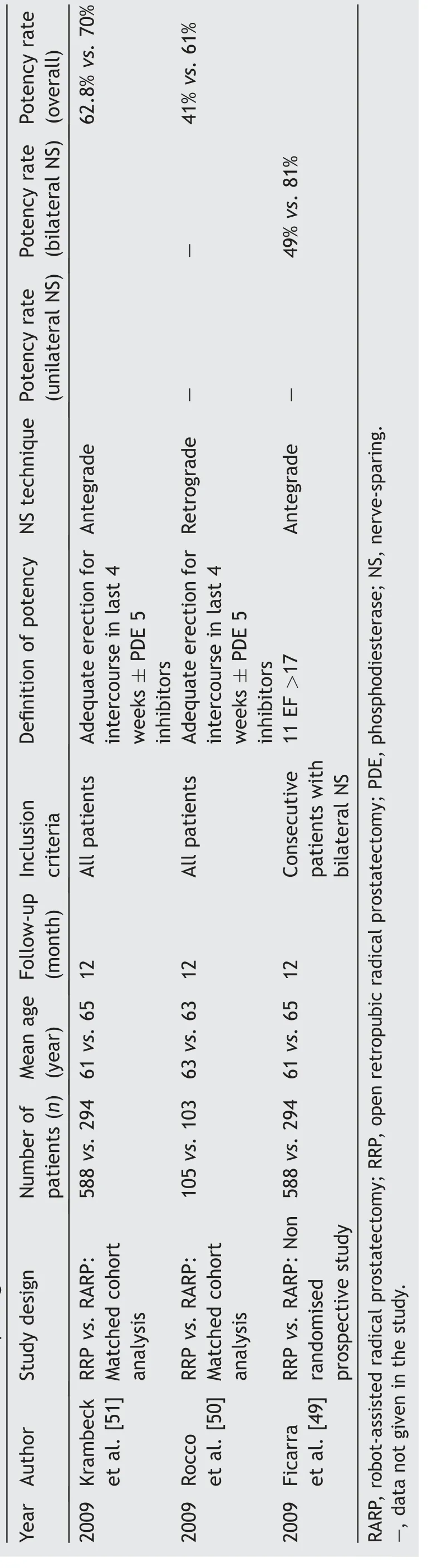
Table 3 Studies comparing outcomes between RARP vs.RRP.

Table 4 Studies comparing outcomes between robot-assisted RARP vs.LRP.
9.Conclusion
NS-RARP, although technically demanding, is a critical step in improving the functional outcomes following surgery.Athermal dissection, athermal control of the prostatic pedicle, minimal or negligible traction to the NVB and bilateral NS as much as possible aid in favourable functional outcomes.Despite the NS approach, the functional outcomes are affected by baseline preoperative potency, the tumour extent in the biopsy results and most importantly the surgical anatomy of the patient.NS-RARP involves different techniques and approaches, while there is a lack of randomized controlled trials to define which technique and/or approach is superior.As the patient’s anatomic factors may affect these techniques and approaches, the surgeon’s experience is utmost important to decide the right surgical technique.Finally, the appropriate patient selection, a wise intraoperative clinical judgment and tailored approach for each patient are required to decide for NS during RARP.
Author contributions
Study concept and design: Anup Kumar, Vipul R.Patel,Sridhar Panaiyadiyan, Kulthe Ramesh Seetharam Bhat,Marcio Covas Moschovas, Brusabhanu Nayak.
Data acquisition: Anup Kumar, Vipul R.Patel, Sridhar Panaiyadiyan, Kulthe Ramesh Seetharam Bhat, Marcio Covas Moschovas, Brusabhanu Nayak.
Data analysis: Anup Kumar, Vipul R.Patel, Sridhar Panaiyadiyan, Kulthe Ramesh Seetharam Bhat, Marcio Covas Moschovas, Brusabhanu Nayak.
Drafting of manuscript:Anup Kumar,Vipul R.Patel,Sridhar Panaiyadiyan, Kulthe Ramesh Seetharam Bhat, Marcio Covas Moschovas, Brusabhanu Nayak.
Critical revision of the manuscript: Anup Kumar, Vipul R.Patel, Kulthe Ramesh Seetharam Bhat, Marcio Covas Moschovas, Sridhar Panaiyadiyan, Brusabhanu Nayak.
Conflicts of interest
The authors declare no conflict of interest.
杂志排行
Asian Journal of Urology的其它文章
- Robtic-assisted radical cystectomy:Literature review
- Robot-assisted endoscopic inguinal lymphadenectomy: A review of current outcomes
- Robot-assisted retroperitoneal lymphadenectomy: The state of art
- Robotic surgery techniques to approach benign prostatic hyperplasia disease: A comprehensive literature review and the state of art
- Robotic renal and adrenal oncologic surgery:A contemporary review
- Comparison of the oncological,perioperative and functional outcomes of partial nephrectomy versus radical nephrectomy for clinical T1b renal cell carcinoma: A systematic review and metaanalysis of retrospective studies
