Robot-assisted endoscopic inguinal lymphadenectomy: A review of current outcomes
2021-03-26GilertoJoseRodriguesGiulinoBetoniGuglielmettiMreloOrvietoKultheRmeshSeethrmBhtVipulPtelRfelFerreirCoelho
Gilerto Jose´ Rodrigues , Giulino Betoni Guglielmetti ,Mrelo Orvieto , Kulthe Rmesh Seethrm Bht ,Vipul R.Ptel , Rfel Ferreir Coelho ,
a Sao Paulo State Cancer Institute, University of Sao Paulo School of Medicine, Sao Paulo, Brazil
b Clı´nica Alemana, Santiago, Chile
c Department of Urology, AdventHealth Global Robotics Institute, Celebration, FL, United States
Abstract Objective: To review the role of robot-assisted endoscopic inguinal lymphadenectomy (RAIL) in the management of penile cancer.Methods: A PubMed search for all relevant publications regarding RAIL series up until August 2019 was performed using the keyword “robotic”, “inguinal lymph node dissection”, and“penile cancer”.Weighted mean was calculated in the largest series for all outcomes using the number of patients included in each study as the weighting factor.Results: We identified 23 articles,of note the three largest series that included 102,27,and 20 RAIL in 51,14,and 10 patients,respectively.Saphenous vein was spared in 88.93%of RAIL cases in these series and node yield was 11.42 per groin;35.28%of patients had positive pathological nodes.The weighted mean of operative time was 87.98 min per RAIL and the estimated blood loss was 37.08 mL per patient.The mean length of hospital stay was 1.29 days and the drain was kept in place for 17.02 days; the major complication rate was only 5.31% in these series.The mean follow-up was 33.46 months with a recurrence-free survival of 96.33%.Conclusion: The literature regarding RAIL describes promising results, although it has shorter follow-up and higher costs when compared to historically series from the open approach.Initials series reported lower cutaneous complications compared to conventional approach,without compromising oncological outcomes.However, long-term results and larger trials are crucial to validate those findings.
KEYWORDS Penile tumor;Minimally invasive surgery;Robotic-assisted inguinal lymphadenectomy
1.Introduction
Invasive penile squamous cell carcinoma (PSCC) has an incidence smaller than 1% of all malignant neoplasms in men from the United States and Europe.However, in developing nations of Asia, Africa, and South America, it reaches up to 10% [1].Besides the penectomy, assessment of the inguinal lymph nodes is of utmost importance,because nodal metastasis follows a predictable spreading pattern.Initially, it starts from the penis to the inguinal sentinel node, then to other superficial and deep inguinal nodes, the node of Cloquet, and finally to pelvic nodes,where the odds to progress with distant metastasis rise substantially [2-4].
Current guidelines recommend to perform bilateral modified inguinal lymphadenectomy(ILND)in patients with no palpable inguinal nodes presenting with intermediate(T1b and G1-2) or any high-risk features (T1G3 or higher,>50% poor differentiated, lymphovascular invasion) and radical ILND in patients with palpable inguinal nodes (cN1/cN2) [5,6].
Catalona [7] was the first author, in 1988, to propose a modified template compared to the radical dissection by Daseler and associates [8].He found the innovative technique as being less morbid than the classical ILND [7].Despite that, perioperative complications such as wound infection,flap necrosis and lymphedema can affect as many as two-thirds of patients even with modified templates[9].Modifications such as thicker skin flaps and smaller fields dissection have successfully decreased these rates to almost a quarter of patients [10].Nevertheless, due to its morbidity, ILND is still reported as underperformed in the United States,and even when this procedure is performed,node yield is often unsatisfactory [11].
Other possibility trying to reduce morbidity for intermediate or high-risk disease is dynamic sentinel guided biopsy with reliability to properly identify rates in more than 90% when done combining techniques of radioisotope and patent blue by experienced centers [12-15].
As in the other fields in urology, minimally invasive approaches to ILND have been described in an attempt to reduce morbidity and optimize convalescence [16].The first endoscopic technique of ILND performed on two human cadavers was described by Bishoff and associates in 2003[17], and subsequently in a living patient.Then, the first successfully videoendoscopic radical inguinal lymphadenectomy (VEIL) report in the clinical urology scenario was performed by Machado et al.[18] in 2005.
In the following years, Machado et al.[3] compared the morbidity of open ILND (OILND) with VEIL.They described 50%more complications in the open procedure.Despite the longer operative time (OT) in the VEIL group, the mean number of retrieved and positive nodes was similar, while length of stay (LOS) and time to resumption of daily activities were shorter with VEIL.
Due to penile cancer rarity and the steep learning curve of pure laparoscopy, a robotic-assisted endoscopic inguinal lymphadenectomy (RAIL) was first described by Josephson and colleagues [19] in 2009, intending to surpass the limitations of lap surgery.The possibility to follow the surgical principles of OILND associated with the benefits of the robotic platform, including the increased magnification, 3-dimensional clarity, and dexterity optimization given by additional degrees of freedom, could decrease the morbidity while preserving the oncologic outcomes of ILND[19-23].
This article aims to review the outcomes of RAIL currently described in the literature.
2.Methods
We performed an electronic PubMed search for all relevant publications regarding outcomes and techniques of the RAIL up to August 2019, which resulted in a total of 23 papers.We used the keywords “robotic”, “inguinal lymph node dissection”, and “penile cancer”.One of them was regarding the role of robot-assisted inguinal lymph node dissection for vulvar carcinoma and it was excluded from this analysis.
Since PSCC is a rare disease and RAIL was first described only 10 years ago, we selected the three largest reports that included ten or more patients and calculated the weighted means for perioperative and oncologic outcomes.
3.Results
Since the first RAIL described in 2009 and the relative rarity of this disease, small reports have been published suggesting feasibility,acceptable OT,low estimated blood loss(EBL), short LOS, proper amount of lymph nodes retrieved and promising postoperative outcomes, especially regarding few rates of complications [21,22,24-28].Of note,two from this previously reports described also initial experience with the use of near-infrared fluorescence imaging (NIRF) using indocyanine green (ICG) to facilitate lymph node identification during robotic groin dissection for PSCC [26,28].
Hereafter, results from the three largest series are presented and their weighted means are evaluated.Patients’characteristics are described in Table 1.In total, 75 patients and 149 groin dissection were analyzed combining the three series.The clinical nodal staging was described as follows: Seventy-three point three two percent of patients without palpable nodes (cN0), 14.72% cN1, and 10.64% cN2(Table 1).
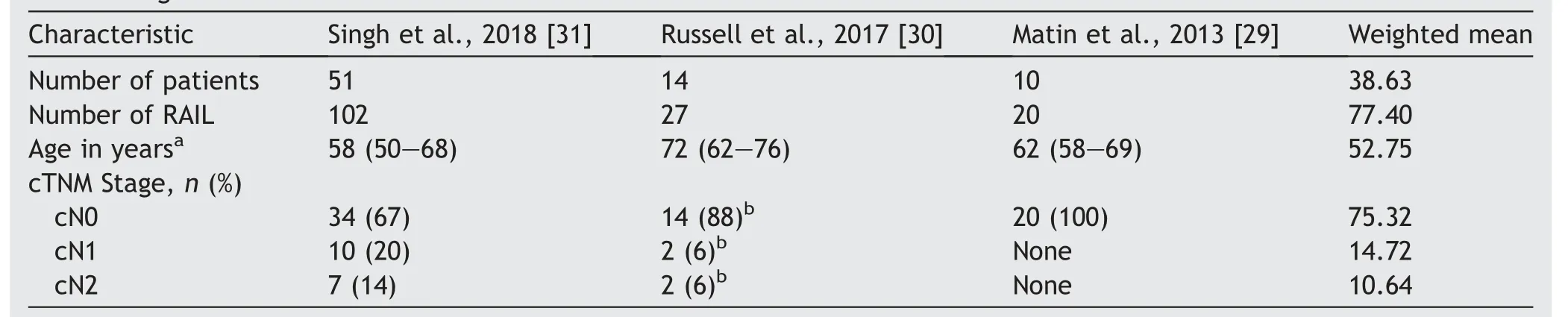
Table 1 Characteristics of patients from the three largest RAIL series, according to number of patients, procedures,age and clinical stage.
The weighted means of operative outcomes are described in Table 2.Of note,63.19%of patients underwent superficial ILND only.The saphenous vein was spared in 88.93%, node yield per groin was 11.42, and OT per limb was 87.98 min, with EBL of 37.08 mL, and LOS of 1.29 day.Drainage was kept in place for 17.02 days.
Table 3 describes the oncologic outcomes.Combining the data of these three series, the rate of positive pathological nodes (pN+) was 35.28%, and the recurrence-free survival rate was 96.34%, with a mean follow-up of 33.46 months.
Finally, complications are summarized in Table 4.The major complication rates(Clavien III and IV)in these series were 5.31%; only three flap necroses were recorded in a total of 149 procedures (1.34%).The lower rates of cutaneous complications seem to be the greatest advantage of RAIL compared to OILND, which has classically been correlated with flap necrosis rate as high as 15%-20% [5].

Table 2 Operative outcomes from the three largest RAIL series, according to node dissection, saphenous vein sparing and perioperative findings.
In 2013, Matin and colleagues [29] reported a prospective phase 1 study of 10 patients who underwent superficial RAIL with a median age of 62 years; all patients were cN0.The primary endpoint of this trial was to ensure the adequacy of RAIL by an independent open surgeon that verified the surgical field with an open incision after the RAIL procedure.The open surgeon confirmed that 18 of 19 inguinal areas (94.7% in nine patients) had an adequate dissection, all the positive nodes were properly retrieved by RAIL, and only two benign nodes could be found just beneath Scarpa’s fascia above the inguinal dissection field.As part of the study design, making an open incision to verify the surgical field limited the evaluation of complications.The median EBL was 100 mL (range from 10 mL to 200 mL), while the OT range per groin was from 90 min to 120 min (Table 2).There were no intraoperative complications.The median superficial and deep pN+ were 2 and 1, respectively(Table 3).Recurrence and follow-up were not recorded-One RAIL procedure needed conversion due to poor visualization after a wrong plane dissection (Table 4).Despite the study design limitation to access the complications, two patients required re-admission to the hospital within 60 days for wound infection treatment.One of them underwent incision and drainage of an abscess.Two other patients were treated as outpatients,one for wound breakdown (over the verification site) and the other for skin necrosis (overlying the dissected field).
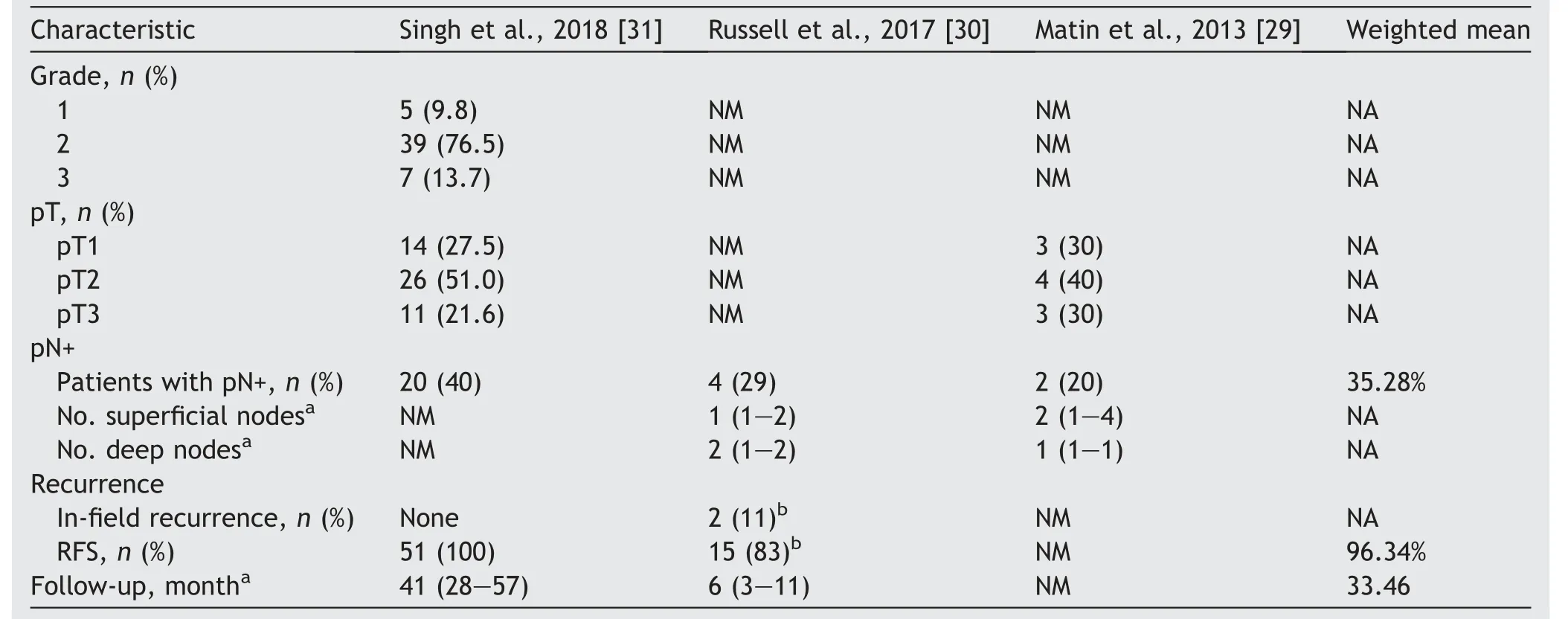
Table 3 Oncological outcomes from the three largest RAIL series,according to pathological grade,tumoral and nodal staging and recurrence status.
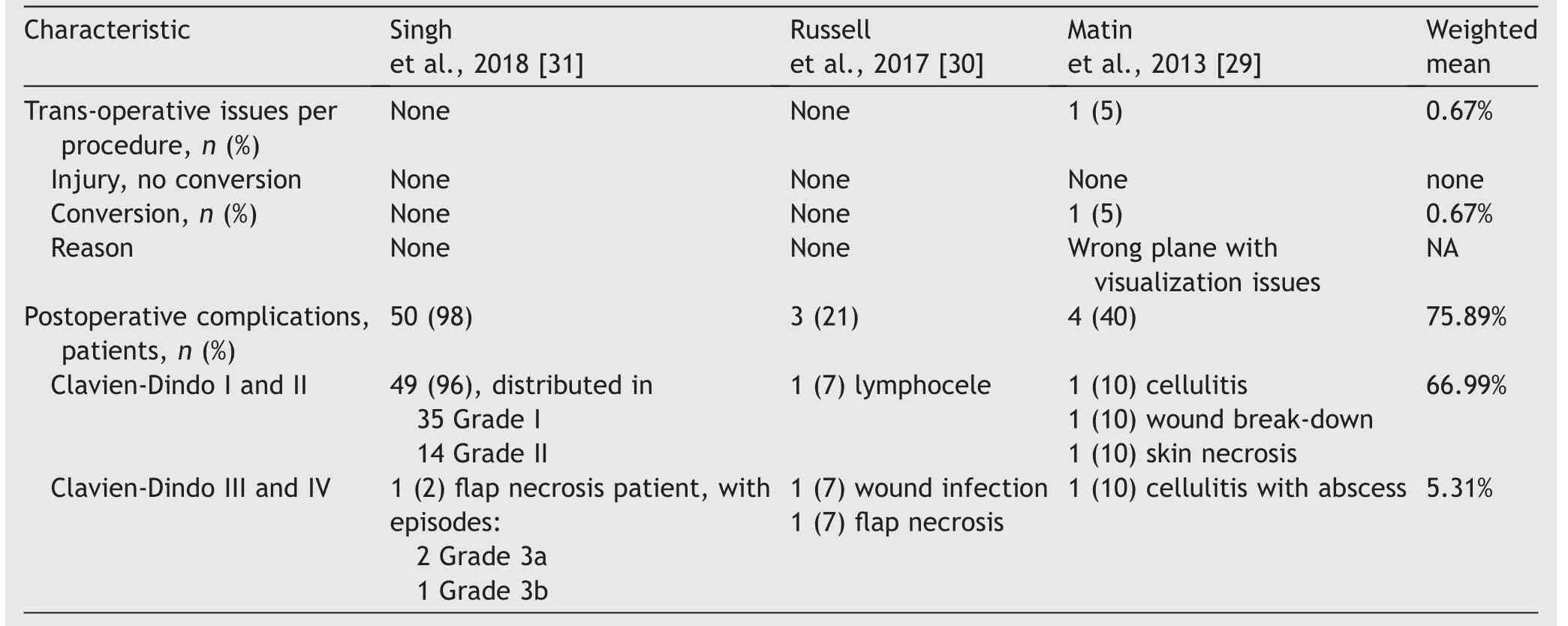
Table 4 Complications from the three largest RAIL series, according to trans-operative and postoperative period.
Then in 2017 Russell et al.[30] reported 14 patients submitted to RAIL and four patients submitted to VEIL.The patients were mainly cN0; however, there were two patients clinical N1(palpable mobile unilateral inguinal lymph node)and N2(palpable mobile multiple or bilateral inguinal lymph nodes), Table 1.They found similar results between the groups with higher ratios of saphenous vein sparing favoring RAIL with a significant difference.Additionally,there were lower reports in overall complications (11% vs.43%) supporting RAIL.From 27 RAIL procedures, 16 were only superficial,and 11 also included dissection of the deep lymph nodes(Table 2).The median nodal yield,OT,EBL and LOS were 8 nodes, 137 min, 50 mL and 1 day, respectively.The median time to drain removal was 36 days.The median pN+ of inguinal superficial and deep were 1 and 2,respectively (Table 3).In a median follow-up of 6 months,all three patients who developed recurrence had pN+ that occurred in a median time of 2 months.There were no conversions to open ILND (Table 4).Three patients developed complications, one minor (lymphocele) and two others that required intervention, such as wound infection and flap necrosis.
Finally, recently, Singh et al.[31] described the largest series up to date from India.They compared retrospectively 51 patients submitted to RAIL to 100 patients treated with OILND.The authors found a significant difference between the groups in terms of OT, LOS, days with drain,major complication, complication, edge necrosis, flap necrosis, and severe limb edema favoring RAIL.The median age of the robotic group was 58 years; 34 patients had no palpable inguinal nodes, ten patients were cN1, and seven were cN2 (Table 1).In the robotic arm, there were 62 procedures with only superficial ILDN and 40 that required both superficial and deep dissection; in this group, the saphenous vein sparing could be performed in 88 of the 102 procedures and the median lymph node yield per groin was 13 with an OT of 75 min.Finally,regarding the robotic arm,the median EBL and LOS were 75 mL and 3 days, respectively.They recorded a total of 20/51 (40%) patients from the RAIL group with pN+ (Table 3).After a median followup of 41 months, no recurrence was observed, with a recurrence-free survival of 100%.Moreover, none of the RAIL procedures needed conversion.Of the 51 patients in the RAIL, 40 (79%) had postoperative complications.However, most of them were Clavien Grade I or II, and only 1(2%) had a major complication.
4.Discussion
Penile cancer is an aggressive disease that can present fast progression and lead to death if not appropriately treated [32].The optimal surgical procedure to increase survival in this group of patients must be performed with free margins resection of the primary PSCC and ILND in those with high-risk features or patients with positive clinical nodes.The most important prognostic factors impacting survival in patients with invasive PSCC are the inguinal and pelvic lymph node status and the extent of metastasis.The number of pN+, the presence of extranodal extension, and the involvement of pelvic nodes are highly associated with the worst cancer-specific survival.That’s why it’s of utmost importance to manage this disease as soon as possible [4].
Efforts have been made for more than 30 years to reduce the significant ratios of morbidity of the OILND whereas almost 2/3 of patients present minor complications,such as superficial wound infections, wound dehiscence, mild edema, and seroma.The 1/3 remaining have major complications such as flap necrosis, deep vein thrombosis, and lymphocele requiring drainage [33,34].Modifications of OILND with smaller fields of dissections, saphenous vein sparing, and thicker skin flaps have been described, even though high rates of complications were maintained[7,35].Still, attempts of template modification also presented false-negative results with insufficient nodes retrieved,while the high incidence of false positive nodes could indicate unnecessary surgery [36].
In this background,dynamic senile biopsy improved over time and recently series reported false-negative rates around 5% with low complication rates lower than 10%without long term sequelae [37-40].
The introduction of minimally invasive approaches showing less postoperative pain, blood loss, and faster postoperative recovery in other pathologies appeared attractive and promising also in the ILND scenario[41-43].Initially, with VEIL and more recently with RAIL, better outcomes in terms of EBL, unintentionally trans-operative injuries, LOS, and postoperative complications have been recorded[19,44,45].In fact,it seems that one of the major advantages of RAIL series is the lower rates of skin necrosis,severe lymphedema,and wound infection requiring surgical intervention compared to OILND [31].
Even when comparing VEIL to RAIL, Russell et al.[30]showed that this evolution occurred due to surgeons’preferences over time.The advantages of three-dimensional magnification, and degrees of freedom with increased manual dexterity provided more precise dissection and allowed to accomplish all surgeries without conversion,beyond to preserve saphenous vein in all their patients.However, in the VEIL arm the saphenous vein could not be spared in 9%and there was one patient that presented a major bleeding requiring conversion.They also reported major rates of complications in patients that saphenous vein was not spared, which favors better outcomes with the RAIL technique.
As an inherent part of a rare pathology, the current literature has few reports since the introduction of RAIL.The eight case-report regarding this procedure could describe the feasibility of the first RAIL technique reported with minimal modifications when compared to the open surgery [19,26,30].They also assumed that the increased freedom of movements and better images provided by the robotic system could properly replicate the open technique, maintaining the oncologic principles [19].
According to the three most recent publications, the number of patients submitted to RAIL increased from 20 to up to 102 cases.Also, these series reported low rates of major complications and better outcomes when compared to OILND.Moreover, RAIL revealed to be an acceptable method in all the three series in terms of lymph node yield,where a median number of nodes retrieved were comparable to OILND reports [46,47].Initially, only patients with unpalpable nodes were included in the studies;however,in the latest two series, even patients with positive nodes underwent surgery with satisfactory outcomes.
Singh et al.[31] compared OILND to RAIL in a head-tohead study and described that the pathological nodal stage and the OILND were independent risk factors associated with an increased risk of major complications.Therefore, the authors reinforced the importance of not delaying the diagnosis and suggested the migration to minimally invasive treatment.
The two most considerable limitations of RAIL are the costs related to the robotic system and long-term follow-up to evaluate the oncologic outcomes.As reported by Chang et al.[48], costs are significantly higher in patients with melanoma who were submitted to ILDN and developed postoperative complications.However, until now, the literature lack studies to evaluate and compare costs in patients with PSCC submitted to ILND.Finally, as the technology continues to spread to developing countries,where the incidence of this disease is higher, the understanding regarding the long-term oncological outcomes of this minimally invasive procedure tends to increase[49,50].
5.Conclusion
Historically, the ILND technique underwent different attempts of modifications to reduce the morbidity related to the procedure.The minimally invasive approach, specially RAIL, is feasible at centers experienced in managing this disease and appears to be promising by decreasing the complication rates, especially the major cutaneous issues.Also, the replication of the open templates with similar lymph node yield retrieved was achieved in the recent series.It’s important to proper identify and select patients more likely to benefit from RAIL, mainly patients with less volume of disease.Still, long-term follow-up and further trials comparing the classical OILND and VEIL with RAIL are expected to ensure long-term oncologic outcomes.
Author contributions
Study concept and design:Gilberto Jose´Rodrigues,Giuliano Betoni Guglielmetti, Marcelo Orvieto, Rafael Ferreira Coelho.
Data acquisition: Gilberto Jose´ Rodrigues.
Data analysis: Gilberto Jose´ Rodrigues, Rafael Ferreira Coelho.
Drafting of manuscript: Gilberto Jose´ Rodrigues, Kulthe Ramesh Seetharam Bhat.
Critical revision of the manuscript: Giuliano Betoni Guglielmetti, Marcelo Orvieto, Kulthe Ramesh Seetharam Bhat, Vipul R.Patel, Rafael Ferreira Coelho.
Conflicts of interest
The authors declare no conflict of interest.
杂志排行
Asian Journal of Urology的其它文章
- Nerve-sparing robot-assisted radical prostatectomy: Current perspectives
- Robtic-assisted radical cystectomy:Literature review
- Robot-assisted retroperitoneal lymphadenectomy: The state of art
- Robotic surgery techniques to approach benign prostatic hyperplasia disease: A comprehensive literature review and the state of art
- Robotic renal and adrenal oncologic surgery:A contemporary review
- Comparison of the oncological,perioperative and functional outcomes of partial nephrectomy versus radical nephrectomy for clinical T1b renal cell carcinoma: A systematic review and metaanalysis of retrospective studies
