Hypertension and its physio-psychosocial risks factors in elderly people: a cross-sectional study in north-eastern region of Bangladesh
2021-03-03GowrangaKumarPaulMohammadMeshbahurRahmanMohammadHamiduzzamanZakiFarhanaSomareshKumarMondalSalehaAkterShaylaNazninMdNazrulIslam
Gowranga Kumar Paul, Mohammad Meshbahur Rahman, Mohammad Hamiduzzaman,Zaki Farhana, Somaresh Kumar Mondal, Saleha Akter, Shayla Naznin, Md. Nazrul Islam
1. Department of Statistics, Mawlana Bhashani Science and Technology University, Santosh, Tangail-1902, Bangladesh;2. Biomedical Research Foundation, Dhaka-1230, Bangladesh; 3. Flinders University Rural Health SA, College of Medicine & Public Health, Flinders University, South Australia, Australia; 4. Bangladesh Bank-The Central Bank of Bangladesh, Bangladesh; 5. Department of Statistics, Mawlana Bhashani Science and Technology University, Santosh,Tangail-1902, Bangladesh; 6. Asian University of Bangladesh, Dhaka, Bangladesh; 7. Department of Statistics, Mawlana Bhashani Science and Technology University, Santosh, Tangail-1902, Bangladesh; 8. Department of Statistics, Shahjalal University of Science and Technology, Sylhet, Bangladesh
Hypertension has been increasingly cited mortality cause in developing countries including Bangladesh,[1-4]and generally associated with coronary artery disease,stroke, heart failure, atrial fibrillation, peripheral vascular disease, vision loss and chronic kidney disease.[5,6]The prevalence of hypertension in developing countries is 32.3%, while this rate is 22% worldwide.[7-9]Islam, et al. reveal this prevalence is increased from 26.4% in 2011 to 40.7% in 2017 among Bangladeshi adults.[10]In Bangladesh, people aged 50 years and over tend to be acutely inclined to hypertension than any other age groups, and in more need of treatments.[11]More often, elderly people live in a resource-poor setting with limited access to education, financial assistance, active lifestyles and healthcare services, and this living circumstance resulted in a high risk of chronic hypertension and premature death.[12-15]Several researches indicate that hypertension increases with age, however, little is known about the prevalence of hypertension among elderly people and associated risk factors in Bangladesh.[6,16-18]
According to the literature, the risk factors of hypertension include age, educational attainment, economic status, Body Mass Index and health beliefs and behaviours.[11]Although preventable or manageable with pharmacological and non-pharmacological interventions,[19]all research findings in Bangladesh agree on that the frequency of hypertensive patients is increasing.[10,20-22]High number of hypertensive patients is a consequence of urbanization, food habits(i.e., malnutrition, fat and salt,low fiber food), sedentary lifestyles (i.e., physical inactivity, expose to high calorie diets), and passive health beliefs and behaviours (e.g., smoking habit,dependency on antihypertensive medications).[23,24]Complications of hypertension lead to a high proportion of cardiovascular disease-related mortality and estimated to have cost Bangladesh over $12 million every year with a projection of $36.7 billion in 2030.[25]
The risk of developing hypertension, pre-hypertensive condition and hypertension is mentally,emotionally and physically challenging, and burdensome to elderly people, their family caregivers,local healthcare services and the government. Research data on the elderly hypertensive patients are essential to illustrate the prevalence of this disease and associated physio-psychosocial risk factors, and also to help the public health leaders and clinicians to intervene the preventive and non-pharmacological treatments tailored to this cohort. Considering this context, we aimed to assess the prevalence of elderly hypertension and determined its associated physio-psychosocial risk factors in Bangladesh.
We conducted a cross-sectional research, involving an interview and an anthropometric assessment. The study protocol was designed following the ethical standards of Helsinki Declaration of 2000 and approved by University Research Centre of Shahjalal University of Science & Technology,Bangladesh (Project Number: PS/2018/1/11). We employed a single-stage cluster sampling method to recruit participants aged 50 years and over from the north-eastern (e.g., Sylhet District) region of Bangladesh. Five hundred twenty-nine participants were randomly selected from 10 sampling units(five urban residential communities and five rural residential communities) of Sylhet District. After obtaining the informed consent, health profile of each participant, i.e., self-reported health problems,biomarkers, performance of daily activities and socio-demographic information, was collected through a structured questionnaire. Necessary medical equipment (i.e., BP machine, blood sugar measurement machine and height-weight measurement machine etc.) were provided to the public health assistant and social worker to assess and collect anthropometric data. Table 1 presents the measurement system of different anthropometric indicators.
Hypertension was measured following the guidelines of American Heart Association. Participant defined hypertensive if she/he has a systolic blood pressure (SBP) ≥ 140 mmHg and/or, diastolic blood pressure (DBP) ≥ 90 mmHg and/or, receipt of an anti-hypertensive medication at time of the survey.[11]Pre-hypertension (SBP ≥ 120 mmHg but < 140 mmHg and/or DBP ≥ 80 mmHg but < 90 mmHg and/or not taking anti-hypertensive medication) and non-hypertension (SBP ≤ 120 or DBP < 80 mmHg or not taking anti-hypertensive medication)were merged together to make the variable dichotomous(i.e., hypertensive: coded as 1); non-hypertensive:coded as 0).[26]Age, education, gender, occupation,residency, marital status, body mass index, health condition, smoking, heart problem, diabetes and sleeping problem were considered as potential risk factors of hypertension and were measured based on self-reported medical history by the participants during a face-to-face interview. Body mass index was categorized into: underweight (< 18.50 kg/m2),normal weight (18.50−24.99 kg/m2) and Overweight (≥ 25.00 kg/m2).[27]In regard to heart disease, the participants were asked to provide medical evidence in favour of their response. Respondent’s diabetics was recorded as diabetic (plasma glucose level ≥ 7.0 mmol/L and/or taking diabetes medication), pre-diabetic (plasma glucose level from 6.0 to 6.9 mmol/L) and diabetes-free (plasma glucose level < 6.0 mmol/L).[28]
Frequency was calculated to describe the prevalence of hypertension among the participants. Bivariate chi-square test was used to determine the difference between expected frequencies (hypertension status) and the observed frequencies in one or moreselected categorical variable. A multivariable logistic regression analysis [crude odds ratio (COR) and adjusted odds ratio (AOR) with 95% confidence interval (CI)] was also performed to identify the significant degree of risk of hypertension. Statistical tests were considered significant atP-value < 0.001, <0.05 and < 0.1.
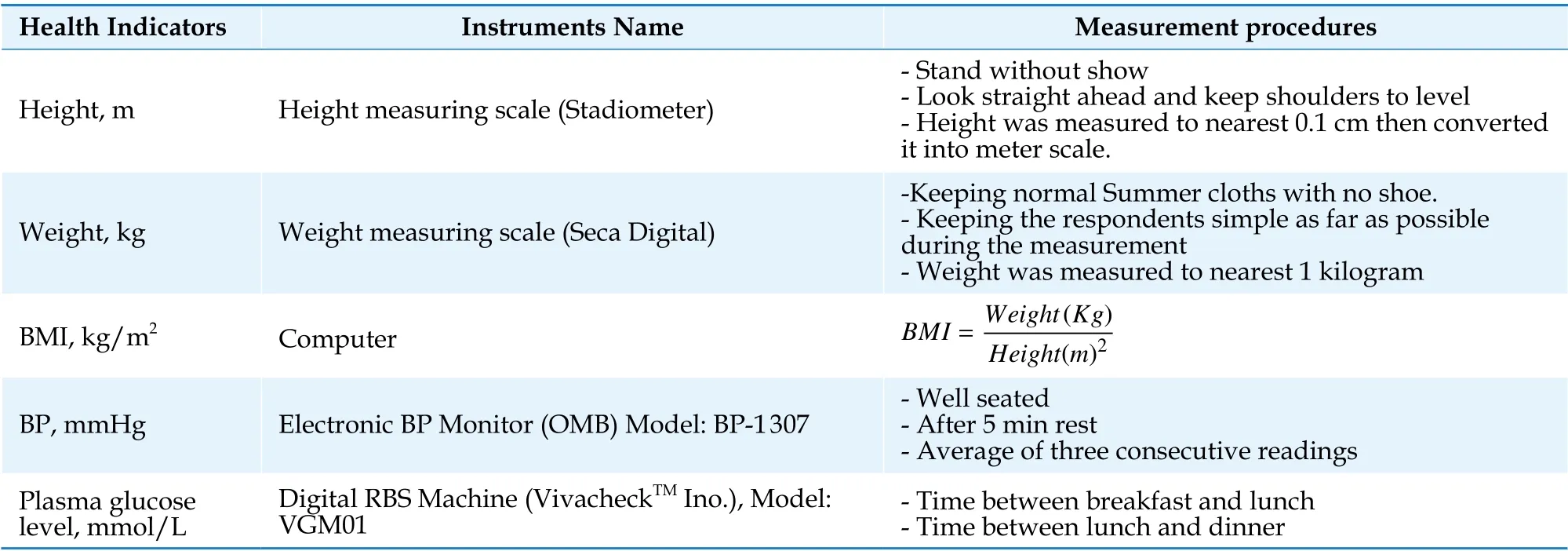
Table 1 Anthropometric measurement systems of height, weight, BMI, BP and RBS.
Figure 1 demonstrates the prevalence of hypertension among the participants and Table 2 illustrates the association between participants’ demographic and physio-psychosocial profile and hypertension status. Mean age was 60 ± 10 years) and male and female participants were 56.3% and 43.7%respectively. Overall prevalence of hypertension was 53.87% and this prevalence was higher for elderly participants (59.5%) aged 60 and over. Frequency of hypertensive participants was at increase with ageing, with an exception for ‘70−74 years’ age group. The percentage of elderly male hypertensive patients was higher than their female counterparts (male: 62%; female: 38%), whereas no significant variation found for all age-gender groups (male:53.4%; female: 54.5%). Widowed participants were more hypertensive than married (61.3%vs. 51.6%).Approximately 18.3% participants were illiterate(hypertensive: 62.9%, non-hypertensive: 37.1%);19.1% completed primary schooling (hypertensive:65.3%, non-hypertensive: 34.7%); 32.1% completed secondary schooling (hypertensive: 50%, non-hypertensive: 50%); and 30.4% had higher education(hypertensive: 45.3%, non-hypertensive: 54.7%).
The results showed that the participants with a perception of having ‘poor health’ had higher risks of hypertension than the participants who reported‘good health’ [68.9%vs. 33.9%]. Smoking (70%) and heart disease (77.5%) were the prevalent risk factors of hypertension. Almost 82.5% overweight participants were hypertensive, while 46% participants with normal body mass index and 31% underweight participants were at risk of hypertension.Additionally, hypertension significantly fluctuated for employment status, such as unemployed participants scored more in hypertension (78.6%) than employed. Urban participants (62%) demonstrated a higher prevalence of hypertension than rural participants (43.5%). The chi-square test of the association between hypertension and demographic and physio-psychosocial profile suggested that old age,widowhood, illiteracy, poor health, smoking, heart disease, overweight, diabetes, sleeping problem,unemployment and urban residency were significant risk factors for hypertension (Table 2).
Table 3 shows CORs and AORs of risk factors associated with hypertension from a binary logistic regression analysis at 95% confidence interval. The logistic regression analysis revealed an increase in the prevalence of hypertension as age increased.The prevalence of hypertension was significantly higher for ‘65−69 years’ age group (AOR = 2.298,95% CI: 1.05−5.02) compared to ‘50-54 years’ age group. Participants with higher education degrees had 1.711 times more chance (AOR: 1.711, 95% CI: 0.796−3.681) of having hypertension than illiterate participants. Both bivariate and multivariate logistic regression demonstrated that the participants having poor health condition had 4.223 (AOR: 4.223, 95%CI: 1.672−10.665) times more chance to be hypertensive than the participants with good health. Having a sound sleep at night was referred as an indicator of low hypertension. Overweight participants were at 10.513 time’s higher risk of having hypertension than underweight participants. Another identical finding was that diabetic patients had 1.850 times (COR: 1.850, 95% CI: 1.242−2.753) more chance of having hypertension their counterparts.The risk of hypertension was also found to be significantly lower (AOR: 0.664, 95% CI: 0.402−1.097)among rural residents compared to urban residents.
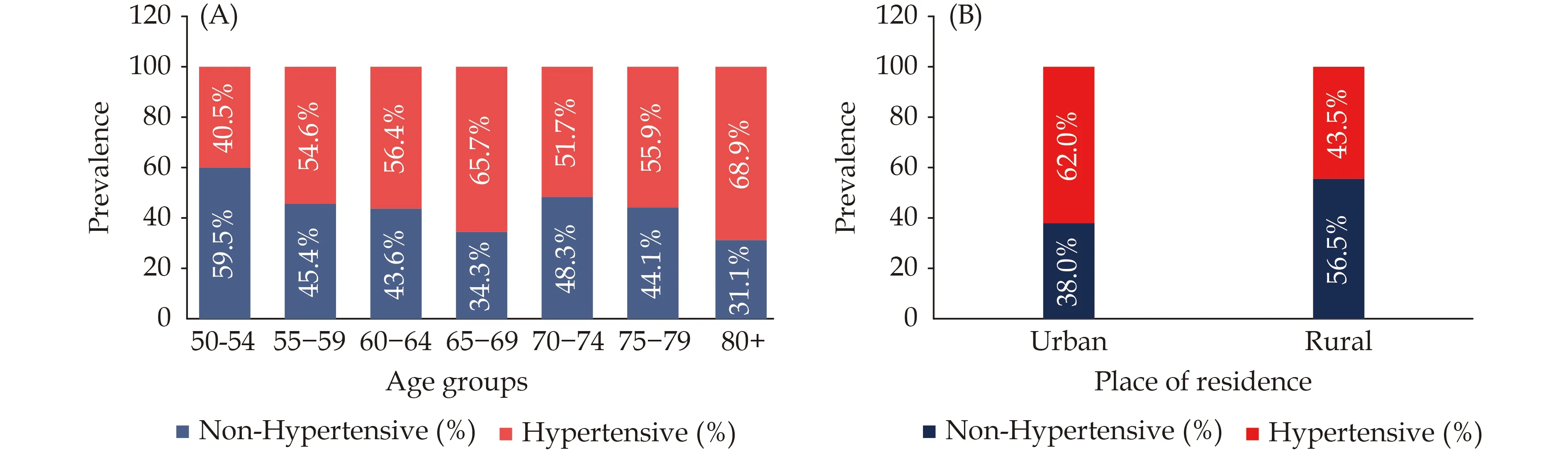
Figure 1 Distribution of the prevalence of hypertension among different groups of participants. (A): Prevalence of hypertensive and non-hypertensive patients according to age group; (B): urban-rural comparison of hypertension of the elderly.
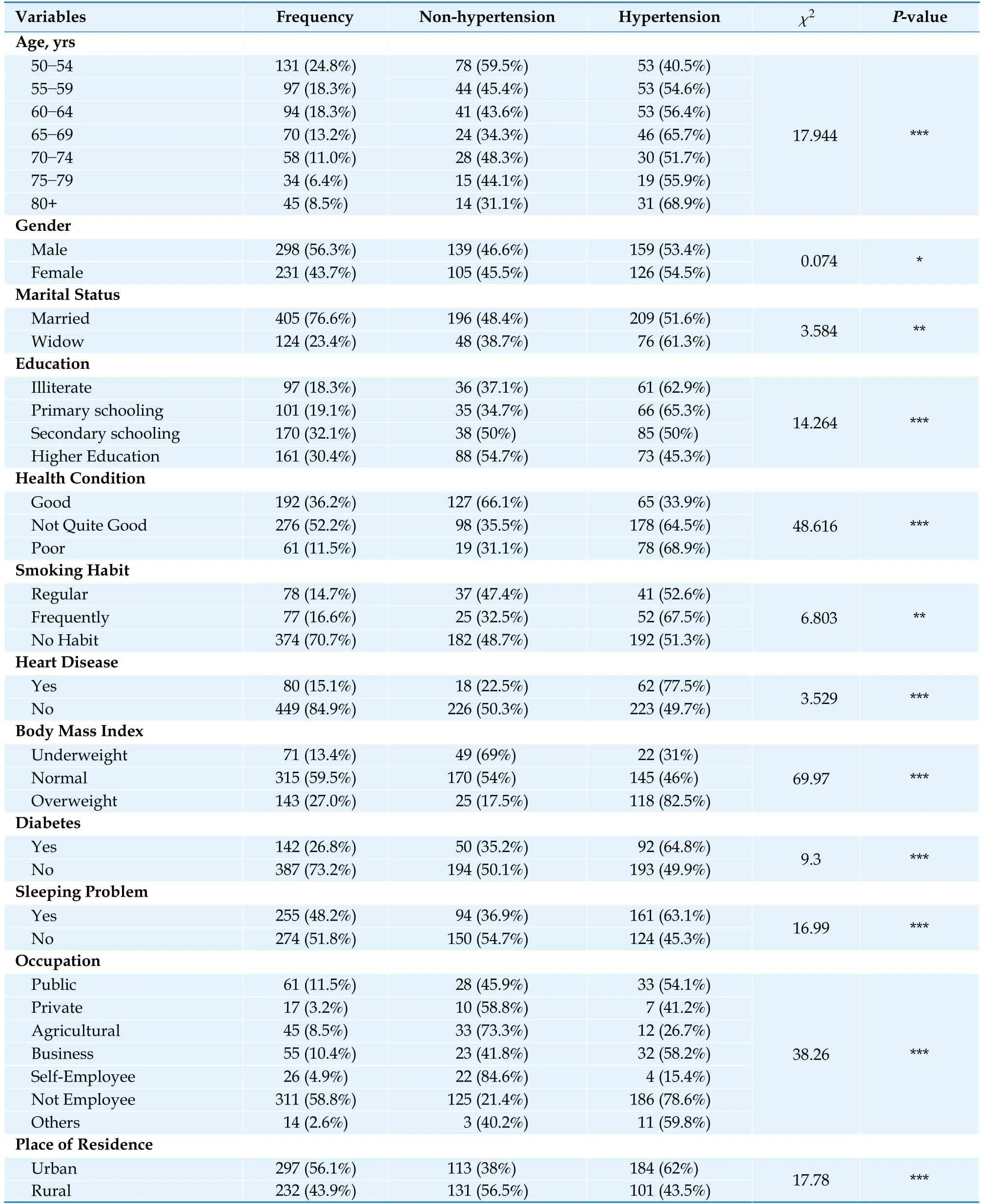
Table 2 Prevalence of hypertension by demographic and physio-psychosocial factors among the participants.
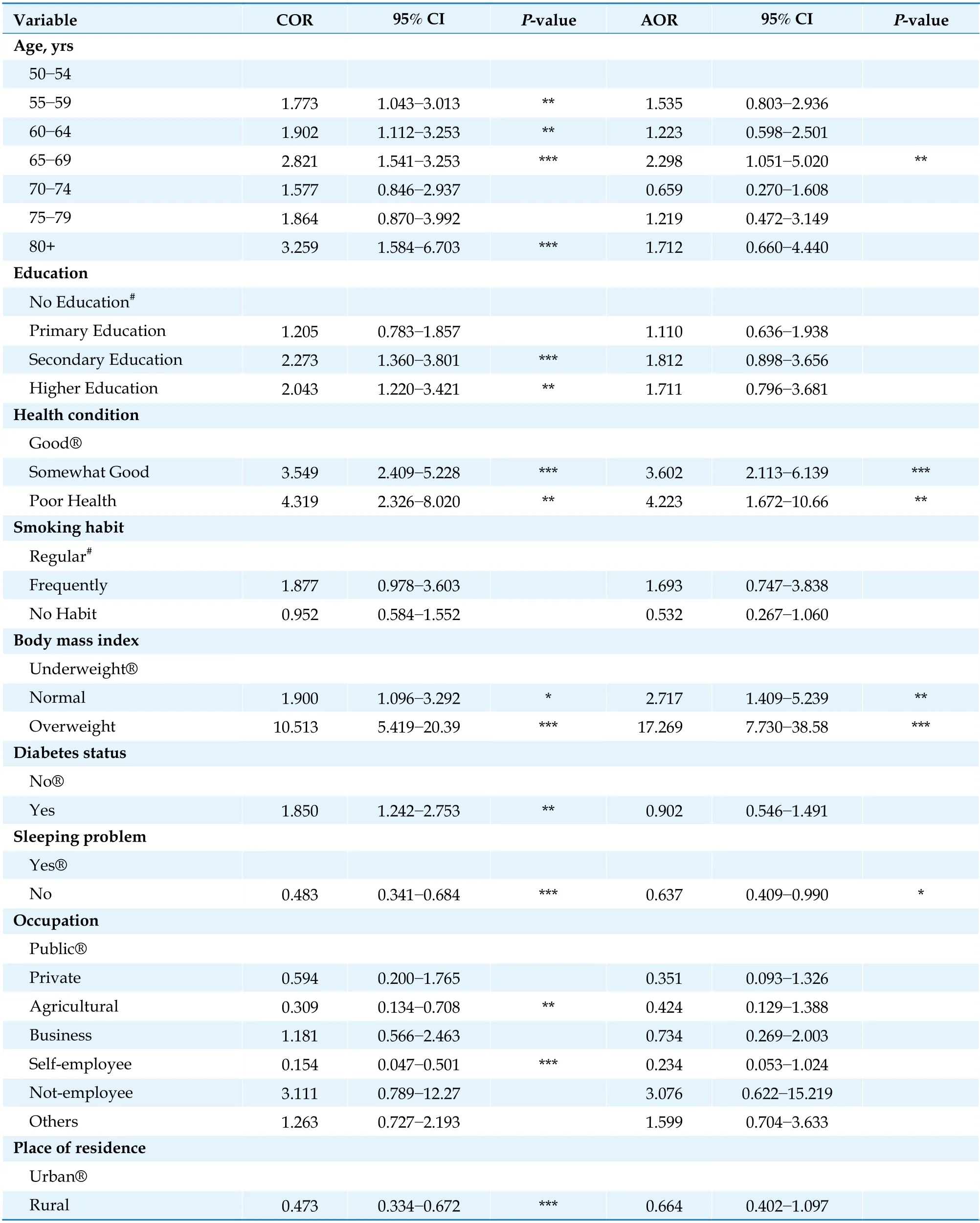
Table 3 Crude odds ratios (CORs) and adjusted odds ratios (AORs) of rick factors associated with hypertension.
We revealed a high prevalence of hypertension(59.5%) among the elderly people aged 60 years and over, and this prevalence of hypertension was significantly higher for ‘65-69 years’ age group compared to ‘50-54 years’ age group. The associated risk factors were widowhood (61.3%), literacy (62.9%),unemployment (78.6%) and smoking (67.5%). We also found that elderly hypertensive patients had an inclination to health problems including perceived poor health (68.9%), overweight (82.5%), heart disease (77.5%), diabetes (64.8%) and sleeping disorder (63.1%). These findings are consistent with previous studies conducted in Bangladesh and in other low-income countries, which investigated all age groups.[29-33]
Our focus was on the physio-psychosocial risk factors associated with elderly people’s hypertension as health problems of this cohort were not assessed regarding hypertension. It is established that factors like overweight can influence blood pressure leading to a hypertensive heart disease and a significant proportion of Sylheti people aged 50 years and over were found as overweight, as were being rich and urban community-dwellers.[34]We found that overweight and diabetes of elderly people were significantly related with their hypertension, which is consistent with other studies carried out in Bangladesh and India.[6,35]The relationship between overweight and hypertension is well known, therefore, further studies are warranted to determine the factors that affect obesity. It is been increasingly documented that elderly people with smoking habit and sleeping disorder experience the burden of hypertension.[36,37]In addition, perceived poor health often means a hypertension for elderly people, especially who live in low-income countries like Bangladesh.[34]
In this study, the prevalence of hypertension was higher in elderly men than women, and this is inconsistent with studies investigated the reasons of hypertension between men and women.[38]Reasons for men being more prone to hypertension in lowincome countries includes stress, alcohol consumption and smoking.[39]Moreover, hypertension was prevalent among urban elderly men than urban elderly women and rural elderly men and women. One cause of high hypertension rate in urban elderly men is that they are engaged in low physical activities and burn low calories resulting in high Body Mass Index.[40]Hypertension is also related by researchers with literacy and it is generally assumed that educated persons are more aware about hypertension than illiterate.[39]Interestingly, we found reverse result, and this can be an indication that engaged in official jobs that adhere low physical activities and high level of work-place stress place educated people at risk of hypertension. According to the literature, employment is a vital risk factor in elderly people’s hypertension, and it seems having no job creates a vulnerability of no or little income and make these people dependent on their family members.[12,14]An anxiety along with multi-morbidity and chronic conditions are common among Bangladesh elderly people and due to which they experience chronic hypertension leading to heart strokes and other heart related problems.
There are a few limitations in this study: firstly,causal relationships between the variables were not determined because of the nature of cross-sectional research; secondly, measurements of hypertension and its associated risk factors are mainly a prevalence measurement; and finally, this study did not focus into the effects of clinical and public health interventions on hypertension.
In conclusion, we demonstrate a high prevalence of hypertension among Sylheti Elderly people regardless of gender and associated physio-psychosocial risk factors, for example, overweight, diabetes,smoking, sleeping disorder, sedentary lifestyle, literacy and unemployment. These findings have several implications as the number of elderly population has been increasing in Bangladesh: (1) modification of the National Guidelines for Clinical Management of Hypertension in Bangladesh with specific attention on the integration of physiopsychosocial risk factors in defining elderly hypertensive patients and personalised care approach in treatment; (2) Clinicians and local public health officers should focus on lifestyle change or non-pharmacological intervention in reducing tobacco consumption rate; (3) educate the family members to understand the importance of active lifestyle and relationship needs of elderly people that reduce anxiety; (4) develop and use elderly patient activation toolkit to reduce obesity, risk of diabetes and sleeping problem; and (5) peer education for elderly people to improve their health literacy and maintain healthy lifestyle.
杂志排行
Journal of Geriatric Cardiology的其它文章
- Journal of Geriatric Cardiology
- Potassium variability during hospitalization and outcomes after discharge in patients with acute myocardial infarction
- Beta-blocker therapy in elderly patients with renal dysfunction and heart failure
- Obstructive sleep apnea increases heart rhythm disorders and worsens subsequent outcomes in elderly patients with subacute myocardial infarction
- Sex modification of the association of the radial augmentation index and incident hypertension in a Chinese communitybased population
- Neurohumoral, cardiac and inflammatory markers in the evaluation of heart failure severity and progression
