溃疡性结肠炎患者活动期肠道菌群及粪便炎症标志物检测及其临床意义
2021-01-28陈茜茜朱海勇
陈茜茜 朱海勇
[摘要] 目的 观察溃疡性结肠炎患者活动期肠道菌群及粪便炎症标志物含量及其临床意义。 方法 回顾性分析2018年3月至2021年1月在我院治疗的60例溃疡性结肠炎患者的临床资料,按照病情状况分为活动期组(n=39)与缓解期组(n=21),同时选择在我院体检的50名健康者为对照组。比较三组研究对象的肠道需氧菌群(包括酵母菌、肠球菌、葡萄球菌、肠杆菌)、厌氧菌群(包括双歧杆菌、拟杆菌、乳杆菌、真杆菌、消化球菌)以及粪便炎症标志物乳铁蛋白(LF)、钙卫蛋白(FC)、髓过氧化酶(MPO)、基质金属蛋白酶-9(MMP-9)的水平。 结果 活动期组酵母菌、肠球菌、葡萄球菌、肠杆菌数量明显高于缓解期组与对照组,缓解期组酵母菌、肠球菌、肠杆菌数量明显高于对照组(P<0.05);活動期组双歧杆菌、乳杆菌、真杆菌明显低于缓解期组与对照组,拟杆菌、消化球菌明显高于缓解期组与对照组,缓解期组双歧杆菌、乳杆菌、真杆菌明显低于对照组,拟杆菌、消化球菌明显高于对照组(P<0.05);活动期组LF、FC、MPO、MMP-9水平明显高于缓解期组与对照组,缓解期组LF、FC、MPO、MMP-9水平明显高于对照组(P<0.05)。 结论 溃疡性结肠炎患者肠道菌群失调,粪便中炎症标志物水平明显较高,能够通过肠道菌群变化及粪便内LF、FC、MPO、MMP-9水平评估疾病的活动性。
[关键词] 溃疡性结肠炎;活动期;需氧菌群;厌氧菌群;乳铁蛋白;钙卫蛋白;髓过氧化酶;基质金属蛋白酶-9
[中图分类号] R574.62 [文献标识码] A [文章编号] 1673-9701(2021)34-0016-04
[Abstract] Objective To observe the levels of intestinal flora and fecal inflammation markers in patients with ulcerative colitis and its clinical significance. Methods The clinical data of 60 patients with ulcerative colitis admitted to our hospital from March 2018 to January 2021 were retrospectively analyzed. According to their condition, the patients were divided into the active period group(n=39) and the remission period group(n=21). At the same time, 50 healthy people who had a physical examination in our hospital were selected as the control group. The intestinal aerobic flora (including yeast, enterococcus, staphylococcus, and enterobacteriaceae), the anaerobic flora(including bifidobacterium, bacteroides, lactobacillus, eubacterium, peptococcus), and the fecal inflammation markers lactoferrin(LF), calprotectin (FC), myeloperoxidase (MPO), matrix metalloproteinase-9 (MMP-9) between the three groups were compared and analyzed. Results The numbers of enterococcus, staphylococci, and enterobacteriaceae in the active stage group were significantly higher than those in the remission stage group and the control group. The numbers of yeast, enterococcus, and enterobacteriaceae in the remission stage group were significantly higher than those in the control group. The differences were statistically significant(P<0.05). The bifidobacterium, lactobacillus, eubacteria in the active period group were significantly lower than those in the remission stage group and the control group. The bacteroides and peptococcus in the active period group were significantly higher than those in the remission stage group and the control group. The bifidobacterium, lactobacillus, and eubacteria in the remission stage group were significantly lower than those in the control group. The bacteroides and peptococcus in the remission stage group were significantly higher than those in the control group. The differences were statistically significant (P<0.05). The levels of LF, FC, MPO, and MMP-9 in the active stage group were significantly higher than those in the remission group and the control group. The levels of LF, FC, MPO, and MMP-9 in the remission stage group were significantly higher than those in the control group, and the differences were statistically significant(P<0.05). Conclusion In patients with ulcerative colitis, the intestinal flora is imbalanced, and the level of fecal inflammatory markers is significantly higher. The activity of the disease can be assessed by the changes in the intestinal flora and the levels of LF, FC, MPO, and MMP-9 in feces.
[Key words] Ulcerative colitis; Active stage; Aerobic flora; Anaerobic flora; Lactoferrin; Calprotectin; Myeloperoxidase; Matrix metalloproteinase-9
溃疡性结肠炎的发病原因还没有完全明确,现在大多数学者认为是由遗传易感、环境、免疫功能不正常、肠道屏障功能出现障碍等诸多原因引发,其中,免疫应答紊乱与慢性炎症反应为引发溃疡性结肠炎的重要环节,肠道中的菌群紊亂是导致免疫应答变化、炎症反应的一个关键因素,是发生溃疡性结肠炎的关键因素[1-3]。近几年,多项文献[4-5],肠道内菌群的不协调与溃疡性结肠炎息息相关。通常来说炎症性肠病肠道内的菌群组成变化主要有多样性减少、黏膜总菌改变、于疾病进展期菌群组成变化,像增加侵袭性细菌的类型、减少保护性菌的数量[6]。溃疡性结肠炎患者的肠黏膜屏障于肠道炎症发生后受损,经由受损的肠黏膜屏障,中性粒细胞进入肠腔,通过粪便排出,所以,粪便内的中性粒细胞衍生产物乳铁蛋白(Lactoferrin,LF)、钙卫蛋白(Fecal calprotectin,FC)、髓过氧化酶(Myeloperoxidase,MPO)、基质金属蛋白酶-9(Matrix metalloproteinase-9,MMP-9)等往往被用于肠道炎症评估[7-8]。但是国内少有医疗机构对溃疡性结肠炎患者的粪便做相应的菌群分析,因而本院在患者入院后对菌群进行分析。基于此,本研究回顾性分析我院诊治的溃疡性结肠炎患者的临床资料,观察其活动期肠道菌群及粪便炎症标志物检测及其临床意义,现报道如下。
1 资料与方法
1.1 一般资料
回顾性分析2018年3月至2021年1月在我院治疗的60例溃疡性结肠炎患者的临床资料,本研究经本院医学伦理委员会批准同意,且所有患者均知情同意。纳入标准:符合溃疡性结肠炎的相关标准者[9]。排除标准:①处于哺乳期、妊娠期的妇女;②合并其他免疫系统疾病者;③合并恶性肿瘤者;④使用糖皮质激素、免疫调节剂、免疫抑制剂、益生菌进行治疗的患者。按照病情状况分为活动期组(n=39)与缓解期组(n=21)。活动期组男23例,女16例;年龄21~49岁,平均(28.69±8.11)岁;病程0.5~18.5年,平均(9.57±5.48)年。缓解期组男7例,女14例;年龄20~51岁,平均(29.06±8.21)岁;病程1~19年,平均(9.88±5.36)年。同时选择在我院体检的50名健康者为对照组,男29例,女21例;年龄19~52岁,平均(29.57±7.38)岁。两组患者的基本资料比较,差异无统计学意义(P>0.05),具有可比性。
1.2 方法
所有研究对象在结肠镜检查日留取5~10 g新鲜粪便,于无菌便盒内密闭保存,30 min之内送检。
1.2.1 直接涂片镜检与分析菌群 对粪便标本进行涂片,面积为1.5 cm×2.0 cm左右,厚度像血膜的菌膜,于干燥固定之后格兰染色,借助油镜对视野(10个)进行观察,按照各油镜视野下细菌总数同各类细菌的比值,对菌群是否失调及失调的程度进行判断,分级及判断标准依据《肠道菌群粪便涂片检查图谱》[10]。
1.2.2 细菌培养鉴定 选择接种环10 μL取一环粪便,使用四区划线法实施接种。①需氧培养,麦康凯平板与血平板接种,于37℃且包括5%体积分数的CO2的有氧环境内孵育24 h,选择VITEK 2全自动细菌鉴定仪(生物梅里埃公司)对需氧菌群(包括酵母菌、肠球菌、葡萄球菌、肠杆菌)进行检测。②厌氧培养:厌氧血平板接种,于无氧且37℃的环境内孵育48 h,之后进行耐氧试验,选择API 20A厌氧菌鉴定卡(北京千舜生物科技有限公司)鉴定厌氧菌群(包括双歧杆菌、拟杆菌、乳杆菌、真杆菌、消化球菌)。
1.2.3 粪便炎症标志物检测 选择生理盐水稀释粪便标本,然后进行离心,选取上清液,使用酶联免疫吸附法对LF、FC、MPO、MMP-9水平进行检测,试剂盒都由南京建成科技有限公司提供。
1.3 统计学方法
应用SPSS 20.0 统计学软件进行分析,计量资料以均数±标准差(x±s)表示,多组比较采用方差分析,两两比较采用t检验,P<0.05为差异有统计学意义。
2 结果
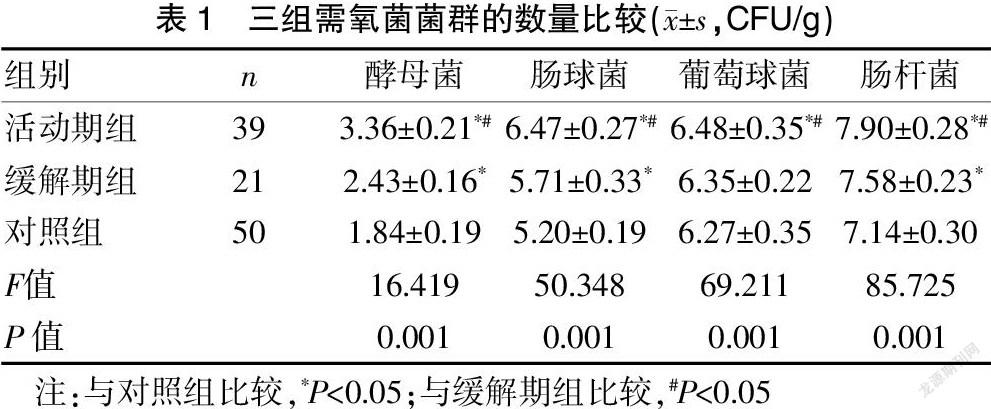
2.1 三组需氧菌菌群的数量比较
活动期组酵母菌、肠球菌、葡萄球菌、肠杆菌数量明显高于缓解期组与对照组,缓解期组酵母菌、肠球菌、肠杆菌数量明显高于对照组,差异有统计学意义(P<0.05)。见表1。
2.2 三组厌氧菌菌群的数量比较
活动期组双歧杆菌、乳杆菌、真杆菌明显低于缓解期组与对照组,拟杆菌、消化球菌明显高于缓解期组与对照组;缓解期组双歧杆菌、乳杆菌、真杆菌明显低于对照组,拟杆菌、消化球菌明显高于对照组,差异均有统计学意义(P<0.05)。见表2。
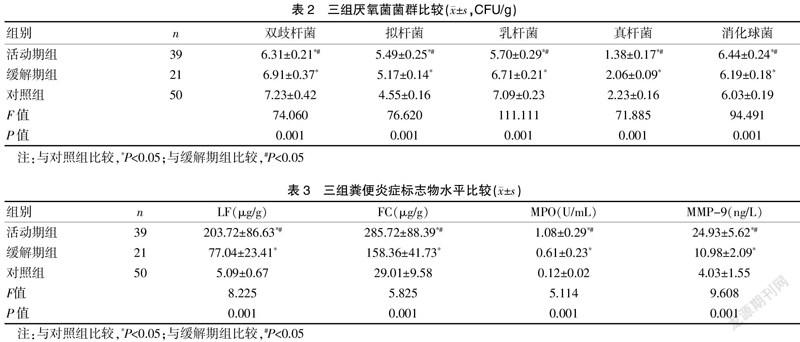
2.3 三组粪便炎症标志物水平比较
活动期组LF、FC、MPO、MMP-9水平明显高于缓解期组与对照组,缓解期组LF、FC、MPO、MMP-9水平明显高于对照组,差异均有统计学意义(P<0.05)。见表3。
3 讨论
溃疡性结肠炎属于常见胃肠道的非特异性慢性疾病,此病临床特征和体征轻重缓急会交替变换,具有不一致性,患者既可出现全身症状,也会仅出现结肠症状[11]。相关文献显示,发生溃疡性结肠炎的原因同肠道菌群、免疫、遗传以及环境等因素息息相关。肠道内的优势菌群同人体的免疫系统会维持动态平衡,通常肠道免疫系统不将这些共生菌群看作非己,所以耐受于其免疫系统,然而若肠道出现慢性炎症,这类细菌会大量增殖,导致肠道免疫屏障被破坏,肠黏膜免疫功能被抑制,从而导致人体肠道出现免疫反应,引发溃疡性结肠炎[12-14]。然而具体的机制目前尚不明确,同炎性因子是否相关仍有待分析。