10例面部黑素瘤患者的临床与病理分析
2021-01-16刘小青才琴曹静樊俊威边毅万学峰
刘小青 才 琴 曹 静 樊俊威 边 毅 万学峰



[关键词]面部;黑素瘤;临床病理;慢Mohs显微描记手术
[中图分类号]R739.5 [文献标志码]A [文章编号]1008-6455(2021)12-0082-04
Clinical and Pathological Analysis of 10 Patients with Facial Melanoma
LIU Xiao-qing1,2,CAI Qin2,CAO Jing2,FAN Jun-wei2,BIAN Yi2,WAN Xue-feng2
(1.Department of Dermatology,Suzhou Dushu Lake Hospital(Dushu Lake Hospital Affiliated to Suzhou University),Suzhou 215125,Jiangsu,China;2.Department of Dermatology, the First Affiliated Hospital of Xinjiang Medical University,Urumqi 830054,Xinjiang,China]
Abstract: Objective To investigate the clinical and pathological features of melanoma. Methods 10 cases of facial melanoma diagnosed in the Department of Dermatology, the First Affiliated Hospital of Xinjiang Medical University and removed by Slow Mohs micrographic surgery were retrospectively analyzed and collected clinicopathological data and treatment of the patients. Results Facial melanoma is usually clinically manifested as patches with unclear boundaries, papules and nodules of varying sizes can be seen on them, and some nodules can be ulcerated; in histopathology, they are manifested as epidermal atrophy and epidermal junctions. Or the superficial and middle dermis can be seen in nests or scattered heterosexual black cells, growing along the basal layer, and sunlight elastic fibrosis can be seen in the superficial and middle dermis, with slow Mohs micrography, the negative rate of one-time surgical resection was low, and the tumor could be completely removed only after 2 to 3 times of dilatation. Conclusion The skin lesions of facial melanoma patients were located at the exposure site, with unclear boundaries and obvious skin atrophy. When the surgical expansion range was determined according to the thickness of Breslow, the one-time surgical resection net rate was only 30%, but it was higher in the cases with active tumor lymphocyte infiltration.
Key words: facial; melanoma; flinicopathology; slow Mohs micrographic surgery
皮膚恶性黑素瘤是来源于皮肤基底层异常增生的黑素细胞,发病原因尚不十分清楚,发病相关因素有家族史、不典型痣、紫外线、外伤等[1]。面部黑素瘤临床多表现为边界不清、颜色不均一的斑疹,手术切除后复发率高[2]。现总结确诊的10例面部黑素瘤患者的临床、病理及手术预后情况。
1 资料和方法
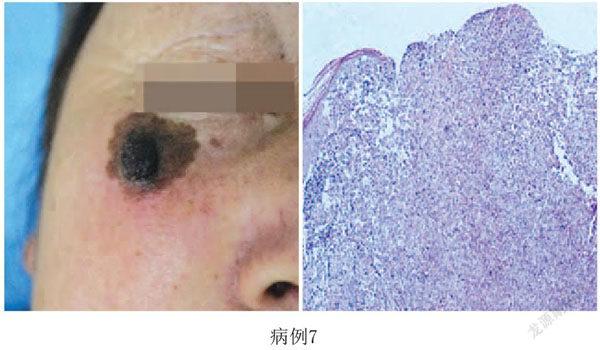
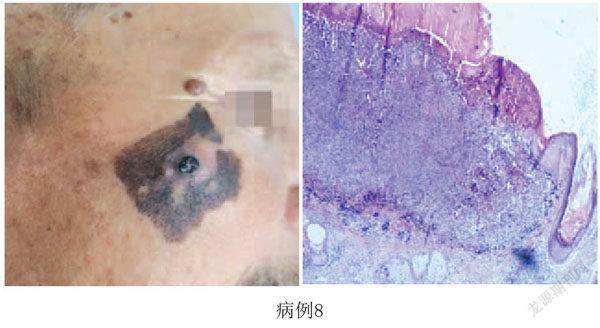
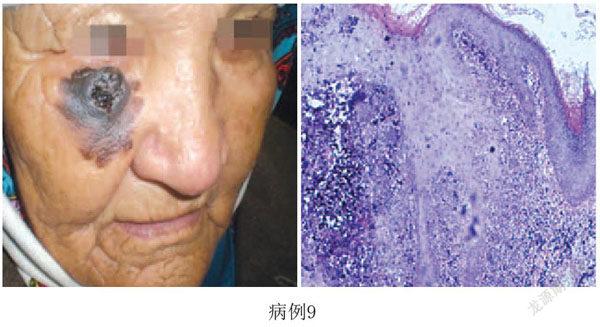
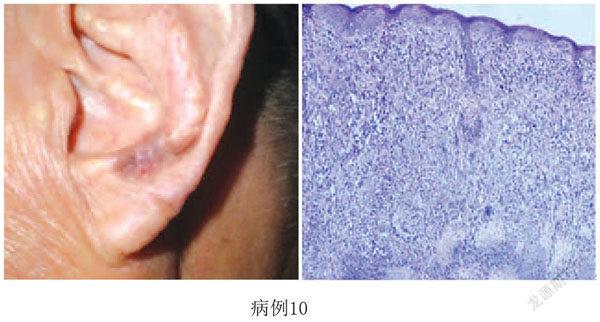
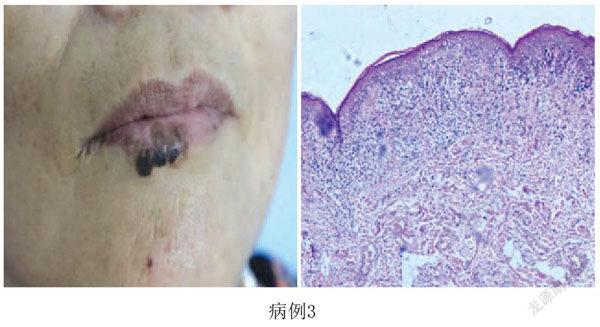
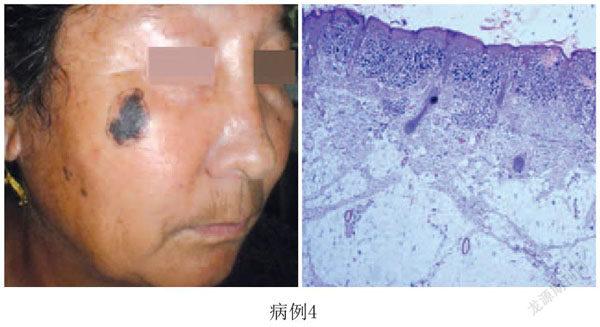
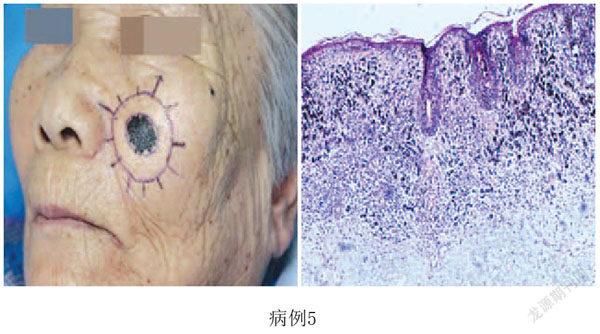
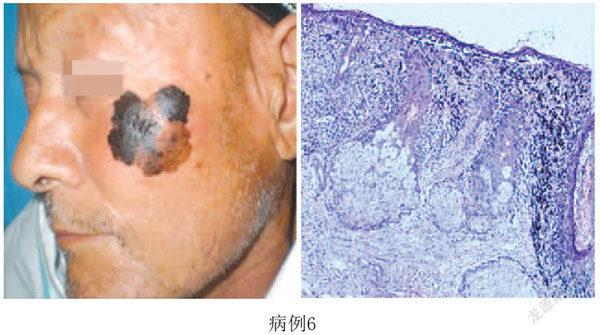
1.1 一般资料:收集2018年7月-2020年5月于笔者科室确诊并发生在面部的10例黑素瘤患者临床及病理资料。10例患者,其中女7例,男3例;汉族3例,少数民族7例;平均年龄64岁(43~79岁),病程2~20年,肿瘤大小2~5.5cm,8例肿瘤位于面颊、1例下唇、1例耳廓,其中6例皮损表面出现丘疹、结节,4例表面出现溃疡,1例皮损中央出现肿瘤消退现象。见表1,图1。同时再次审阅病理切片以进一步核对诊断,并明确病理分型。
1.2 方法:在住院期间,完善实验室检查、浅表淋巴结超声及PET-CT等相关检查,除外淋巴结及远处转移,在患者可耐受手术的情况下,局麻下行慢Mohs显微描记手术,根据黑素瘤诊治指南及规范确定手术扩切范围[3-4]。
1.2.1 黑素瘤扩切范围:①原位黑素瘤:扩切范围为0.5~1cm;②侵袭性黑素瘤:Breslow≤1mm,扩切范围1cm;Breslow>1~2mm,扩切范围1~2cm;Breslow>2~4mm,扩切范围2cm;Breslow≥4mm,扩切范围2cm。临床上均有黑素瘤的ABCDE表现:A.(Asymmetry)不对称;B.(Border irregularity)边界不规则;C.(Color variation)颜色不均匀;D.(Diameter)直径大于6mm;E.(Evolving或Elevation)进展或隆起。
1.2.2 Clark分级:指皮肤黑素瘤的浸润深度,分为5级。Ⅰ级表示肿瘤细胞局限于表皮层(原位黑素瘤);Ⅱ级表示肿瘤细胞浸润真皮乳头层但尚未充满真皮乳头层;Ⅲ级表示肿瘤细胞充满真皮乳头层到达乳头层和网状层交界处;Ⅳ级表示肿瘤细胞浸润真皮网状层;Ⅴ级表示肿瘤细胞浸润皮下组织。
TIL:肿瘤浸润淋巴细胞(Tumor infiltrating lymphocyte);LM:恶性雀斑样痣(Lentigo maligna)为原位黑素瘤;LMM:恶性雀斑样痣黑素瘤(Lentigo maligna melanoma)为侵袭性黑素瘤。
2 结果
皮肤病理学检查中(见表1病理特点部分),10例标本均有表皮萎缩,肿瘤细胞核大、异形,沿表皮基底层呈一定程度的水平生长以及附属器受累,真皮浅层日光弹力纤维变性等情况;免疫组化染色中S-100、HMB-45、Melan-A染色均阳性。3例为原位黑素瘤,病理类型为恶性雀斑样痣(LM),Clark分级为Ⅰ级,其中2例标本中肿瘤浸润淋巴细胞(TIL)缺如,1例标本中TIL表现为活跃;7例侵袭性黑素瘤病理类型为恶性雀斑样黑素瘤(TIL),Clark分级集中在Ⅳ~Ⅴ级,其中5例标本中TIL表现为不活跃,2例标本中TIL表现为活跃。
在慢Mohs显微描记手术中,根据黑素瘤诊治指南及规范确定手术扩切范围中,仅有3例一次性切净,4例经过两次手术后切净,另外3例经过三次手术后才完全清除了肿瘤组织。LM切净所需的平均扩切范围为10.7mm,LMM平均扩切范围为16.1mm。上述患者术后定期门诊复访,目前未见复发。
3 讨论
面部黑素瘤多发生在中老年患者曝光部位,大部分患者真皮层可出现明显弹力纤维变性,提示面部黑素瘤多与长期接受紫外线照射有关[5]。面部黑素瘤的病理类型多为恶性雀斑样痣和恶性雀斑样黑素瘤,该型黑素瘤临床上通常境界不清,水平方向上存在亚临床扩散,一般的扩大切除具有较高的复发率[6-7]。国内黑素瘤类型主要为肢端型[8],研究多集中在肢端雀斑痣样黑素瘤,对LM和LMM研究较少。
目前存在的问题是黑素瘤的扩切范围是根据Breslow厚度确定的,该研究发现面部黑素瘤患者的年龄偏大,由于皮损位于曝光部位,皮肤存在一定程度的萎缩,部分患者的表皮仅有3~5层角质所形成的细胞组成,测量其厚度仅为50~100μm,真皮层明显变薄,肿瘤细胞一旦突破基底层,将很快侵袭至真皮网状层,甚至脂肪层,此时实际测定的Breslow厚度可能仍不超过1mm。如果现在仅根据Breslow厚度制定扩切范围,导致一次性手术切净率低,多次手术增加了患者的痛苦。
既往的研究中,大家更多关注的是临床与病理之间的联系,如肿瘤的Breslow厚度、有无溃疡形成,以及Clark分级、患者年龄、肿瘤大小、肿瘤细胞的水平生长、日光弹力纤维变性等情况[9];很少关注肿瘤浸润淋巴细胞的数量、皮肤萎缩现象。本研究发现当TIL活跃时,一次性手术切净率可明显提高,可能与炎症细胞一定程度上限制了肿瘤的扩散有关。同时发现,LM切净所需的平均扩切范围为10.7mm,LMM平均扩切范围为16.1mm;与Maria等报道[10]LM的手术边缘阴性所需的平均范围为9.3mm,而LMM为13.7mm接近。我们希望通过分析患者临床表现及病理特点,能够对面部黑素瘤手术治疗提供参考,建议在制定面部黑素瘤扩切范围时,不仅要考虑Breslow厚度,同时也要关注Clark分级、肿瘤大小、肿瘤细胞的水平生长、TIL活跃度以及皮肤萎缩等情况,实际的手术扩切范围可能会大于指南所推荐。
[参考文献]
[1]董小龙,马勇光,杨欣.皮肤恶性黑色素瘤诊断及外科治疗策略[J].中国美容医学,2016,25(6):108-112.
[2]Connolly KL,Hibler BP,Lee EH,et al.Locally recurrent lentigo maligna and lentigo maligna melanoma:characteristics and time to recurrence after surgery[J].Dermatol Surg,2017,43(6):792-797.
[3]Prc N.Chinese guidelines for diagnosis and treatment of melanoma 2018(English version)[J].Chin J Cancer Res,2019,31(4):578-585.
[4]Coit DG,Thompson JA,Albertini MR,et al.Cutaneous melanoma,version 2.2019,NCCN clinical practice guidelines in oncology[J].J Natl Compr Canc Netw,2019,17(4):367-402.
[5]Mills AM,Policarpio-Nicholas ML,Agaimy A,et al.Sclerosing microcystic adenocarcinoma of the head and neck mucosa:a neoplasm closely resembling microcystic adnexal carcinoma[J].Head Neck Pathol,2016,10(4):501-508.
[6]Wen X,Li D,Zhao J,et al.Time-varying pattern of recurrence risk for localized melanoma in China[J].World J Surg Oncol,2020,18(1):6.
[7]徐爽,劉珍.头颈黏膜恶性黑色素瘤远处转移的危险因素[J].中国老年学杂志,2020,40(4):736-738.
[8]中国抗癌协会肉瘤专业委员会软组织肉瘤及恶性黑色素瘤学组.皮肤和肢端恶性黑色素瘤的外科治疗规范中国专家共识1.0[J].中华肿瘤杂志,2020,42(2):81-93.
[9]王雷,廖文俊,王刚,等.恶性雀斑样黑素瘤6例临床及组织病理学分析[J].临床皮肤科杂志,2010,39(10):609-611.
[10]Maria J,Quintanilla-Dieck,Christopher K,et al.Management of early-stage melanoma.[J].Facial Plast Surg Clin North Am,2019,27(1):35-42.
[收稿日期]2020-11-03
本文引用格式:刘小青.10例面部黑素瘤患者的临床与病理分析[J].中国美容医学,2021,30(12):82-85.
