Non-alcoholic fatty liver disease later diagnosed as myotonic dystrophy
2021-01-13NaokiTanakaTakefumiKimuraNaoyukiFujimoriYasuyukiIchiseKenjiSanoAkiraHoriuchi
Naoki Tanaka,Takefumi Kimura, Naoyuki Fujimori, Yasuyuki Ichise, Kenji Sano, Akira Horiuchi
Naoki Tanaka, Department of Metabolic Regulation, Shinshu University School of Medicine, Matsumoto 390-8621, Japan
Takefumi Kimura, Naoyuki Fujimori, Department of Gastroenterology, Shinshu University School of Medicine, Matsumoto 390-8621, Japan
Yasuyuki Ichise, Akira Horiuchi, Digestive Disease Center, Showa Inan General Hospital, Komagane 399-4117, Japan
Kenji Sano, Department of Pathology, Iida Municipal Hospital, Iida 395-8502, Japan
Abstract
Key Words: Non-alcoholic fatty liver disease; Non-alcoholic steatohepatitis; Frontal baldness; Cataract; Creatine kinase
INTRODUCTION
Non-alcoholic fatty liver disease (NAFLD) is a common cause of persistent liver dysfunction and is defined as the presence of hepatic steatosis without regular consumption of ethanol or drugs[1,2].For the diagnosis of NAFLD, other causes of chronic liver injury, such as hepatitis virus infection, bacterial and parasitic infection, autoimmunity, drugs and toxicants, hemochromatosis, Wilson disease, and citrin deficiency should be excluded.Additionally, the possibility of secondary NAFLD, including gastrointestinal/pancreatic surgery, hypothyroidism, hyperadrenalism, and pancreatic exocrine insufficiency, needs to be carefully surveyed[3,4].
Although it is accepted that endocrine/metabolic disorders are closely associated with the development of NAFLD, the relationship between myopathy and NAFLD has not been fully addressed.Among several types of myopathy, myotonic dystrophy (MD) is often accompanied by metabolic/endocrine disorders, such as dyslipidemia, central obesity, insulin resistance, and hypogonadism[5].Due to considerable variation in the severity and progression of myopathy, MD patients with minimal-to-mild muscle symptoms may be followed as having other diseases.We herein describe a patient with non-alcoholic steatohepatitis (NASH), a severe phenotype of NAFLD, later diagnosed as having MD.
CASE PRESENTATION
Chief complaints
A 40-year-old non-obese man without a history of regular ethanol consumption was referred to our hospital due to persistent hypertransaminasemia and hyperlipidemia.
History of present illness
It was pointed out that he had liver dysfunction and hyperlipidemia at annual health checkups from 35 years of age.He had noticed easy fatigability, but presumed that it was caused by overwork and insufficient sleep.He had no history of regular ethanol, drugs, or supplements consumption, or smoking.
History of past illness
He had no history of past blood transfusion, surgical treatment, or acupuncture.
Physical examination
His body mass index was 23.4 kg/m2.He was asymptomatic with no signs of hepatomegaly, xanthoma, or Achilles tendon thickening.
Laboratory examinations
Laboratory findings revealed significant increases in serum aspartate aminotransferase (65 U/L, normal 13-30), alanine aminotransferase (103 U/L, normal 7-23), total cholesterol (298 mg/dL, normal 142-220), and triglycerides (TG; 318 mg/dL, normal 30-150).Hyperinsulinemia and greater index of homeostasis model assessment for insulin resistance indicated the presence of insulin resistance.Hepatitis virus markers and autoantibodies were all negative and immunoglobulins, ferritin and ceruloplasmin were within normal ranges.Laboratory data at the time of liver biopsy are shown in Table 1.
Imaging examinations
Abdominal ultrasonography revealed hyperechogenic liver parenchyma with deep attenuation, indicating the presence of steatosis.
Further work-up
A percutaneous liver biopsy was conducted to evaluate his persistent liver dysfunction.Liver histology showed macrovesicular steatosis, ballooned hepatocytes with eosinophilic inclusion bodies (Figure 1A, arrows), and perisinusoidal fibrosis (Figure 1B), which led to the diagnosis of NASH.According to the criteria proposed by Kleineret al[6], the score for steatosis, lobular inflammation, and hepatocyte ballooning were 2 (moderate), 1 (few), and 1 (few), respectively, for a total NAFLD activity score of 4.Bezafibrate (400 mg/d) was commenced for his hypertriglyceridemia.
A blood examination to assess the effects of fibrate treatment 1 mo later revealed elevated levels of creatine kinase (CK; 757 U/L, normal 62-287) and myoglobin.The patient denied any symptoms of muscle pain, weakness, or dark urine.The abnormalities in serum CK and myoglobin persisted despite immediate cessation of the fibrate.Thyroid function was normal.
The patient’s face was closely inspected again (Figure 2).He had frontal baldness at the age of 40 and a hatchet face.Manual muscle testing demonstrated that he was very slow opening his hands after grasping forcefully (i.e., grip myotonia).Careful history taking revealed a prior cataract operation.These findings indicated the possibility of MD.
MD is an autosomal dominant disease that affects the dystrophia myotonica protein kinase (DMPK) gene on chromosome 19[5].The expansion of CTG trinucleotide repeats in the 3’ untranslated region of this gene results in the retention of an expanded RNA repeat that is directly toxic to myocytes.Southern blotting of the patient’s DNA after BamHI digestion detected an additional band caused by CTG repeats (Figure 3), confirming the diagnosis of MD.
FINAL DIAGNOSIS
The final diagnosis in this patient case was NASH with underlying MD.
TREATMENT
The patient is being treated with eicosapentaenoic acid (2700 mg/d) for dyslipidemia and is under calorie restriction by medical dieticians.
OUTCOME AND FOLLOW-UP
Since the diagnosis of MD, the patient has been followed for 14 years.His hepatosteatosis and mild elevation of serum aminotransferases have persisted, with no findings indicating liver cirrhosis or cancer.However, he has suffered from progressive muscle weakness and reduced physical activity.
DISCUSSION
MD is a relatively common myopathy with almost 100% penetrance that is estimated to afflict approximately 5-7 per 100000 persons worldwide[5].The condition is characterized by two different mutations: An expansion of CTG repeats in the 3’ untranslated region of the DMPK gene on chromosome 19 and an expansion of CCTG repeats in intron 1 on zinc finger protein 9 on chromosome 3, which are classified as MD type 1 and type 2, respectively.Southern blotting of the present patient led to the diagnosis of MD type 1.
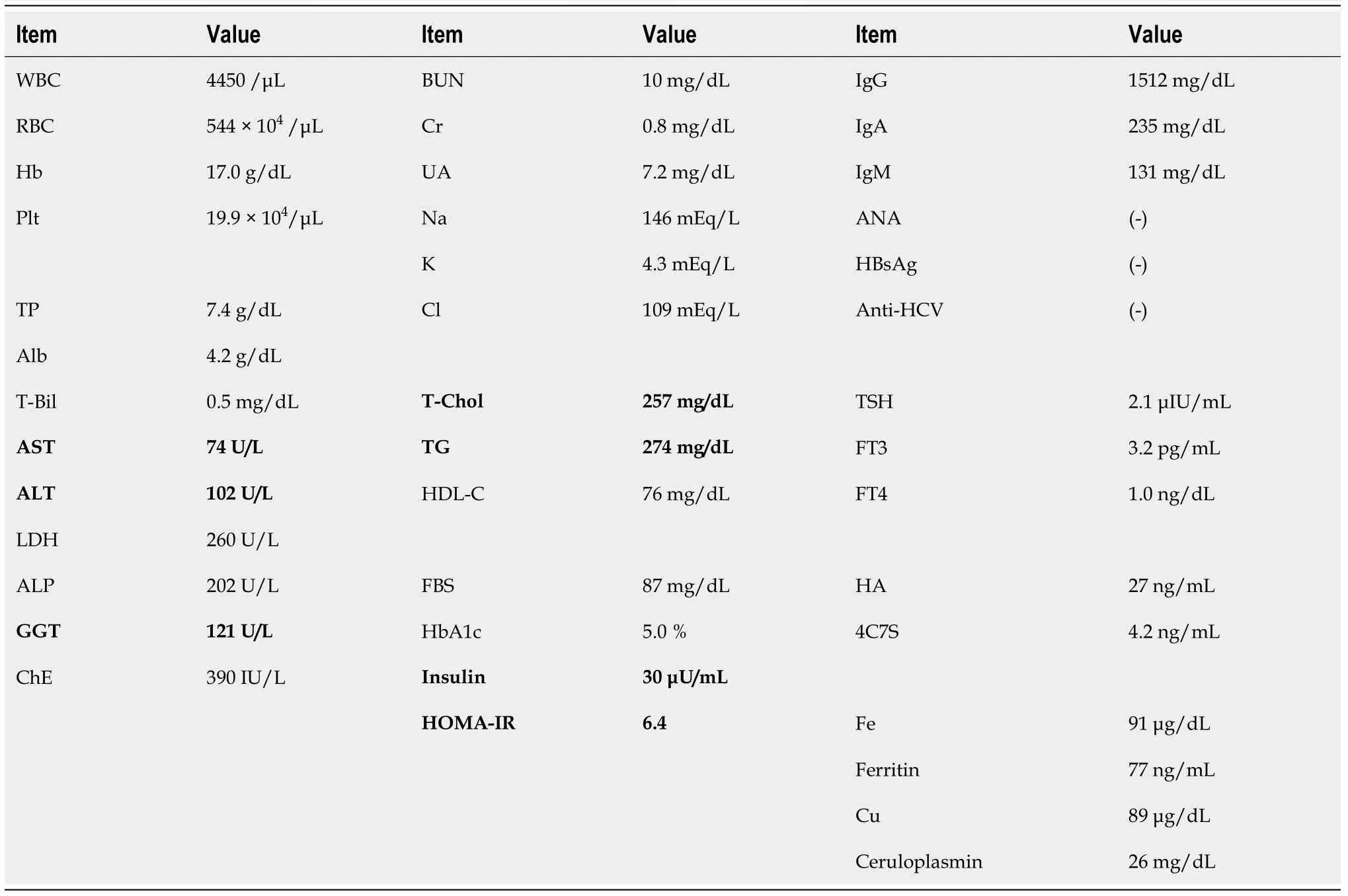
Table 1 Laboratory findings at the time of liver biopsy
MD is a multisystemic disease exhibiting diverse clinical manifestations, including muscle weakness, myotonia, early cataracts/baldness, arrhythmia, neuropsychiatric symptoms, and gonadal atrophy.The common features of MD type 1 are myotonia and insulin resistance, which are caused by aberrant splicing of chloride channel 1 and insulin receptor RNA in skeletal muscle due to the toxic effect of retained CUGexpanded repeats.Whole-body glucose disposal is reduced by 15%-25% after insulin infusion in MD type 1 patients, and insulin sensitivity, as well as insulin receptor RNA and protein, in the skeletal muscle is significantly decreased.Since peripheral insulin resistance is commonly observed in MD patients, metabolic disturbances, such as dyslipidemia, diabetes, and NAFLD/NASH may co-exist.
Indeed, it was reported that liver test abnormalities were frequent in MD patients[7-10].Shiehet al[11]prospectively evaluated the abnormalities in liver enzymes and metabolic parameters of 31 MD type 1 patients.The prevalence of diabetes, impaired fasting glucose, and metabolic syndrome (MetS) was approximately 12%, 21%, and 41%, respectively.Furthermore, 44% of MD patients had liver test abnormalities and 42% had NAFLD, as defined by abnormal liver chemistry tests and ultrasonography findings.
We reviewed the clinical data of 7 MD type 1 patients with NAFLD who underwent liver biopsy, including this case, and summarized the pathological features in Table 2[11-14].Ballooned hepatocytes were detected in 5 patients, who were all histologically diagnosed as having NASH.Our case did not receive a repeated liver biopsy.However, he did not show gradual decreases in platelet count or serum albumin, nor did he exhibit remarkable values for indicators of liver fibrosis progression or imaging findings suggestive of liver cirrhosis, such as splenomegaly, enlargement of the left lobe, or liver surface irregularity, during his 14-year follow-up.One report described a case of MD type 1 progressing to NASH-derived liver cirrhosis (Case #6 in Table 2)[14].Additionally, a case of MD type 2 manifested as myopathy, mild myotonia, cataract, diabetes, erectile dysfunction, gastrointestinal dysmotility, dysarthria, mild myocardial thickening and non-alcoholic and non-hepatitic liver cirrhosis was documented[15].Therefore, regular monitoring of laboratory indicators of liver synthesis ability (e.g., serum albumin and prothrombin time) and liver fibrosis (e.g., platelet count and serum type 4 collagen 7S) as well as liver imaging is advised for MD patients with NAFLD.In patients with cryptogenic non-alcoholic cirrhosis, the possibility of MD may be considered.

Table 2 Summary of previously reported liver pathology in 7 myotonic dystrophy type 1 patients with non-alcoholic fatty liver disease
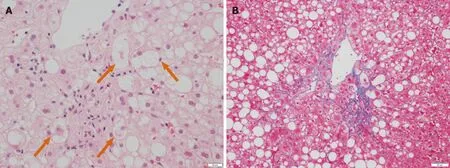
Figure 1 Pathological findings of liver biopsy.
Vujnicet al[16]examined the prevalence of MetS components in 66 MD type 1 patients and found dyslipidemia to be the most frequent [hypertriglyceridemia (67%) and low HDL cholesterol (35%)].On the other hand, the prevalence of hypertension, central obesity, and hyperglycemia was relatively low (18%, 13%, and 9%, respectively).This observation indicated that hypertriglyceridemia often co-existed in MD type 1 patients and that some MD patients with minimal-to-mild muscle symptoms might be mistaken as having hypertriglyceridemia and/or NAFLD.Insulin resistance enhances hepatic TG synthesis and the secretion of very-low-density lipoprotein particles, but reduces the activity of lipoprotein lipase, consequently leading to raised circulating TG levels.Fibrates are commonly available for treating hypertriglyceridemia, but myotoxicity and rhabdomyolysis are possible adverse effects.Before commencing fibrate administration for NAFLD/NASH patients with hypertriglyceridemia, serum CK levels should be checked to rule out the possibility of latent MD.

Figure 2 Photograph of the patient.

Figure 3 Southern blotting of patient DNA.
Recent studies documented the contribution of small intestinal bacterial overgrowth and disrupted bile acid metabolism to the pathogenesis of NAFLD/NASH[1,2,17,18].Tarnopolskyet al[19]documented that 65% of MD type 1 patients with gastrointestinal symptoms exhibited small intestinal bacterial overgrowth using glucose breath hydrogen testing.Additionally, it was reported that specific bile acids, such as dihydroxymono-oxocholanic acid and dihydroxycholanic acid, were detected in the serum of MD type 1 patients and biliary ursodeoxycholic acid was reduced[20], indicating bile acid abnormality accompanied by MD.Although the pathogenesis of NAFLD/NASH is multifactorial, these factors might be associated with NAFLD/NASH in MD.
CONCLUSION
MD is a relatively common congenital myopathy accompanied by peripheral insulin resistance.However, some MD patients with minimal-to-mild muscle symptoms might be followed as having other diseases associated with insulin resistance, such as hypertriglyceridemia, postprandial hyperglycemia, and NAFLD/NASH.In patients with abnormal liver function tests, muscular diseases might be hidden at all ages[21-24].When gastroenterologists encounter NAFLD/NASH patients, serum CK should be verified.If hyperCKemia is detected, the possibility of MD may be considered and careful observation of the patient’s face, and history taking for cataracts may help uncover subclinical MD.
ACKNOWLEDGEMENTS
We thank Mr.Trevor Ralph for his editorial assistance.
杂志排行
World Journal of Hepatology的其它文章
- Clinical implications, diagnosis, and management of diabetes in patients with chronic liver diseases
- Biomarkers for hepatocellular cancer
- Comprehensive review of hepatotoxicity associated with traditional Indian Ayurvedic herbs
- N-acetylcysteine and glycyrrhizin combination: Benefit outcome in a murine model of acetaminopheninduced liver failure
- Transaminitis is an indicator of mortality in patients with COVID-19: A retrospective cohort study
- Clinical efficacy of direct-acting antiviral therapy for recurrent hepatitis C virus infection after liver transplantation in patients with hepatocellular carcinoma