Postprandial dyslipidemia in insulin resistant states in adolescent populations
2020-11-11VictoriaHigginsKhosrowAdeli
Victoria Higgins, Khosrow Adeli,✉
1Molecular Medicine and Pediatric Laboratory Medicine, Research Institute, The Hospital for Sick Children, 2Department of Laboratory Medicine and Pathobiology, University of Toronto, Toronto, ON M5G 1X8,Canada.
Abstract Obesity and the metabolic syndrome are becoming increasingly prevalent not only in adults, but also in adolescents. The metabolic syndrome, a complex cluster of metabolic abnormalities, increases one's risk of developing type 2 diabetes and cardiovascular disease (CVD). Dyslipidemia, a key component of the metabolic syndrome, is highly associated with insulin resistance and contributes to increased CVD risk. Dyslipidemia has traditionally been assessed using a fasting lipid profile [i.e. fasting triglycerides, total cholesterol, low-density lipoprotein cholesterol (LDL-C), and high-density lipoprotein cholesterol (HDL-C)]. However, the postprandial state predominates over the course of a day and non-fasting triglycerides independently predict CVD risk. In insulin resistant states, the intestine overproduces triglyceride-rich lipoprotein (TRL) particles, termed chylomicrons (CMs), following ingestion of a fat-containing meal, as well as in the fasting state. Along with elevated hepatic TRLs (i.e. very-low density lipoproteins), CMs contribute to remnant lipoprotein accumulation,small dense LDL particles, and reduced HDL-C, which collectively increase CVD risk. Given the early genesis of atherosclerosis and physiological metabolic changes during adolescence, studying postprandial dyslipidemia in the adolescent population is an important area of study. Postprandial dyslipidemia in the pediatric population poses a significant public health concern, warranting a better understanding of its pathogenesis and association with insulin resistance and CVD. This review discusses the metabolic syndrome, focusing on the link between insulin resistance, postprandial dyslipidemia, and CVD risk. Furthermore, the clinical significance and functional assessment of postprandial dyslipidemia, specifically in the adolescent population, is discussed in more detail.
Keywords: dyslipidemias, insulin resistance, obesity, adolescent, apolipoprotein B-48, lipoproteins
Metabolic syndrome and its emergence in adolescence
Obesity and insulin resistance are highly associated with additional metabolic abnormalities, collectively termed the metabolic syndrome (MetS)[1]. Adults with the MetS have a fivefold greater risk of developing type 2 diabetes (T2D)[2], and are three times as likely to have[3]and more than twice as likely to die from[4]cardiovascular disease (CVD). In the late 1980s,Reaven described insulin resistance as the central pathophysiological feature of a cluster of metabolic abnormalities, denoting this phenomenon "Syndrome X"[5]. Several organizations have since proposed definitions for this syndrome, now termed the MetS,with the goal of reaching a consensus to improve its clinical assessment and diagnosis[6-10]. While specific cut-off values and emphasis of clinical features/components vary between definitions of the MetS,they all require a partial combination of central obesity, elevated triglycerides (TG), reduced highdensity lipoprotein cholesterol (HDL-C), glucose intolerance, and increased blood pressure. The most widely accepted definition, proposed by the International Diabetes Federation (IDF), bases the MetS diagnosis on the presence of central obesity(ethnic-specific waist circumference cut-offs) in addition to two of the following: increased TG (≥1.7 mmol/L), reduced HDL-C (<1.03 mmol/L for males;<1.29 mmol/L for females), increased fasting plasma glucose (≥5.6 mmol/L), and elevated blood pressure(≥130 mmHg systolic; ≥85 mmHg diastolic)[10].
Clustering of CVD risk factors is apparent not only in adults but also in pediatrics[11-13]. Obesity is associated with higher blood pressure, higher plasma glucose, and altered plasma lipids in adolescents[11].The prevalence of MetS in adolescents with obesity from the National Health and Nutrition Examination Survey (NHANES 1999-2002) varied from 12.4% to 44.2%, depending on the MetS definition used, which was higher than the prevalence of MetS in all adolescents (i.e. 2.0% to 9.4%)[13]. The presence of CVD risk factors in childhood and adolescence is becoming a major public health concern with the increased prevelance in pediatric obesity. The proportion of children and adolescents with overweight or obesity increased by 47.1% between 1980 and 2013 worldwide[14]. In the United States from 1999 to 2016, overweight and obesity prevalence in children and adolescents increased, with the highest prevalence (41.5%) observed in adolescents aged 16 to 19 years[15]. Defining the MetS in pediatrics is challenging due to the development of transient insulin resistance during puberty[16-17], variation in lipid levels with age and sex[18], and limited pediatric reference values for MetS components[19]. Similar to adults, several definitions have been proposed for the MetS in pediatrics[20-23], all requiring a combination of the same risk factor components. It is important to understand the pathophysiology of this complex cluster of metabolic abnormalities in adolescents due to its strong association with future morbidity and mortality. Approximately 85% of children with obesity become adults with obesity[24-25]and childhood obesity increases adulthood morbidity and mortality risk[24,26]. In the Princeton Lipid Research Clinics Follow-up Study from the US and Canada, the presence of the MetS in children and adolescents aged 6 to 19 years predicted clinical CVD in adults aged 30 to 48 years[27]. Importantly, dyslipidemia comprises two components of the MetS (i.e. high TG and low HDL-C), highlighting its strong association with T2D and CVD.
In this review, we discuss dyslipidemia in relation to insulin resistance and CVD risk, with a focus on the postprandial state (i.e. after a meal). We then focus on the adolescent population and discuss the clinical significance and assessment of dyslipidemia. Lastly,we review methodologies used in research settings to functionally assess postprandial lipid and lipoprotein dynamics in humans and their potential clinical applicability.
Postprandial lipid metabolism
Lipoprotein particles are primarily synthesized by the intestine or liver (Fig. 1). Dietary or exogenous lipis are digested and absorbed, aided by hepatic and pancreatic secretions including bile salts. Within the enterocyte, triglyceride-rich lipoprotein (TRL)particles, termed chylomicrons (CMs), are formed and secreted into lymphatic vessels and eventually the circulation. CMs are made continuously in the fasted and fed states and are comprised of both exogenous and endogenous lipids. CMs are characterized as large, spherical TRLs primarily comprised of TG and also containing phospholipids, cholesterol, and apolipoproteins (apos) (i.e. apoB48, apoAI, apoAIV,and apoCs)[28]. ApoB48 is more highly lipidated in the postprandial state, resulting in the secretion of larger particles despite only a relatively minor increase in particle number[29-30]. Nevertheless, CMs are constitutively produced even in the absence of dietary fat in the intestinal lumen, resulting in the production of smaller TG-poor CMs secreted in the fasting state[31]. A recent study that used mass spectrometric techniques and multicompartmental modelling estimated the production rate of basal apoB48 secretion in the fasting state to be approximately 53 mg/day[32]. Within the circulation, CMs are metabolized,releasing fatty acids (FAs), cholesterol, and other lipids for subsequent uptake by peripheral tissues. As CMs become TG-depleted, they form smaller, denser particles, termed CM remnants. CM remnants are then predominately taken up by the liver through apoE binding to hepatic LDL receptor and LDL receptorrelated protein 1[33]. The liver also produces TRL particles, termed very-low-density lipoproteins(VLDL), in which lipid is derived from either exogenous FAs, CM remnant uptake, orde novolipogenesis[34]. In the circulation, VLDL-TG is hydrolyzed by lipoprotein lipase (LPL) to yield intermediate-density lipoprotein (IDL) and eventually LDL particles, again delivering FAs, cholesterol, and other lipids to peripheral tissues. LDL is then taken up by peripheral tissues or the liver,viathe LDL receptor. Lastly, HDL formation begins with lipidpoor apoAI secretion from the intestine or liver,known as nascent HDL[35]. Nascent HDL subsequently acquires additional lipids by efflux from peripheral cells as well as transfer of lipids and apolipoproteins with TRLs (i.e.CMs and VLDL). HDL is thought to play a key role in reverse cholesterol transport, which promotes efflux of excess cholesterol from peripheral tissues for transport back to the liver.
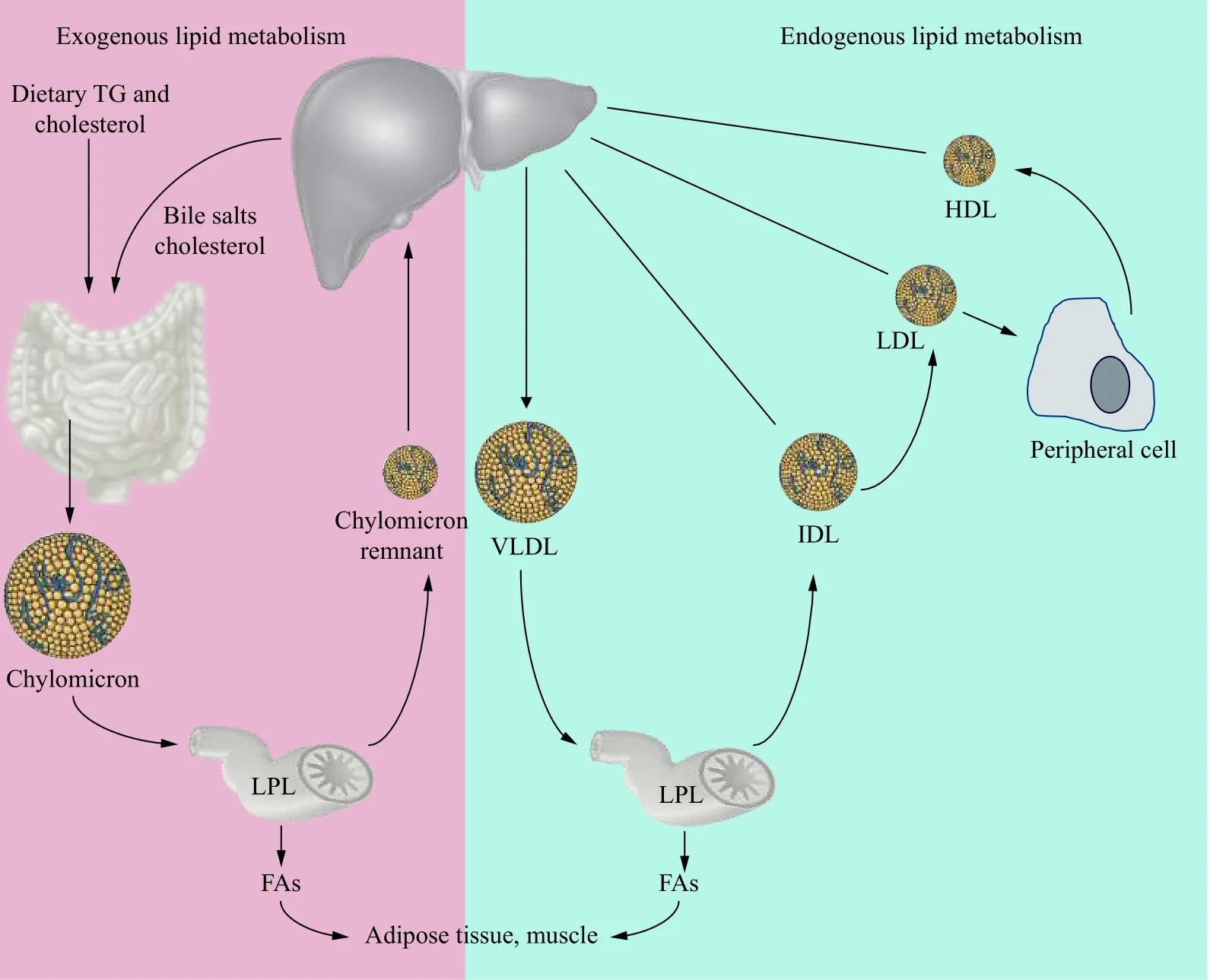
Fig. 1 Exogenous and endogenous lipid metabolism pathways. Digestion and absorption of dietary fat initiates the exogenous lipid metabolism pathway. Triglycerides (TG) and cholesterol are packaged within enterocytes to form chylomicrons (CMs), which eventually enter the circulation. In the circulation, lipoprotein lipase (LPL)-mediated hydrolysis liberates fatty acids (FAs) from CMs for uptake by peripheral tissues, forming smaller, denser CM remnants. CM remnants are then taken up by the liver via the low-density lipoprotein (LDL) receptor and LDL receptor-related protein 1. The endogenous lipid metabolism pathway begins in the liver with very-low-density lipoprotein (VLDL)synthesis and secretion. In the circulation, hydrolysis of VLDL-TG yields intermediate-density lipoprotein (IDL) and LDL particles. LDL is taken up by peripheral tissues or the liver via the LDL receptor. Lastly, HDL particles, synthesized by both the intestine and liver, play a key role in reverse cholesterol transport to promote efflux of excess cholesterol from peripheral tissues for transport back to the liver.
Postprandial dyslipidemia and cardiovascular disease risk
With current eating patterns in Western societies,the postprandial state predominates over the course of a day, with fasting status generally only achieved for a few hours in the early morning[36]. Nevertheless, lipids were primarily measured in the fasting state to reduce the variability in non-fasting TG measurements and to ensure low-density lipoprotein cholesterol (LDL-C) is accurately estimated using the Friedewald equation[37].However, non-fasting (i.e.random blood sample measurement irrespective of fasting duration) TG concentration fluctuates only modestly, with a maximal mean increase of 0.3 mmol/L 1-6 hours following a habitual meal[37]. Calculated LDL-C also minimally changes after food intake in those with and without T2D[38]and non-fasting LDL-C is predictive of CVD risk[39]. Non-fasting lipid assessment has several practical advantages, including improved patient compliance and follow-up, as well as reduced patient volume during early morning hours[37].Importantly, non-fasting TG strongly associates with CVD risk. Prospective studies show an association between non-fasting TG concentration and increased risk of coronary heart disease[40], ischemic stroke[41],myocardial infarction, ischemic heart disease, and death[42-43]. Postprandial CM remnants correlate with 5-year progression of coronary atherosclerosis in postinfarction patients[44]and postprandial remnant cholesterol is higher in patients with coronary artery disease compared to that in controls, despite a similar fasting lipid profile[45]. Non-fasting lipid measurements may even be superior to fasting measurements regarding CVD risk prediction. An 11.4-year follow-up study in women found that postprandial, but not fasting, TG levels independently associate with incident CVD events[46]. Furthermore,postprandial remnant cholesterol was more strongly associated with carotid intima-media thickness (cIMT)than fasting remnant cholesterol in healthy middleaged men[47]. Therefore, clinical CVD risk assessment guidelines from several national organizations now include the option of non-fasting lipid measurements[37-38,48-50].
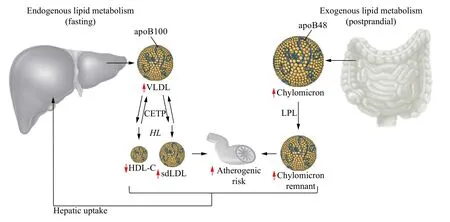
Fig. 2 Diabetic dyslipidemia. Disorders of both endogenous hepatic lipid metabolism and exogenous intestinal lipid metabolism contribute to diabetic dyslipidemia. In the fasting state, apoB100-containing very-low density lipoprotein (VLDL) particles are overproduced from the liver. VLDL accumulation, as well as cholesterol ester transfer protein (CETP) and hepatic lipase (HL) activity contribute to the formation of small dense low-density lipoprotein (sdLDL) particles and reduced high-density lipoprotein cholesterol (HDL-C). In the postprandial state, apoB48-containing chylomicrons are overproduced, contributing to an accumulation of chylomicron remnants through the action of lipoprotein lipase (LPL). Both sdLDL and chylomicron remnants can enter the arterial wall and contribute to risk of atherosclerosis. Modified from Adeli et al[51].
Lipid and lipoprotein abnormalities are commonly observed in insulin resistant states, termed "diabetic dyslipidemia" (Fig. 2). Diabetic dyslipidemia is primarily comprised of hypertriglyceridemia, low HDL-C, and a shift towards small dense LDL(sdLDL) particles[51]. These features are primarily driven by TRL accumulation, including hepatic VLDL, primarily in the fasting state, and intestinal CM, primarily in the postprandial state. The postprandial increase in TRL-TG is predominantly due to an increase in apoB48-containing TRLs (i.e.CMs) transporting dietary lipid[52]. A recent study using non-steady-state multicompartmental modelling to characterize lipoprotein kinetics similarly confirmed a greater postprandial TG flux in the CM than VLDL fraction. However, due to their baseline secretion in the fasting state, VLDL particles remain the major carriers of plasma TG during the postprandial period[52]. VLDL particles also increase slightly postprandially, due to competition with CMs for lipolysis and clearance[53-54]. Accumulation of TRLs in the postprandial state drive further lipoprotein abnormalities, including an accumulation of atherogenic TRL remnants. The now widely reported finding that CM remnants penetrate and are retained by the subendothelial space[55-58]suggests a role of remnant accumulation in CVD risk. This is further supported by predisposition of patients with type Ⅲ hyperlipoproteinemia, a genetic disorder characterized by remnant particle accumulation due to impaired clearance, to premature atherosclerosis and CVD risk[59]. Fully hydrolyzed CM remnants contain approximately 40 times more cholesterol per particle than LDL particles[60-61]and may be preferentially retained relative to other lipoproteins[57,62]. Remnants increase endothelial permeability, leading to increased diffusion of remnants and LDL particles into the subendothelial spaceviaparacellular transport[63].Within the arterial wall, remnants induce atherosclerotic lesion development[62,64]viaseveral mechanisms including increasing monocyte adhesion to endothelial cells[65]and monocyte migration into the sub-endothelial spaceviaupregulation of monocyte chemoattractant protein-1 expression[66-67]. Thus,remnants induce several critical steps of atherosclerosis progression. TRL accumulation also leads to TG enrichment of HDL, promoting HDL clearance[68]and formation of atherogenic sdLDL[69].

Fig. 3 Chylomicron synthesis and secretion. Inside the enterocyte, dietary fatty acids (FAs) are transported to the endoplasmic reticulum(ER) via intestinal and liver FA-binding proteins (IFABP and L-FABP, respectively). FA is then rapidly converted to triglycerides (TG) at the ER membrane by the subsequent actions of monoacylglycerol acyltransferase (MGAT) and diacylglycerol acyltransferase (DGAT).Niemann-Pick C1-like 1 protein (NPC1L1) aids in cholesterol absorption and trafficking to the ER. Free cholesterol is then esterified at the ER to cholesteryl ester (CE) by membrane-bound acyl-CoA:cholesterol acyltransferase 2 (ACAT2). Chylomicron particle formation begins with the translocation of apoB48 across the ER membrane. Microsomal triglyceride transfer protein (MTP) transfers lipids to nascent apoB48 to form a prechylomicron particle. Lipid droplets (LD) within the ER lumen merge with the prechylomicron particle in a process termed "core expansion", with subsequent addition of apoAIV. Prechylomicron particles bud from the ER, traverse the cytosol in prechylomicron transport vesicles (PCTVs), and fuse with the Golgi membrane. Mature CMs are then transported from the Golgi to the basolateral membrane via transport vesicles and are subsequently exocytosed into the lamina propria and eventually enter the blood circulation.Adapted from Adeli et al[51].
Postprandial dyslipidemia in insulin resistant states and prediabetes
Postprandial dyslipidemia associated with insulin reisstance has been previously reviewed[70]and is described briefly here. TRL accumulation in the postprandial state is a common feature of insulin resistance[71-72]. Most investigations examining the link between insulin resistance and impaired postprandial lipid metabolism initially focused on delayed CM clearance as a contributor to postprandial CM accumulation. Delayed postprandial TRL clearance has been observed in subjects with obesity,insulin resistance, metabolic syndrome and T2D[73-76],which may result from reduced LDL receptor expression[73,77]and/or increased apoC-Ⅲ[75], and interferes with LPL activity[78-79]. Intestinal overproduction of CMs, the normal process of which is summarized inFig. 3, may also contribute to TRL accumulation in the fasted and postprandial state, as described below.Ex vivostudies of enterocytes have shown oversecretion of apoB48-containing lipoproteins with fructose feeding[80]. Postprandial CM overproduction has also been confirmed in the insulin resistant fructose-fed hamster model[80-81], the JCR:LA-cp rat model of insulin resistance and obesity[64,82-83], and the Psammomys obesus rat model of insulin resistance and T2D[84]. Postprandial CM overproduction was also confirmed in humans with insulin resistance[76]and T2D[74,85]. In vivo investigation of insulin resistant, fructose-fed hamsters demonstrated unresponsiveness to insulin-induced inhibition of CM production, in contrast to that of chow-fed controls[86], suggesting insulin resistance can occur at the level of the enterocyte. This was further confirmed in humans, in which T2D patients likewise exhibited a blunted response to the inhibitory action of insulin on CM production[87].
TG synthesis within the small intestine is increased in insulin-deficient diabetic rats, concurrent with enhanced TG transport[88], suggesting increased de novo lipogenesis (DNL) within the enterocyte may partially contribute to increased CM particle number and TG content in insulin resistance states.Furthermore, enterocytes are capable of utilizing glucose for TG synthesis[89], supporting the observed upregulation of intestinal TG synthesis in patients with T2D. Altered enterocyte machinery for de novo lipogenesis and CM assembly also lead to intestinal CM overproduction and ultimately postprandial hypertriglyceridemia. In insulin resistant states,monoacylglycerol transferase 2 (MGAT2) and diacylglycerol acyltransferase 1 (DGAT1) expression and activity are increased[84,90]alongside enhanced DNL and enterocyte lipid content, potentially explaining the observed elevation in apoB48 stability and reduced proteasomal degradation[81,84].Furthermore, L-FABP has been reported to be increased in Psammomys obesus rats[84], suggesting enhanced FA trafficking to the ER for TG synthesis and incorporation into CMs. While microsomal triglyceride transfer protein (MTP) activity and protein expression were not altered in the Psammomys obesus rat[84], elevated MTP mass[80-81]and activity[80]were elevated in fructose-fed hamsters. Plasma free FAs (FFAs) are often increased in individuals with insulin resistance and/or T2D[91]. Increased FFA in insulin resistant states[91]combined with the ability of circulating FFA to promote CM output suggests another potential mechanism of CM overproduction in insulin resistance[92-93]. The ability of FFAs to promote CM output may be the result of direct incorporation into secreted CMs or via promoting mobilization of stored TG[94-95].
Clinical significance of pediatric dyslipidemia
There are several established risk factors for CVD,including family history of CVD, physical inactivity,tobacco exposure, elevated blood pressure,overweight/obesity, dyslipidemia, and T2D[49]. With the increased prevalence of pediatric obesity, several CVD risk factors, including dyslipidemia, are increasingly prevalent early in life. In a study of 823 children and adolescents with obesity recruited from Ankara Children's Hematology-Oncology Training and Research Hospital in Turkey, 42.9% exhibited fasting dyslipidemia (i.e. defined as having either elevated total cholesterol, TG, or LDL-C, or reduced HDL-C levels)[96]. Dyslipidemia detected in childhood or adolescence strongly tracks into adulthood[97-99]. For example, a 27-year follow-up study of 2204 subjects from the Cardiovascular Risk in Young Finns Study showed fasting serum lipid levels strongly track from early life to adulthood, particularly for adolescents aged 12-18 years[97]. Early detection of dyslipidemia is also important because atherosclerosis originates in childhood and CVD risk factors early in life strongly associate with atherosclerosis. Two main studies showed this link through assessing the relationship between risk factors and atherosclerosis measured by autopsy of the aorta and coronary arteries in children,adolescents, and young adults who died of accidental causes[100-101]. In the Bogalusa Heart Study[100], the presence, number, and intensity of CVD risk factors were significantly related to the extent and severity of atherosclerosis in the aorta and coronary arteries measured at autopsy (i.e. fatty streaks and fibrous plaques) in subjects aged 2 -39 years. Non-invasive measures, including cIMT, are more commonly used to assess atherosclerotic plaque development, and have been shown to associate with dyslipidemia in childhood and adolescence[102-104]. The National Heart,Lung, and Blood Institute (NHLBI) guidelines report that identifying and managing dyslipidemia in youth,as well as throughout adulthood will reduce CVD risk,including subclinical evidence of atherosclerosis[48].
Dyslipidemia assessment in adolescents
In 2016, the Canadian Cardiovascular Society released updated guidelines for the management of dyslipidemia for the prevention of CVD in adults[49].However no guidelines have been currently proposed for managing dyslipidemia in pediatrics by Canadian societies. The NHLBI in the United States published updated Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents[48], which are widely used in Canada for the management of dyslipidemia in pediatric patients.The dyslipidemic pattern observed in childhood and adolescence is primarily comprised of moderately to severely elevated TG, normal to moderately elevated LDL-C, and reduced HDL-C[48]. The NHLBI guidelines provide acceptable, borderline-high, and high values for total cholesterol, LDL-C, non-HDL-C,apoB, and TG, as well as acceptable, borderline-low,and low values for HDL-C and apoAI[48].Recommendations include that lipid assessment should be based on the average of at least two lipid profiles obtained between 2 weeks and 3 months apart. First line management of children and adolescents with dyslipidemia is focused on lifestyle modification, including diet and physical activity.Specific algorithms to guide recommendations on initiating medication therapy are based on elevated LDL-C and/or elevated TG and are generally applicable only for children ≥10 years of age.Initiation of statin therapy is recommended for patients with (1) LDL-C≥4.90 mmol/L, (2) LDL-C 4.20-4.90 mmol/L with either a positive family history of premature CVD in a first-degree relative, 1 highlevel risk factor, or 2 moderate-level risk factors,or (3) LDL-C 3.40 -4.20 mmol/L with either clinical CVD, 2 high-level risk factors or 1 high-level risk factor and 2 or more moderate-level risk factors. For patients with TG≥2.25 mmol/L, omega-3 fish-oil therapy should be considered or a lipid specialist should be consulted to initiate statin treatment if non-HDL-C is also ≥3.80 mmol/L. Overall, the goal of assessing dyslipidemia and other CVD risk factors early in life is to prevent additional CVD risk factor development and to identify and manage children and adolescents with CVD risk factors who are consequently at increased risk of an ischemic CVD event later in life.
While fasting lipid assessment is traditionally performed by quantifying the total circulating lipid content (i.e. triglyceride and cholesterol) and cholesterol content of LDL, HDL, and/or non-HDL particles, lipoprotein particle number and/or size may be of greater clinical utility. For example, fasting LDL particle number (LDL-P) associated more strongly than LDL-C with atherosclerotic risk[105-107]. In pediatrics with discordant LDL-P and LDL-C, it also associated more strongly with body mass index and homeostatic model assessment of insulin resistance[108].Although density gradient ultracentrifugation is considered the "gold-standard" for lipoprotein fractionation[109], its wide-spread clinical adoption is limited due to its labor-intensive and time-consuming protocol, including additional enzymatic assays to quantify lipoprotein composition (i.e. cholesterol and TG content). Furthermore, classifying lipoproteins using density-based methods inherently results in heterogeneous categories comprised of lipoproteins differing in diameter, composition, and potentially atherogenicity[110-111]. Nuclear magnetic resonance(NMR) spectroscopy provides an alternative method that can simultaneously quantify the number and size of several lipoprotein subclasses[112]. Several studies in adolescents have shown an association of adiposity and insulin resistance with an atherogenic lipoprotein profile, as measured by NMR spectroscopy, including increased concentration of small LDL-P and large VLDL particle number (VLDL-P), decreased concentration of large LDL-P and large HDL particle number (HDL-P), as well as decreased LDL-P size and HDL-P size[111,113-117]. More insulin resistant adolescents, defined by hyperinsulinemic-euglycemic clamp, exhibited a higher concentration of small LDLP, small HDL-P, and large TRL particle number(TRL-P), as well as smaller average LDL-P and HDLP size[115]. Furthermore, waist circumference (WC)positively correlated with fasting large, but not small,TRL-P[113]. Relative weight reduction over a 2.5 year period was associated with favorable changes in TRLP, LDL-P, and HDL-P sizes, as well as LDL-P concentration[118], suggesting adiposity plays a causative role in a dyslipidemic lipoprotein phenotype profile. One study assessed the association of adiponectin with NMR lipid parameters and found that adiponectin positively associated with LDL-P and HDL-P size and negatively associated with small LDL-P and HDL-P, suggesting this adipokine may play a role in the effect of adiposity on the dyslipidemic phenotype[119]. However, adiponectin did not significantly associate with the concentration of large VLDL-P, which includes chylomicron-sized particles. Importantly, NMR lipid parameters were stronger independent predictors of vascular damage than traditional fasting lipid parameters in adolescents[120-121]. However, no studies to-date have comprehensively characterized the lipid and lipoprotein phenotype profile in adolescents in the postprandial state, despite the well-recognized association between postprandial lipemia and CVD risk[46].
Functional assessment of postprandial dyslipidemia
Oral fat tolerance test methodology
In the research setting, an oral fat tolerance test(OFTT) can be used to functionally assess postprandial lipid dynamics. Lipid and lipoprotein assessment using the OFTT allows the determination of early impairements in postprandial lipid metabolism that can not otherwise be detected in the fasted state[122]. The mechanism underlying this method is similar to that of the oral glucose tolerance test (OGTT), which evaluates glucose metabolism following an oral glucose load to diagnose impaired glucose tolerance or T2D[123-124]. The OFTT involves ingesting a high-fat meal, followed by blood sampling at specified time points to measure lipid parameters,most commonly TG. This procedure provides an indication of an individual's capacity to metabolize lipids in the postprandial state from digestion and absorption of lipids through secretion and clearance of lipoproteins. However, the OFTT is not commonly used clinically, partly due to a lack of standardized test procedures and cut-off TG values, as well as the inconvenience of the test. Methodologies vary widely in pre-test meal conditions (e.g. kind of meal ingested and exercise the day before the OFTT), volume of meal, ingredients, energy macronutrient composition(i.e. fat, carbohydrate, protein), and frequency of the test meal, as well as postprandial blood collection time points[125]. Variation also exists in the analysis and interpretation of data collected from an OFTT.Calculating the overall variation in a parameter following an OFTT can be done by calculating the area under the curve (AUC), generally by the trapezoidal method[125]. Incremental concentrations[e.g. incremental area under the curve (iAUC)] can be obtained by substracting baseline from postprandial values[125]. The iAUC provides a representation of the relative change from baseline in the postprandial state and normalizes baseline values which can vary between subjects[125]. Efforts towards OFTT methodology standardization have been made in the adult population based on a meta-analysis of 113 studies[126-127]. The recommendations suggest that an OFTT should consist of a single fat load after a minimum 8 hours fast that is comprised of 75 g of fat,25 g of carbohydrates, and 10 g of protein[127].
Clinical utility of oral fat tolerance tests
The diagnostic value of clinically performing an OFTT has yet to reach consensus. In subjects without T2D, the postprandial plasma TG excursion following an OFTT has been shown to be predictive of coronary artery disease[128-131]. Similarly, a case-control study showed that the presence of atherosclerosis, as defined by cIMT, was associated with a greater postprandial TG response following an OFTT in lean, healthy subjects, even after adjusting for fasting TG[132].However, the association between CVD risk and TG levels following an OFTT in patients with T2D remains controversial. Among 60 patients with T2D,cIMT was elevated in those with postprandial hypertriglyceridemia (TG >2.27 mmol/L 4 hours after a mixed meal), despite normal fasting TG levels[133]and participants with T2D and a history of a myocardial infarction had higher postprandial TG than individuals with T2D but without a history of a myocardial infarction[134]. Conversely, other studies reported no association between postprandial TG levels and coronary artery disease in patients with T2D[135-136]. For example, a case-control study of 164 patients with T2D found that TG levels after consumption of a high-fat beverage were not associated with the presence of coronary artery disease[136]. Overall, these observations suggest that the OFTT may be more clinically useful for CVD risk assessment in patients without T2D. However, it is important to note that findings from OFTT studies can be confounded by the type of meal used,macronutrient population, as well as population studied (e.g. the varied extent of additional metabolic abnormalities in subjects with T2D).
The clinical utility of the OFTT also appears to be dependent on the fasting TG concentration, with higher utility for intermediate fasting TG levels. The same meta-analysis of 113 studies described above[126]found that the TG response to an OFTT was highly variable across fasting TG levels (1 -2 mmol/L).However, the OFTT provided little additional information for individuals with fasting TG levels<1 mmol/L or >2 mmol/L, as fasting TG was highly predictive of postprandial TG in these instances.Therefore, Kolovou et al recommended that the OFTT may only be clinically useful for subjects with fasting TG levels between 1 mmol/L and 2 mmol/L (normal fasting TG levels are <1.7 mmol/L) and should not be performed in subjects not meeting this criteria[127].Furthermore, in a case-control study of 770 subjects,TG levels following an OFTT were significantly elevated in those with paternal history of coronary artery disease compared to those without, although this was only observed in subjects with moderately high fasting TG levels[137]. Overall, postprandial TG may provide a better indication of CVD risk than fasting TG levels in those with more moderate metabolic abnormalities (i.e. no T2D, moderate elevation in fasting TG levels). Those with no metabolic abnormalities are unlikely to have abnormal postprandial TG levels and postprandial TG levels may not provide clinically useful information for patients with T2D and/or very high fasting TG levels.It is also important to note that while the OFTT may aid in identifying early postprandial dyslipidemia,particularly altered TRL metabolism, and assessing CVD risk, it would not be of clinical use to detect lipid disorders that cause extreme TG elevations that contribute to pancreatitis[138]. The OFTT is also limited by the inconvenience of fasting, consuming a test meal, and waiting 6 -8 hours for multiple blood collections. However, it has been recommended that a single TG measurement 4 hours after the OFTT meal be used for clinical purposes[127], as this measurement has shown to best represent the postprandial lipemia response[42,126,139]. While the clinical utility of the OFTT warrants further investigation to determine if and how results can inform patient management, its use in a research setting provides value, including assessing postprandial markers beyond TG and delineating the pathology of postprandial metabolic abnormalities.
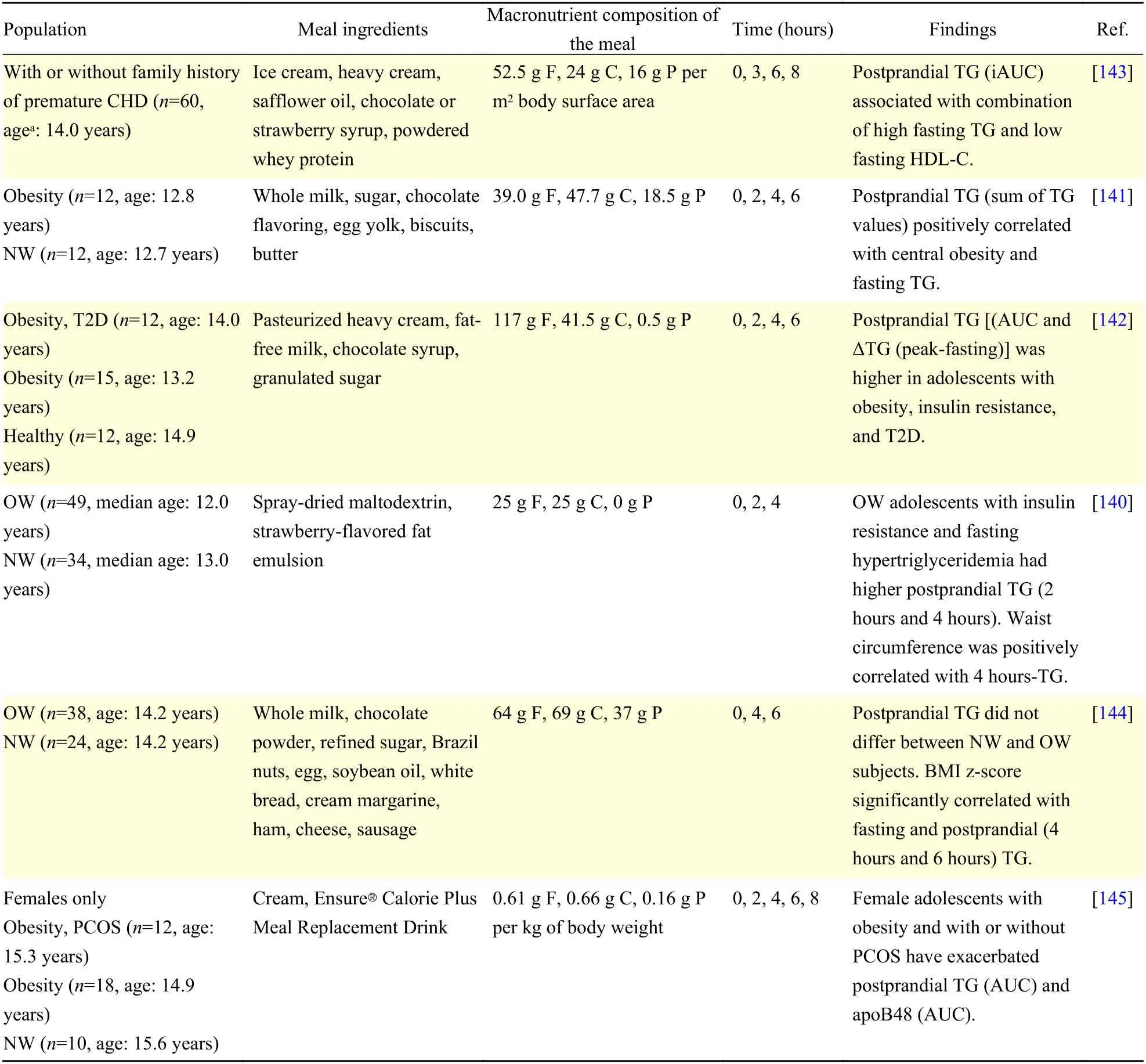
Table 1 Studies assessing postprandial lipemia in adolescents with obesity and/or associated co-morbidities
No recommendations for evaluating postprandial lipemia in the pediatric population have yet been provided[127], due to the sparsity of studies performing such assessments. Few studies have assessed postprandial lipids and lipoproteins in adolescents(Table 1). In these studies, postprandial TG concentration was significantly higher in adolescents with central, rather than peripheral, obesity[140-141]and insulin resistance was a major determinant in postprandial TG elevation[142]. These findings suggest postprandial TG is a major metabolic abnormality associated with adiposity and insulin resistance in adolescents. Vine et al reported higher postprandial TG and apoB48 in adolescent females with obesity than in controls with normal weight[145]and these levels significantly associated with both adiposity and insulin resistance[145]. Thus, accumulation of intestinally-derived CMs in adolescents is associated with obese and insulin resistant states. Nevertheless,most studies in adolescents to-date have primarily assessed TG, which overlooks the great variation in lipoprotein composition, size, number, and associated atherogenic potential. Furthermore, studies in adolescents are warranted to consider the physiological insulin resistant state in puberty, as well as the association with androgens and estrogens.Therefore, it is of interest for future studies to provide a comprehensive assessment of the postprandial lipid and lipoprotein phenotype in adolescents with obesity and insulin resistance.
Concluding remarks
The MetS, a cluster of metabolic risk factors that increases one's risk of developing T2D and CVD, is becoming increasingly prevalent not only in adults,but also in adolescents. One key component of the metabolic syndrome is lipid/lipoprotein abnormalities,termed diabetic dyslipidemia. While traditionally measured in the fasting state, dyslipidemia measured postprandially is now recognized as an equivalent or superior predictor of CVD risk to fasting measurements. In this review, we discussed the development of postprandial dyslipidemia in insulin resistant states and its association with elevated CVD risk. We also described the assessment of lipid and lipoprotein dynamics in both clinical and research settings, with a focus on the adolescent population.Overall, the growing rates of metabolic dysfunction in younger populations is posing a significant public health risk and warrants further research to better understand its development, progression, and associated risk profile.
杂志排行
THE JOURNAL OF BIOMEDICAL RESEARCH的其它文章
- Pre-evaluation of humoral immune response of Bactrian camels by the quantification of Th2 cytokines using real-time PCR
- Comparison of the modified Wiltse's approach with spinal minimally invasive system and traditional approach for the therapy of thoracolumbar fracture
- Exposure to environmental bisphenol A inhibits HTR-8/SVneo cell migration and invasion
- Cumulative live birth rates of in vitro fertilization/intracytoplasmic sperm injection after multiple complete cycles in China
- Cofilin participates in regulating alpha-epithelial sodium channel by interaction with 14-3-3 isoforms
- TIR/BB-loop mimetic AS-1 protects vascular endothelial cells from injury induced by hypoxia/reoxygenation
