Venous resection at pancreaticoduodenectomy can be safely performed in the presence of jaundice
2020-10-23RuplyPndeJmesHodsonRviMrudnygmDriusMirzJohnIscKeithRoerts
Ruply Pnde , Jmes Hodson , Rvi Mrudnygm , Drius Mirz , John Isc ,Keith J Roerts , c , ∗
a HPB Surgery, University Hospitals Birmingham NHS Foundation Trust, Birmingham B15 2TH, UK
b Institute of Translational Medicine, University Hospitals Birmingham NHS Foundation Trust, Birmingham B15 2TH, UK
c Institute of Immunology and Immunotherapy, University of Birmingham, Birmingham B15 2TH, UK
Venous resection at pancreaticoduodenectomy (PD) has established itself as a viable treatment for borderline resectable cancer, with equivalent survival to those patients undergoing PD for cancer without venous resection [1].Thus surgery for these patients is clearly desirable, when possible, compared to palliative care.However, there is concern and debate about the safety of venous resection at PD [2].There is a need to improve patient pathways, outcome and experience [3].To this end, in patients who present with jaundice, it is clear that surgery without preoperative biliary drainage (PBD) reduces complications [4].In 2015, our team introduced a ‘fast track’ program to routinely perform PD in the presence of jaundice [5].This change of practice has become routine, with most patients now undergoing surgery without PBD.It is, however, unclear whether portal vein (PV) resection + PD is safe in the setting of jaundice.The aim of this study, therefore, was to compare outcomes and complications between patients with or without jaundice undergoing PD with associated resection of the superior mesenteric vein (SMV) and/or PV.
Consecutive patients undergoing PD plus SMV/PV resection for suspected pancreatic ductal adenocarcinoma between the 1st January 2011 and 1st September 2018 at our center were identified from our institutional database.Complications and outcomes were observed prospectively, and recorded by a dedicated data manager.This study was approved by the Ethics Committee of our hospital.In 2015 the ‘fast track’ program was introduced to routinely perform PD among patients with jaundice; our preoperative pathways and experiences are described elsewhere [5].Venous involvement is not considered a contraindication for surgery if surgical resection and reconstruction of the vein are considered technically achievable.The initial threshold of total bilirubin for surgery was 300 μmol/L, but this increased over time in a stepwise fashion, and is now 500 μmol/L.The preference of the team is to perform an end-to-end resection with primary anastomosis.Wedge resections or patches are used when an area of tumor contact is small.Packs are put behind the liver and, if needed, a Cattell Braasch maneuver is performed to mobilise the small bowel, to reduce the gap in the vein.If the gap is too wide for primary closure, the team prefers to use cadaveric iliac vein graft, matched for blood group with the recipient.Patients receive prophylactic low-molecular-weight heparin following surgery to the point of discharge.If any issues with the vein patency are identified, this would require a change to treatment dose of low-molecular-weight heparin or warfarinisation.Following surgery, PV patency is assessed using ultrasound prior to discharge, or other managements as needed if the patient is unwell.
Comparisons of demographics and outcomes by jaundice status were performed using Fisher’s exact tests for nominal variables, and Mann-WhitneyUtests for continuous or ordinal variables.Time-to-event outcomes were compared between groups using Cox regression models, and visualised using Kaplan-Meier curves.Analyses of blood markers were performed using a generalized estimating equation approach, in order to account for correlations between repeated measures on the same patient.The postoperative day (POD) of the blood measurement was set as the withinsubject factor, and an autoregressive correlation structure was assumed.The jaundice status, POD of the blood measurement and an interaction term between these were entered as factors into each model.Total bilirubin, creatinine and C-reactive protein levels were all found to be skewed, and so were log10-transformed, prior to analysis, in order to normalize the distribution.The distribution of glomerular filtration rate (GFR) had a preponderance of patients with values at the upper limit of detection of 90 + mL/min/1.73 m2,hence the data were dichotomized using this as a cut-offvalue.APvalue<0.05 was considered statistically significant.
Over the period, 89 (27%) of 328 and 11 (16%) of 67 patients with pancreatic adenocarcinoma and cholangiocarcinoma, respectively, had an associated venous resection.Of these, 36/100 had jaundice at surgery (median total bilirubin: 277 μmol/L, range 45-613).Seventy-five veins were closed with primary closure (wedge resectionn= 14, end-to-end closuren= 61) and 25 required a vein graft (patchn= 4, interposition graftn= 21).Two patients had the jejunal branch of the SMV tied offand the ileal branch reconstructed to the main SMV with interposition vein graft.
There were no significant differences in patient demographics and the approaches to surgery between patients with and withoutjaundice.However, patients with jaundice were significantly more likely to have borderline resectable disease, and significantly less likely to receive neoadjuvant chemotherapy ( Table 1 ).
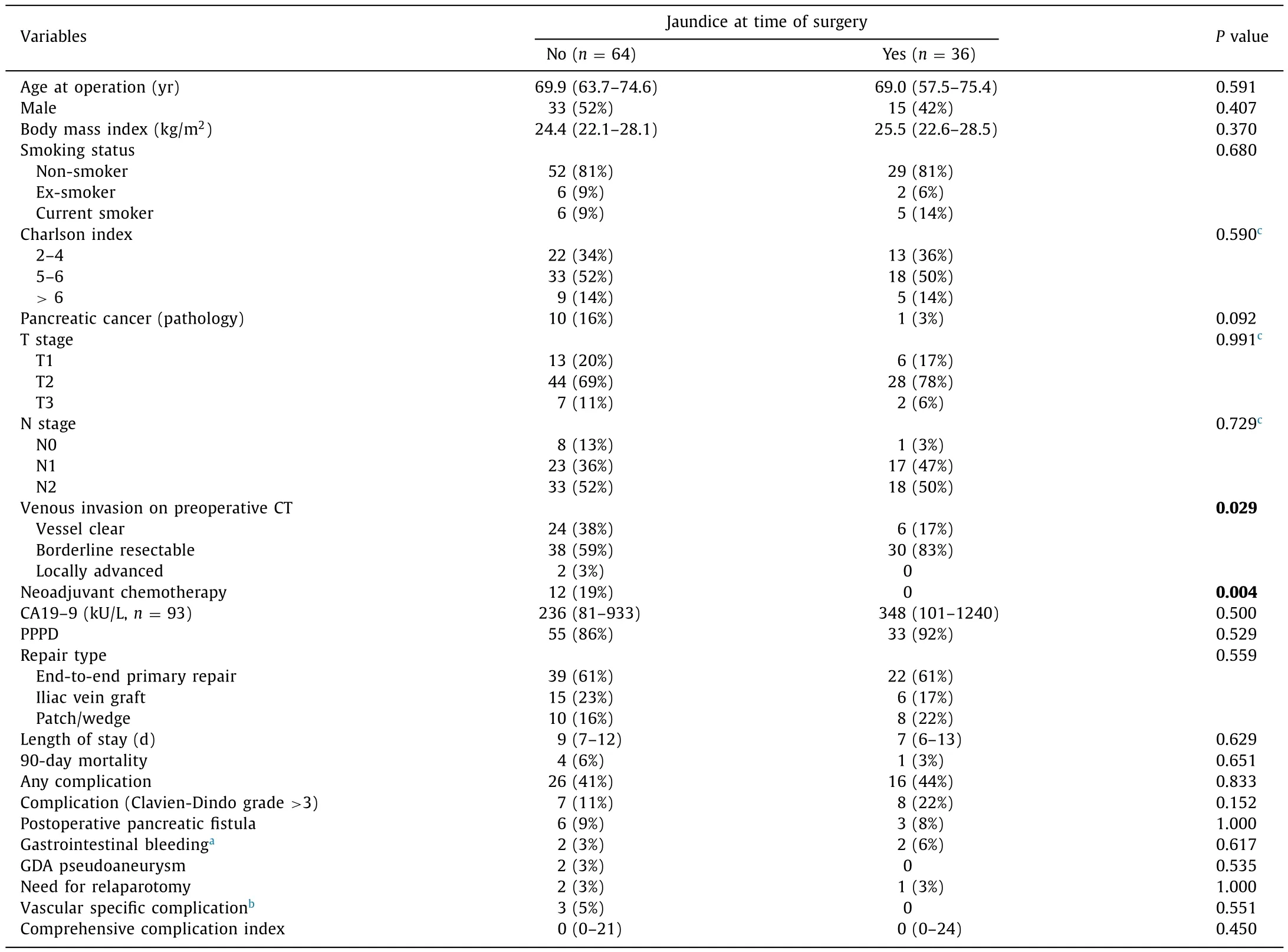
Table 1Demographics and outcomes by jaundice status.
Analyses of the changes in blood markers following surgery are reported in Fig.1.Total bilirubin levels were found to drop rapidly following surgery, with a significantly larger decline observed among jaundiced patients, with a reduction of 60% (geometric mean: 144 to 58μmol/L) from PODs 1-7, compared to 36% (14 to 9μmol/L) in patients without jaundice (P<0.001).Creatinine levels also declined significantly across the postoperative period (P<0.001) with no significant difference detected between patients with and without jaundice (P= 0.832).C-reactive protein increased postoperatively, peaking on POD 2 before declining; levels were consistently lower in the jaundiced cohort(P= 0.006).Postoperative outcomes, including length of stay, complication rates, specifically both post-pancreatectomy hemorrhage and postoperative pancreatic fistula, and 90-day mortality were found to be similar in patients with and without jaundice ( Table 1 ).Over a median follow-up time of 13 months, no significant difference in long-term postoperative survival was detected between the groups, with a hazard ratio of 0.94 (95% CI: 0.53-1.67,P= 0.825)for patients with jaundice, relative to the no jaundice group (median survival: 20 vs.18 months).Of the five patients who died within 90 days of surgery, two had complications related to the venous anastomosis (both in the no jaundice group).Of these,one patient required laparotomy on POD 1 for thrombosis of the SMV after an end-to-end primary anastomosis.A venous interposition graft was placed after thrombectomy.This patient developed a grade C postoperative pancreatic fistula and died of sepsis and multi-organ failure on POD 27.The other patient was admitted at POD 84 with weight loss, deterioration and ascites.There was PV occlusion on CT scan and cancer recurrence was suspected.This patient died 88 days after surgery.
Mesenteric/portal vein occlusion occurred in 13 patients.Nine resulted from cancer recurrence, with two of the remainder being those described above, and the other two occlusions being largely asymptomatic, requiring no intervention.Rates of vein occlusion were similar in patients with and without jaundice (4% vs.11% at 1 year) ( Fig.2 ).
The main finding of this study is that venous resection in patients with jaundice is as safe and with a similar complication profile as those without jaundice.This is an important finding,given the need to improve survival among patients with pancreatic cancer, where resection of patients with vascular involvement increases the proportion of patients undergoing attempts to achieve cure [3].This may also lead to improved patient experience [6]where avoidance of PBD avoids the associated discomfort of the procedure, as well as reducing the risk of complications [4].‘Fast track’ surgery also reduces the time to definitive treatment and costs to the health service, whilst increasing resection rates [5]with avoidance of PBD now being recommended in national guidance [6].Importantly, we observed no effects on postoperative renal function or bleeding, given possible concerns over the effects of jaundice upon relevant homeostatic mechanisms.

Fig.1.Changes in blood markers over the postoperative period.Total bilirubin, creatinine and C-reactive protein are summarized using geometric mean, with whiskers representing 95% CI.
There are very limited data available to assess the safety and feasibility of performing venous resection at PD among patients with jaundice.Portal hypertension is associated with renal dysfunction and jaundiced patients tend to have deranged clotting.It is not known whether the interruption of portal blood flow to the jaundiced liver has an adverse effect.Other groups have shown that venous resection can be performed safely but at the expense of a high rate of postoperative laparotomy [7].The North American study by Castleberry et al.[7]reported data from the NSQUIP database and thus differed from the vast majority of publications in this area, which reported single-center outcomes; that study demonstrated that venous resection was performed infrequently and relaparotomy rates were high, particularly among low-volume centers.This has not been our experience.However, our unit is a relatively high-volume liver transplant and HPB center (200-250 transplants, 180-200 pancreas operations and 250-300 liver resections annually), which may explain this difference.
It is insightful to observe that vein patency remained high and most occlusions were in the setting of cancer recurrence and did not lead to complications.However, a small number (2%) of patients did have complications related to the vein which led to death.
Cold stored cadaveric vein grafts offer significant advantage over autologous or prosthetic vein grafts as they are biologic and do not expose the patient to additional surgery to obtain the graft.This study and others confirm the safety of these grafts [8].
In conclusion, this series of patients undergoing venous resection at PD for periampullary cancer demonstrates a relatively lowrate of serious complications, need for relaparotomy and technical failure of the vein anastomosis, regardless of whether surgery is performed in the presence of jaundice.The need for venous resection at PD is not a contraindication to ‘fast track’ surgery without PBD amongst patients with jaundice.

Fig.2.Patency of mesenteric veins following surgery.Patients were censored at the final follow-up or at death.
Acknowledgments
None.
CRediT authorship contribution statement
Rupaly Pande:Data curation, Formal analysis, Writing -original draft, Writing - review & editing.James Hodson:Formal analysis, Writing - review & editing.Ravi Marudanayagam:Supervision, Writing - review & editing.Darius Mirza:Visualization,Writing - review & editing.John Isaac:Visualization, Writing -review & editing.Keith J Roberts:Conceptualization, Methodology,Visualization, Writing - review & editing.
Funding
None.
Ethical approval
This study was approved by the Ethics Committee of our hospital.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Hepatobiliary&Pancreatic Diseases International
- No difference in mortality among ALPPS, two-staged hepatectomy, and portal vein embolization/ligation: A systematic review by updated traditional and network meta-analyses
- Telomerase reactivation is associated with hepatobiliary and pancreatic cancers
- Critical role of estrogen in the progression of chronic liver diseases
- Robotic isolated partial and complete hepatic caudate lobectomy: A single institution experience
- C -C motif chemokine ligand 16 inhibits the progression of liver cirrhosis via inactivating hepatic stellate cells