Robotic isolated partial and complete hepatic caudate lobectomy: A single institution experience
2020-10-23ZhiMingZhaoZhuZengYinLiChaoPanMingGenHuXiangLongTanRongLiu
Zhi-Ming Zhao , Zhu-Zeng Yin , Li-Chao Pan, Ming-Gen Hu, Xiang-Long Tan, Rong Liu
The Second Department of Hepatopancreatobiliary Surgery, The First Medical Center, Chinese People’s Liberation Army General Hospital, Beijing 100853,China
Keywords:
ABSTRACT
Introduction
The caudate lobe (Couinaud’s segment I) is located on the dorsal side of the liver and is surrounded by the hepatic vein,hepatic pedicle, and inferior vena cava (IVC).It can be divided into the Spiegel lobe, caudate process, and paracaval portion [1,2].Healey and Schroy simply divided the caudate lobe into the left dorsal segment and right dorsal segment.The left dorsal segment corresponds to the Spiegel lobe, and the right dorsal segment includes the caudate process and paracaval portion [3].With further understanding of the caudate lobe anatomy, reports on laparoscopic resection of the hepatic caudate lobe have been gradually increasing [4-11], but it is still considered technically challenging and demanding [12].
According to the nature, location, and size of caudate lobe tumors as well as liver function, isolated caudate lobectomy can be categorized into partial and complete caudate lobectomy [ 13 , 14 ].Partial caudate lobectomy includes Spiegel lobectomy, caudate process lobectomy, and paracaval portion lobectomy.As we all know,robotic system provides 3-dimensional visualization, instruments with 7 degrees of freedom and better ergonomics for the operating surgeon.Currently, the Da Vinci robotic system has been widely applied to liver surgery procedure and it has initially shown potential advantages in complex hepatectomy [ 15 , 16 ].However, recent reports on robotic caudate lobectomy are limited to Spiegel lobectomy [17-19].Thus, this study aimed to explore the safety and feasibility of the robotic isolated partial and complete caudate lobectomy.

Fig.1.Trocar placement and intraoperative view of surgical fields after removing the specimen.A: Trocar layout.ASS, assistant port; OPT, optic port; R1-3, robotic port for mechanical Arm 1-3.B: Surgical fields of Spiegel lobectomy.C: Caudate process and paracaval portion lobectomy by right-side approach, the dorsal of right hepatic vein(RHV) and middle hepatic vein (MHV) were exposed.D: Exposure of the inferior vena cava (IVC), RHV and MHV after isolated complete caudate lobectomy.Arantius ligament (black arrow); Stump of the portal pedicle branches of caudate lobe (P, yellow arrow); Inferior vena cava (IVC, white arrow); Right hepatic vein (RHV, blue arrow); Middle hepatic vein (MHV, green arrow).
Patients and methods
Study design
Clinical data of 32 patients who underwent robotic isolated caudate lobectomy in our department from May 2016 to January 2020 were retrospectively analyzed.The patients were divided into three groups according to the location of lobectomy: left dorsal segment lobectomy (Spiegel lobectomy), right dorsal segment lobectomy (caudate process or paracaval portion lobectomy), and complete caudate lobectomy.
The inclusion criteria were as follows: (i) benign diseases of the caudate lobe, (ii) hepatocellular carcinoma, (iii) liver metastasis of colorectal cancer, and (iv) isolated partial or complete caudate lobectomy.The exclusion criteria were as follows: (i) cholangiocarcinoma, (ii) combined with other hepatectomy, (iii) complicated with hepatic vein or IVC invasion, and (iv) hepatic portal lymph node metastasis.
This study was approved by the Ethics Committee of our hospital (S2016-098-02).Written informed consent was obtained from all patients.The operation was performed by surgeons with extensive experience in laparotomy and robotic hepatectomy.
Surgical procedure
Anesthesiaandbodyposition
After general anesthesia, the patient was adopted a 25 °reversed Trendelenburg position and lithotomy position, and the central venous pressure was maintained at 0-5 cmH 2 O.A vertical incision (assistant port) was made at the point superior to the umbilicus, and a Veress needle was inserted through the incision.The pneumoperitoneum pressure of carbon dioxide was established at 14 mmHg, a 12-mm trocar was then inserted, and the robot lens was inserted to complete abdominal cavity exploration.The layout of the trocar port is shown in Fig.1 A.Robotic procedures were performed using the Da Vinci Si Surgical System (Intuitive Surgical Inc., Sunnyvale, CA, USA).Intraoperative ultrasound and Pringle maneuver were routinely used.
Livermobilization,transectionandhemostasis
Mobilization of liver was performed as previously reported [ 17 , 20 , 21 ].Briefly, the left lateral lobe and Spiegel lobe were mobilized for Spiegel lobectomy and complete caudate lobectomy.Limited or completed mobilization of right liver was carried out for caudate process or paracaval portion resection.For all procedure, liver parenchyma transection was achieved using an ultrasonic scalpel.The branches of hepatic veins and hepatic pedicle were ligated using Hem-o-lock clips (TFX Medical, Durham, NC, USA) or Absorbable Ligating Clip Cartridge(COVIDIENTM , Mansfield, MA, USA).Bleeding in the hepatic raw area was coagulated by the bipolar electrodes and electric hook.Opening in hepatic veins were readily sutured with 6-0 prolene by the robotic platform.
Partialcaudatelobectomy
For Spiegel lobectomy, the left lateral liver lobe was retracted upward by Arm 3.When gently anterior retraction of the Spiegel lobe offthe IVC, the short hepatic veins and left caudal branches of the portal vein were identified, divided and clipped.Subsequently,the Spiegel lobe was transected alone the Arantius ligament from the caudal to cranial side ( Fig.1 B).
Right-side approach was usually preferred for caudate process or paracaval portion resection and the right liver portion was retracted upward by Arm 3.After the short hepatic veins and right caudal branches of the posterior pedicle were ligated and dissected, the caudate process parenchyma was transected and the anterior border of the resection plane was the posterior pedicle.Specifically, for the paracaval portion resection, liver transectionproceeded along the dorsal surface of the right hepatic vein (RHV)and middle hepatic vein (MHV) ( Fig.1 C).
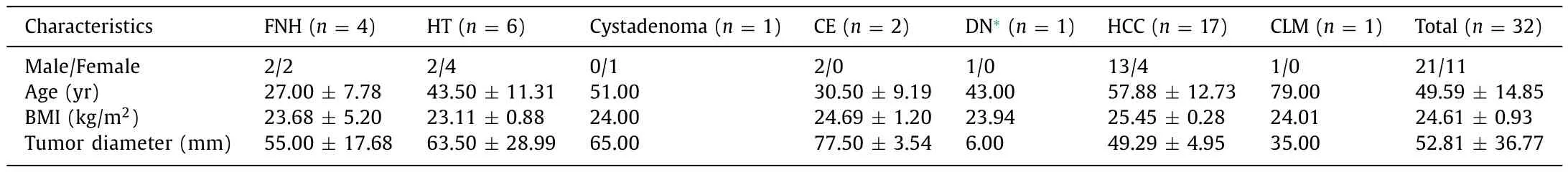
Table 1Patient characteristics and pathology.

Table 2Patient characteristics and surgical outcome of the three groups.
Completecaudatelobectomy
The left-side approach was preferred for total caudate lobectomy.Isolation and division of the short hepatic veins offthe IVC were facilitated by the robotic platform.After complete mobilization of the Spiegel lobe, the caudate process was retracted to the left-side from behind the hepatic pedicle, and the right portal vein branch of the caudate lobe was divided and clipped.Liver parenchyma transection was performed along the IVC from cranial to caudal side.When the dorsal plane of liver between the RHV and MHV was transected, the complete caudate lobectomy was considered to be achieved ( Fig.1 D).
Drainageandspecimen
The surgical field was carefully checked for any bleeding or biliary leakage.The drainage tube was routinely placed on the cross section of the liver or through the Winslow hole, which was led out from robotic Arm 2.The specimens were taken using the extended assistant port in the midline of the upper abdomen.
Perioperative evaluation
The operative time, intraoperative blood loss, blood transfusion rate, postoperative hospital stay, and postoperative complication rate of the three groups were assessed, and the pathological margin of each group was evaluated in case of malignant tumors.Bile leakage was considered when bilirubin level in the drainage fluid from the abdominal drainage tube at 3 days after operation was≥3 times the normal value of serum bilirubin [22].Postoperative complications were assessed according to the Clavien-Dindo classification, and Clavien-Dindo grade III and higher complications were considered serious [23].The comprehensive complication index (CCI) in each group was calculated according to previous literature [24].
Statistical analysis
All data were analyzed and processed by SPSS 20.0 (IBM Corp.,Armonk, NY, USA).The normally distributed data were expressed as mean ±standard deviation (SD), and inter-group comparison was performed using one-way analysis of variance (ANOVA) leastsignificant difference method.The non-normally distributed measurement data were expressed as median (range), and inter-group comparison was performed using the Kruskal-Wallis test.AP<0.05 was considered statistically significant.
Results
Among the 32 patients, 21 were male and 11 were female (age 49.59 ± 14.85 years), with a body mass index (BMI) of 24.61 ±0.93 kg/m2and tumor diameter of 52.81 ±36.77 mm.Among these patients, seventeen had primary hepatocellular carcinoma,one liver metastasis from colorectal cancer, six hepatic hemangioma, four focal nodular hyperplasia, two cystic echinococcosis,one mucinous cystadenoma, and one atypical hyperplastic nodule( Table 1 ).
All 32 patients underwent robotic isolated caudate lobectomy,of which 17 (53.13%) underwent Spiegel lobectomy, 7 (21.88%) underwent caudate process or paracaval portion lobectomy, and 8(25.00%) underwent complete caudate lobectomy.There was no conversion to laparotomy or perioperative death.No difference was noted in age, sex, BMI, tumor diameter, or resection margin of malignant tumor among the three groups; however, significant differences were observed in operative time, intraoperative blood loss,and postoperative hospital stay ( Table 2 ).
The operative time was shorter and blood loss was less of the left dorsal segment lobectomy group (median operative time,114 min; blood loss, 50 mL) compared with those of the right dorsal segment lobectomy group (median operative time, 210 min;blood loss, 100 mL) and complete caudate lobectomy group (median operative time, 197.5 min; blood loss, 100 mL) (operative time:P= 0.010 andP= 0.005; blood loss:P= 0.005 andP= 0.017,respectively).No difference was found in the operative time andblood loss between the right dorsal segment and complete caudate lobectomy groups (P= 1.0 0 0).The postoperative hospital stay of the three groups was compared pairwise, and no significant difference was found between the left dorsal segment lobectomy group and the right dorsal segment lobectomy group (P= 0.240), or between the right dorsal segment lobectomy group and the complete caudate lobectomy group (P= 0.661).However, the median postoperative hospital stay in the left dorsal segment lobectomy group was 4 days, which was significantly shorter than that in the complete caudate lobectomy group (median postoperative hospital stay: 7.5 days,P= 0.003).
Three cases (9.38%) required intraoperative blood transfusion,including one in the right dorsal segment lobectomy group and two in the complete caudate lobectomy group, while no intraoperative blood transfusion was required in the left dorsal segment lobectomy group (P= 0.119).No severe complications of Clavien-Dindo grade III or higher were reported among the three groups after the operation.The incidence rates of Clavien-Dindo grade I complications were 35.29%, 42.86%, and 50.00%, among the three groups, respectively (P= 0.776).Clavien-Dindo grade II complications did not occur in the left and the right dorsal segment lobectomy group, while occurred in two patients (25.00%) in the complete caudate lobectomy group (P= 0.041).However, no difference in the postoperative CCI was found among the three groups(P= 0.159).
Discussion
Hepatectomy for benign lesions (e.g., focal nodular hyperplasia and hepatic hemangioma) were symptomatic or in the presence of uncertainty at preoperative radiologic evaluation.For those who had asymptomatic lesions, biopsy or observation and followup was recommended.Resection for cystic echinococcosis was according to the classification and treatment by the World Health Organization Informal Working Group on Echinococcosis (WHOIWGE) [25].Complete caudate lobectomy was necessary in case of lesions that occupy most of the caudate lobe, as was necessary in two patients.
The caudate lobe is located on the dorsal side of the liver and its anatomy is complicated [ 14 , 26 , 27 ].The caudate lobectomy in open surgery procedures was performed with the ventral field of view.Therefore, its unique anatomical structure makes it difficult to expose the caudate lobe during open hepatectomy, and sometimes combined hepatectomy is required.However, the caudal view is used in laparoscopy and robotic hepatectomy [ 6 , 28 ],which can reveal more clearly the caudate lobe, hepatic pedicle,IVC, and the dorsal of MHV and RHV.
In this study, the operative time and blood loss associated with robotic isolated Spiegel lobectomy were significantly better than those of the caudate process or paracaval portion lobectomy and complete caudate lobectomy groups.The postoperative hospital stay of the partial caudate lobectomy group was significantly shorter than that of the complete caudate lobectomy group.Following review of the clinical data of our team’s robotic left lateral lobectomy cases [21], we found no significant difference between robotic Spiegel lobectomy and left lateral lobectomy in terms of operative time, blood loss, and postoperative hospital stay.In accordance with the reports of Marino et al.[17], we preliminarily believe that robotic Spiegel lobectomy is safe and feasible, and the surgical technique is relatively straightforward, which makes it suitable for beginners.
Partial caudate process or paracaval portion lobectomy usually adopts the right-side or anterior-central approach, which requires dissociation of the right liver lobe or splitting of the liver [ 14 , 29 ].In addition, there is no clear boundary between the caudate process and the right posterior liver lobe, and the liver parenchyma should be transected along the surface of the middle hepatic vein and the right hepatic vein before paracaval portion lobectomy [30].Therefore, in this study, the operative time was significantly longer and blood loss was significantly more in caudate process or paracaval portion lobectomy than those in Spiegel lobectomy.
In complete caudate lobectomy, the dissociation of the dorsal part of the hepatic vein is critical and often leads to catastrophic hemorrhage.Traditional laparoscopy is associated with a great challenge in this step, which is one of the reasons for conversion to laparotomy [ 4 , 6 , 7 ].In robotic complete caudate lobectomy, we found that stable stretching of the mechanical Arm 3 and enlarged 3-dimensional view could more easily and clearly reveal the dorsal side of the hepatic vein.In case of hepatic vein hemorrhage during liver parenchyma disconnection, 6-0 prolene can be used for precise sutures.In this study, eight patients underwent successful robot-assisted complete caudate lobectomy, two patients received blood transfusion during the operation, and no conversion to laparotomy was necessary.Although two patients experienced Clavien-Dindo grade II complications, no difference in the CCI among the three groups was noted.
In conclusion, to our knowledge, this study reported the greatest number of cases of robotic isolated caudate lobectomy.The results of the study preliminarily confirmed that robotic isolated partial and complete caudate lobectomy is safe and feasible.Spiegel lobectomy is relatively straightforward and more suitable for beginners.
Acknowledgments
None.
CRediT authorship contribution statement
Zhi-Ming Zhao:Data curation, Formal analysis, Methodology,Writing - original draft.Zhu-Zeng Yin:Data curation, Formal analysis, Methodology, Writing - original draft.Li-Chao Pan:Data curation, Writing - review & editing.Ming-Gen Hu:Data curation,Writing - review & editing.Xiang-Long Tan:Data curation, Writing - review & editing.Rong Liu:Conceptualization, Supervision,Writing - review & editing.
Funding
None.
Ethical approval
This study was approved by the Ethics Committee of Chinese People’s Liberation Army General Hospital (S2016-098-02).Written informed consent was obtained from all participants.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Hepatobiliary&Pancreatic Diseases International
- No difference in mortality among ALPPS, two-staged hepatectomy, and portal vein embolization/ligation: A systematic review by updated traditional and network meta-analyses
- Telomerase reactivation is associated with hepatobiliary and pancreatic cancers
- Critical role of estrogen in the progression of chronic liver diseases
- C -C motif chemokine ligand 16 inhibits the progression of liver cirrhosis via inactivating hepatic stellate cells
- Dynamic expression of hepatic GP73 mRNA and protein and circulating GP73 during hepatocytes malignant transformation