Incidence and risk factors of pancreatitis in obstructive jaundice patients after percutaneous placement of self-expandable metallic stents
2020-10-23YiYngRuiBoLiuYnLiuHuiJieJing
Yi Yng , , Rui-Bo Liu , Yn Liu , Hui-Jie Jing , ∗
a Department of Radiology, the Second Affiliated Hospital of Harbin Medical University, Harbin 150086, China
b Department of Interventional Radiology, Harbin Medical University Cancer Hospital, Harbin 150081, China
Keywords:
ABSTRACT
Introduction
Periampullary carcinomas are rare, accounting for 5% of all gastrointestinal tract malignancies [1 , 2].Most patients with periampullary carcinoma show no symptom in early-stage and therefore, the clinically diagnosed patients are usually in advanced stage which makes the tumorectomy impossible.In order to alleviate the corresponding clinical symptoms and improve the quality of life,percutaneous self-expandable metallic stent is used as a preferred treatment [3-6].
Percutaneous self-expandable metallic stent insertion is a well-established method for palliating a patient with inoperative malignant biliary abnormalities that were caused by pancreatic cancer, liver cancer, gallbladder carcinoma and metastatic lymphadenopathy.However, when treating obstructive jaundice, pancreatitis is a serious but rare complication [7 , 8].Although there are many studies on the sequel after the implantation of palliative stenting for unrespectable tumors, little is known about risk factors that are associated with the complications [9].
The present study reported the incidence and risk factors of pancreatitis after percutaneous self-expandable metallic stent placement in 980 patients with obstructive jaundice due to different malignancies.
Patients and methods
Patients
This retrospective study was approved by the Institutional Review Board of Harbin Medical University Cancer Hospital.Written informed consent was obtained from all participants.We collected the data of patients who had self-expandable metallic stents via a percutaneous transhepatic biliary drainage (PTBD)tract.According to the enrollment criteria including aging over 18 years old, without pancreatitis in nearly 3 months, and signed the informed consent form, 1560 patients were involved in our study from January 2010 to October 2016.However, 580 of them were excluded due to the loss of follow-up or other reasons.Ultimately, a total of 980 patients (448 males and 532 females; median age 67 years, ranging 27-88 years) were included.All of the diagnosis of tumor and obstructive jaundice were based on clinical manifestation that were incorporated with computed tomography (CT), magnetic resonance cholangiopancreatography (MRCP),cholangiogram findings and serum bilirubin levels.Indications for biliary stent include cholangiocarcinoma (48.3%), pancreatic carcinoma (16.6%), gastrointestinal carcinoma (14.9%), gallbladder carcinoma (9.1%), hepatocellular carcinoma with bile duct invasion(9.2%), and other (1.9%).
Preoperative preparation
All patients were required to have a maximum international normalization ratio (INR) of 2.0 and a minimum platelet count of 5 ×109/L.For those who did not meet the standard, appropriate transfusions or vitamin K1 were prescribed to decrease the risk of bleeding and ensure safety.
Intervention process
PTBD was performed to treat obstructive jaundice and provide access for the placement of a biliary stent.Local anesthesia was performed using intramuscular 2% lidocaine hydrochloride and conscious sedation.To be more specific, a 5 mL disposable syringe was inserted along the puncture path.No blood was extracted and 3 mL of 2% lidocaine hydrochloride was injected while withdrawing.The intrahepatic bile duct was punctured under fluoroscopic or ultrasound guidance with a 21-gage Chiba needle (Cook, Bloomington, IN, USA).Through a 0.018 inch guide wire (Cook), a PTBD catheter was advanced into the bile duct.The stenosis site and exact anatomy of the bile duct were assessed via cholangiograms.The length of stent was 4-10 cm and the diameter of stent was 6-10 mm according to the obstructive site.Before removing the PTBD catheter, the 0.035 inch guide wire was inserted, and a 5-F catheter was advanced through it.All the procedures were conducted according to the standard guideline.The guide wire and catheter were advanced across the stenosis to the duodenum and the contrast media was injected into the catheter.After that, the obstructive length was measured, and the suitable stent was chosen to lie across the stenosis.Balloon dilation of the stenosis was not routinely performed unless the stenosis was too tight to place the stent.Stent was at least 2-3 cm longer than the stricture since the stricture needs to be covered completely, including the proximal and distal adjacent portions.The median length of stent was 6 cm (range 4-10 cm) and the diameters ranged from 6 to 10 mm.The process was shown in the Fig.1.
Follow-up
All patients were followed up at every 2-day interval after the stent replacements.A higher level of bilirubin is a more sensitive indicator of stent obstruction compared with fever [10].In case of recurrent jaundice or increasing bilirubin levels, CT scans were used to evaluate the obstruction.In the case of stent occlusion, we performed decompressions of the bile duct by secondary percutaneous interventional procedures depending on the condition of the patients.
Pancreatitis diagnostic criteria
The diagnosis of pancreatitis was based on the symptom of the patient, the laboratory indexes and radiological features [11].The symptom of pancreatitis is abdominal pain accompanying with abdominal distension, vomiting and nausea.In laboratory aspect, the serum amylase, lipase and the white blood cell count were increased.Radiologic features include CT and ultrasonography.
Risk factors for pancreatitis
Risk factors for the development of pancreatitis were evaluated by analyzing several demographic, pathologic, laboratory and stent variables.Demographic variables included patient age, sex, site of the stent; pathologic variables including the bile duct situation;laboratory variables consisted of white blood cell count, platelet count, INR, prothrombin activity and total bilirubin; stent variables incorporated the diameter and length of stent and the number of stents.However, the causes of obstructive jaundice were different and the 1079 stents were placed by more than 15 operators with varying experience with biliary interventions.These factors were not analyzed as the potential risk factors for pancreatitis.
Statistical analysis
The serum total bilirubin levels, serum amylase and lipase levels before admission and during hospitalization were analyzed by the paired samplet-test.Variables found to be significant for pancreatitis at univariate simple logistic regression analysis (P<0.05)were selected into multivariate analysis to determine which factor was the significant independent factors.Multivariate analysis was performed, with variables selected in a stepwise forward manner.All statistical analysis was performed by SPSS software (version 19.0; SPSS Inc., Chicago, IL, USA).APvalue less than 0.05 was considered statistically significant.
Results
The rate of pancreatitis
Among the 980 patients undergone stents placement during the study period, 45 (4.6%) resulted in pancreatitis.After operation,pancreatitis was detected within 1 day in 29 patients (64.4%), at day 2 in 12 patients (26.7%), and at day 3-5 in 4 patients (8.9%).Only 1 patient died of severe acute pancreatitis within 1 day after the operation.The 45 patients with pancreatitis had some or all symptoms of pancreatitis ( Table 1 ).
Risk factors analysis
Univariate analysis showed that white blood cell count>10 ×109/L (Odds ratio [OR]= 5.338;P<0.001), platelet count<5 ×109/L (OR = 9.898;P<0.001), INR>2 (OR = 17.979;P<0.001), prothrombin activity<40% (OR = 13.330;P<0.001),total bilirubin ≥300 μmol/L (OR = 9.681;P<0.001), albumin<25 g/L (OR = 19.575;P<0.001), using one stent (OR = 0.107;P<0.001), and common bile duct stent placement (OR = 2.469;P= 0.021) were significantly associated with the incidence of pancreatitis ( Table 2 ).Multivariate regression analysis showed thatcommon bile duct stent placement (OR = 2.096, 95% CI: 1.248-5.379;P= 0.002) was the only independent risk factor associated with the development of pancreatitis ( Table 3 ).Therefore, the obstructive site in common bile duct had 2.096 times risk of pancreatitis compared to intrahepatic bile duct stent placement when the patients chose the stents to relieve obstructive jaundice.

Fig.1.A 62-year-old male with obstructive jaundice resulting from pancreatic cancer underwent the placement of self-expandable metallic stent.A: CT showed a solid tumor in head of pancreas (arrow) at postoperative day 15.B: MRCP showed the obstructive site was located in the junction of pancreatic duct and common bile duct (arrow).C:Angiogram imaging showed the stent crossed the duodenal papilla (arrow).
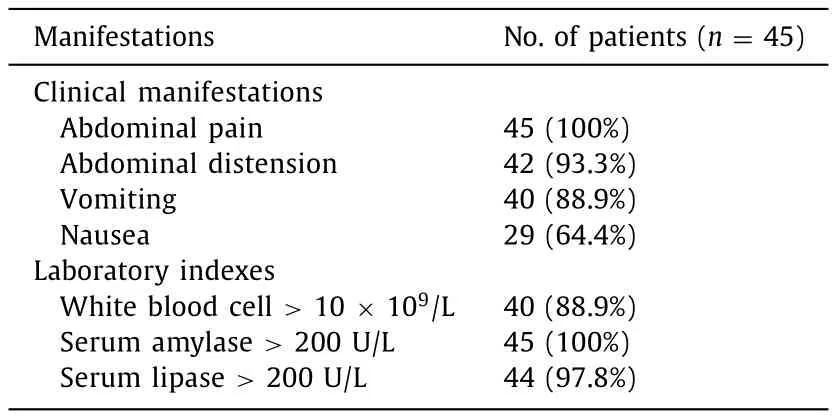
Table 1The laboratory indexes and the symptom of pancreatitis.

Table 3Multivariate logistic regression analysis of risk factors associated with pancreatitis.
Treatment outcomes
Among the 45 patients with pancreatitis, somatostatin had no effect on one patient who died of severe acute pancreatitis within 1 day after the operation.Somatostatin relieved the corresponding symptoms and decreased the levels of serum amylase and lipase in 44 patients.The median maximum serum amylase and li-INR: international normalized ratio.pase levels were 628 U/L (range 167-921 U/L) and 465 U/L (range 235-584 U/L), respectively.The levels of serum amylase and lipase gradually decreased at days 4 in most patients ( Fig.2 ).

Table 2Univariate logistic regression analysis of risk factors associated with pancreatitis.
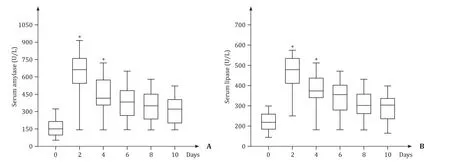
Fig.2.The levels of serum amylase ( A) and lipase ( B) of patients with pancreatitis within 10 days.∗P < 0.05.
The dosage of somatostatin was 4 mg per day by intravenous injection for 14 days.Of the 44 patients treated with somatostatin,12 (27.3%) experienced minor complications.Complications mentioned above may have no association with the using of somatostatin and was probably resulted from the damage of pancreatic function.No major complications were observed in any of the 44 patients.
Discussion
To our knowledge, percutaneous placement of self-expandable metallic stent is a recognized and established method of treatment in patients with obstructive jaundice [12].Treatment options to achieve biliary drainage including PTBD, endoscopic and surgical resection [13].Each treatment has its own pros and cons.Most of patients are not suitable for surgical treatment because of the late diagnosis [14].Although endoscopic approach is generally recommended for obstructive jaundice, percutaneous approach is much easier to target the bile duct with ultrasound guidance compared to an endoscopic approach [15].Percutaneous placement of stent is a preferred method with lower incidence of infection and availability of interventional expertise [16].No matter which method of intervention is chosen, it is aiming at relieving the symptoms related to jaundice, including preventing liver dysfunction and cholangitis [17].With the modifications and improvements in technique of PTBD, multi-functional advances in stent design have made its deployment safe and effective, making stent an acceptable option in patients with obstructive jaundice.The stents have several advantages including higher levels of patency, shorter hospital stay and lower overall cost than traditional treatment.It is also well-known that advances in chemotherapy and radiotherapy from part of the palliative treatment can prolong life expectancy in patients who have had stents inserted and thereby possibly outliving the stent patency period [18-20].
The complications of stenting included bleeding, perforation,bacteremia, pancreatitis, cholangitis, fever, pain and other reversible symptoms.Previous studies [21 , 22]showed that the overall complication rate was 8% −42%, with early complications ranging from 9.7% to 17% in the patients who had undergone the placement of stents.Our study was focused on pancreatitis caused by the stents.Most of our pancreatitis cases were diagnosed within postoperative day 1.All patients were treated with somatostatin and other necessary methods timely.Somatostatin was an effective and safe drug for patients with pancreatitis.It can inhibit the secretion of pancreatic juice and promote the recovery of pancreatic function.Placement of gastric tube was a useful method to decompress the pressure of gastrointestinal and forestall patients to eat and drink anything while sufficient nutrition was provided during this period.Antibiotics were given if necessary.At the same time, the condition changes and the levels of serum amylase and lipase were monitored.
The end points for treatment were to decrease the serum amylase and lipase levels to normal and relieve the symptoms.Somatostatin was used for two more days than other treatments in case of the recurrence of pancreatitis.
Our univariate analysis showed white blood cell count>10 × 109/L, platelet count<5 × 109/L, INR>2, prothrombin activity<40%, total bilirubin ≥300 μmol/L, albumin<25 g/L, number of stents, and common bile duct stent placement were significantly associated with the development of pancreatitis.The multivariate analysis, however, showed that common bile duct stent placement was the only independent risk factor associated with the development of pancreatitis.One explanation that stent placement predisposes patients to pancreatitis may be the anatomic arrangement of the area of watt ampulla in the duodenum.When the obstructive site located in common bile duct or pancreas head, the distal stent can oppress the pancreas tube more frequently, causing pancreatitis.The direct stimulation by distal stent especially common bile duct stent placement may be one of the reasons that caused the pancreatitis.In this study, patients who underwent common bile duct stent placement had 2.096 times risk of pancreatitis compared to intrahepatic bile duct stent locations.For these patients,PTBD is a better option to solve the high levels of serum bilirubin,although there is potential of increased risks of other complications by PTBD.
After treatment, only 1 patient died of severe acute pancreatitis within 1 day.Forty-four patients demonstrated stable situation.Twelve patients experienced minor complications.All the minor complications were completely resolved by conservative treatments and percutaneous pancreatic pseudocyst drainage under ultrasound guidance.Somatostatin may have some impact on recovery of the pancreatic function and decreasing the major complications.
Our study had several limitations.The retrospective design may restrict the evaluation of risk factors for pancreatitis.Other factors instead of stent placement may also play a role in pancreatitis.The uneven surgical skill among surgeons may also cause different outcomes after operation.
In conclusion, percutaneous placement of self-expandable metallic stent offered a secure and efficacious method in dealingwith obstructive jaundice.Pancreatitis is a relatively low complication of stent placement.Common bile duct stent placement is the only independent risk factor associated with pancreatitis.Hence,PTBD is preferable for patients with distal bile duct obstruction.Moreover, somatostatin is a safe and effective method for pancreatitis resulted from stent placement.
Acknowledgments
None.
CRediT authorship contribution statement
Yi Yang:Data curation, Formal analysis, Investigation, Writing -original draft.Rui-Bao Liu:Methodology, Writing - original draft.Yan Liu:Methodology, Writing - original draft.Hui-Jie Jiang:Conceptualization, Funding acquisition, Supervision, Writing - review& editing.
Funding
This study was supported by grants from the National Key Research and Development Program of China ( 2019YFC0118100 ),the National Natural Science Foundation of China ( 81671760 and 81873910 ), Scientific Research Transformation Special Fund of Heilongjiang Academy of Medical Sciences ( 2018415 ), Scientific Research Project of Health and Family Planning Commission of Heilongjiang Province ( 201812 and 201622 ).
Ethical approval
This study was approved by the Ethics Committee of the Harbin Medical University Cancer Hospital.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Hepatobiliary&Pancreatic Diseases International
- No difference in mortality among ALPPS, two-staged hepatectomy, and portal vein embolization/ligation: A systematic review by updated traditional and network meta-analyses
- Telomerase reactivation is associated with hepatobiliary and pancreatic cancers
- Critical role of estrogen in the progression of chronic liver diseases
- Robotic isolated partial and complete hepatic caudate lobectomy: A single institution experience
- C -C motif chemokine ligand 16 inhibits the progression of liver cirrhosis via inactivating hepatic stellate cells