Risk factors for delayed hemorrhage after endoscopic sphincterotomy
2020-10-23JingYnChunXiZhouChongWngYunYunLiLeYingYngYouXingChenJinJinHuGuoHuLi
Jing Yn , Chun-Xi Zhou , Chong Wng , Yun-Yun Li , Le-Ying Yng , You-Xing Chen ,Jin-Jin Hu b , Guo-Hu Li , ∗
a Department of Gastroenterology, The First Affiliated Hospital of Nanchang University, Nanchang 330 0 06, China
b Department of Urology, The First Affiliated Hospital of Nanchang University, Nanchang 330 0 06, China
Keywords:
ABSTRACT
Introduction
Since first introduced in 1974, endoscopic sphincterotomy(EST), as a standard therapy of pancreaticobiliary diseases during endoscopic retrograde cholangiopancreatography (ERCP), has some obvious complications, such as post-procedure pancreatitis,perforation, and hemorrhage [1 , 2].Among them, postoperative hemorrhage is one of the most severe complications, and the incidence ranged from 0 to 27% [2 -4].Minor hemorrhage is often self-limited and ceases without special treatment, while major hemorrhage may be lethal and require endoscopic hemostasis or interventional therapy.At present, the risk factors for post-EST delayed hemorrhage have not been analyzed in China.Therefore,this study aimed to explore the risk factors for post-EST delayed hemorrhage and suggest some precautionary measures.
Methods
Patients
The patients who successfully underwent ERCP and EST in the First Affiliated Hospital of Nanchang University between January 2007 and June 2015 were analyzed.Among 8477 patients, 137(77 males and 60 females; aged from 22 to 85 years, median 57 years) had post-EST delayed hemorrhage and 8340 (3942 males and 4398 females; aged from 12 to 90 years, median 58 years)had no post-EST hemorrhage.Cholelithiasis was the most common ERCP indication.The clinical characteristics are listed in Table 1.The patients with platelet less than 50 ×109/L, bilirubin enzyme separation or total bilirubin (TBIL) greater than 500 μmol/L, prothrombin time (PT) prolonged more than 6 s or international normalized ratio (INR) greater than 1.5 times the upper limit of normal, the use of antiplatelet and anticoagulant drugs, and the presence of severe chronic renal insufficiency and cardiopulmonary disease were excluded.The reason why we excluded the groups at high-risk of bleeding was that those factors are con-traindicative for EST and have been repeatedly identified by many studies.For those patients, we chose to remove the obstruction with nasobiliary drainage or bile duct stent to ensure safety.The present study was approved by the institutional review board of our hospital, which waived the requirement for written informed consent because of the retrospective nature of the study.
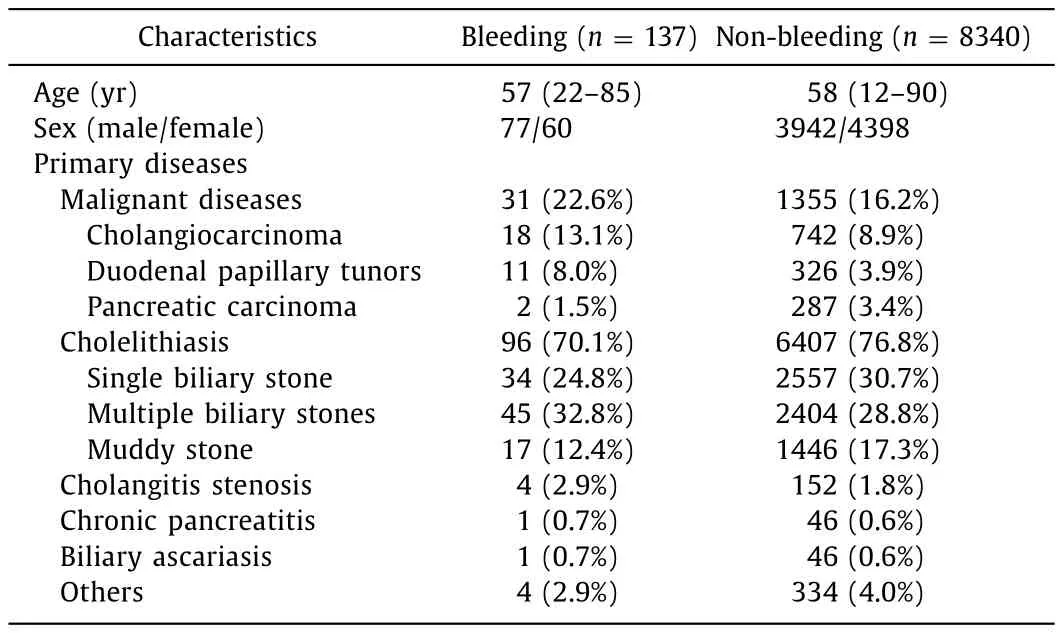
Table 1Clinical characteristics.
Procedure
We adopted the Olympus JF-240 side-view duodenoscopy(Olympus Optical Co., Ltd., Tokyo, Japan), ERBE Vio 200 sAPC(ERBE, Tübingen, Germany), Olympus MAJ-244 basket and disposable papillotomy knife (Olympus Optical Co., Ltd.,), Boston Jagwire(Jagwire Boston Scientific, Miami, FL, USA), Cook nasal biliary drainage catheter (COOK, Winston-Salem, NC, USA) and others.The patient was placed in the left prone position and sedated with propofol.Conventional guidewire was used to guide the intubation.If the intubation was difficult, pre-cutting or other methods were used.All patients underwent EST during surgery and were observed after EST to determine if there was immediate bleeding.Minor bleeding stopped without special treatment, and major bleeding was treated with endoscopic hemostasis.Blood amylase levels and routine blood tests were monitored after the operation.Patients were given a liquid diet if their blood amylase levels at 3 postoperative hours and the next morning were all normal.If hematemesis, hematochezia, and hemic fluid drained by a nasal biliary catheter after ERCP appeared or a review of the routine blood tests suggested that the hemoglobin level had declined, then it was necessary to promptly determine the reason for bleeding via endoscopy and initiate appropriate hemostasis measures according to the situation.Patients were discharged after stopping/no bleeding and other complications for more than 2 days, and generally followed up through the outpatient service or over the telephone.
Definitions
Post-EST hemorrhage was defined as hemorrhage diagnosed endoscopically within 7 days after EST [2].Early hemorrhage was defined as hemorrhage during the operation or within 24 h of the operation.Delayed hemorrhage was defined as hemorrhage occurring more than 24 h after EST [5].The severity of bleeding was categorized as mild, moderate, or severe.Mild bleeding was defined as a decrease in hemoglobin<3 g and no need for transfusion.Moderate bleeding was defined as the need for transfusion (4 units or less) but no need for interventional therapy (angiographic or surgical).Severe bleeding was defined as the need for transfusion(5 units or more) or interventional therapy (angiographic or surgical) [6].The severity of jaundice was definitions [7]: no jaundice,TBIL<34.2 μmol/L; mild jaundice, TBIL 34.2-171 μmol/L; moderate jaundice, 171-342 μmol/L; and severe jaundice, TBIL>342μmol/L.The line between the duodenal papilla opening and root was defined as 12 o’clock.EST is generally operated between 11 and 1 o’clock, and a directional deviation of incision was defined as a direction of incision outside of the range from 11 to 1 o’clock ( Fig.1 ).

Fig.1.The direction of incision of endoscopic sphincterotomy.
Statistical analysis
The statistical analysis was performed using SPSS 17.0 (SPSS Inc., Chicago, IL, USA).All variables were qualitative, and the Chi-square test or Fisher exact test were used for analysis.Variables with statistical significance in the univariate analysis were included in the logistic regression for the multivariate analysis.APvalue<0.05 was considered statistically significant.
Results
Of the 137 patients (1.62%) with delayed hemorrhage ( Table 2 ),18 were diagnosed more than 72 h after ERCP, 27 were within 48-72 h, and the others were within 24-48 h.Among them, 90 had only melena, 11 had only hematemesis, 14 had only hemic fluid drained by a nasal biliary catheter and 22 had hybrid symptoms.The hemorrhage degree was mild in 101, moderate in 29 and severe in 7.All hemorrhages were successfully controlled:sixty patients with mild hemorrhage were controlled with drugs,one patient with severe bleeding was controlled via interventional therapy ( Fig.2 ) and the rest (76) were controlled by the combination of drugs and endoscopic hemostasis ( Fig.3 ).
Univariate and multivariate analyses were used to analyze the risk factors for delayed hemorrhage.Influential factors include patient-related factors (age, sex, the severity of jaundice, the size and number of stones and underlying diseases) and operationrelated factors (stone removal basket, endoscopic papillary balloondilation, intraoperative bleeding, pre-cutting, the directional deviation and length of incision).Univariate analysis showed that male,the severity of jaundice, duodenal papillary tumors, diabetes, intraoperative bleeding, moderate and large incisions, and directional deviation of incision were risk factors for post-EST delayed hemorrhage (P<0.05) ( Table 3 ).Multivariate analysis demonstrated that intraoperative bleeding [odds ratio (OR) = 3.326; 95% CI:1.785-6.196;P<0.001]and directional deviation of incision(OR = 2.184; 95% CI: 1.266-3.767;P= 0.005) were risk factors for post-EST delayed hemorrhage ( Table 4 ).
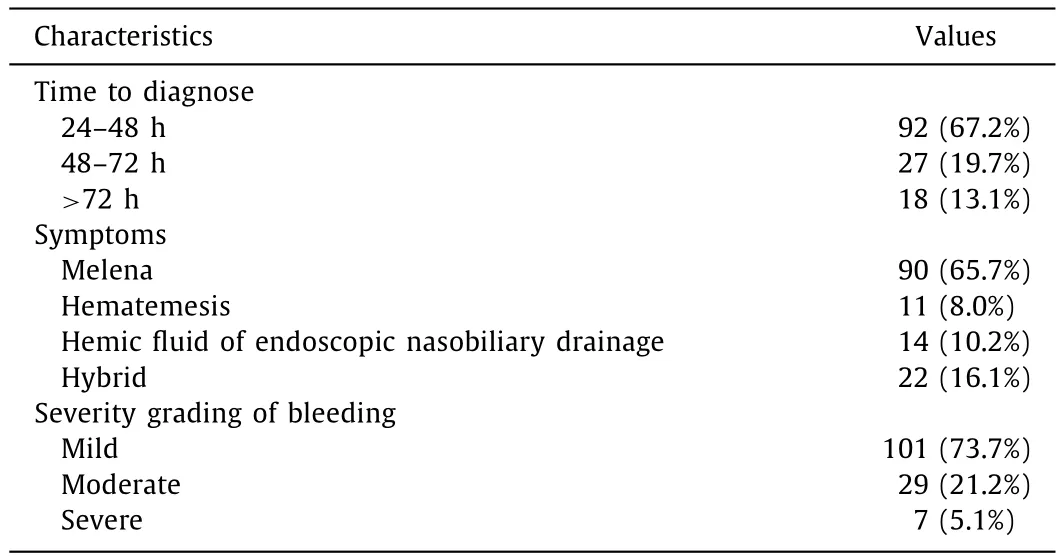
Table 2Patients characteristics ( n = 137).
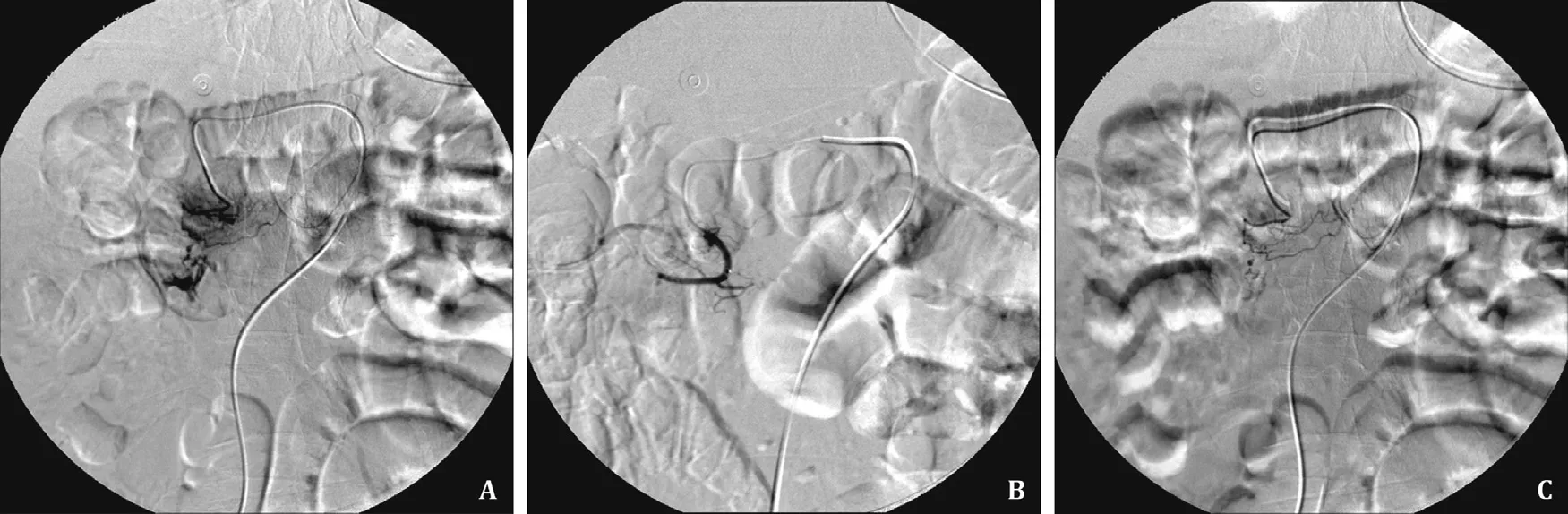
Fig.2.Interventional therapy, contrast medium overflowed from a branch of duodenal artery ( A), embolization was in progress ( B ), embolization was successful and bleeding stopped ( C).

Fig.3.Methods of endoscopic hemostasis, electrocoagulation ( A), balloon tamponade ( B), endoscopic clip placement ( C).
Discussion
EST is one of the crucial modalities of ERCP.Despite improvements in the ERCP process, EST is still recognized as a challenging modality with a high failure rate and postoperative complications.Previous studies [6 , 8-16]have reported some risk factors, including needle-knife sphincterotomy, the type of current,intraoperative bleeding, the direction and length of incision, the skill of the endoscopist, coagulopathy, active cholangitis, the use of anticoagulants, uncontrolled cutting, periampullary diverticula,and hemodialysis.Although there have been many studies on the risk factors for post-EST hemorrhage, few have focused on delayed hemorrhage [2 , 3].In our study, the incidence of post-EST delayed hemorrhage was 1.62%.Intraoperative bleeding and directional deviation of incision are risk factors for post-EST delayed hemorrhage.
Our results are in accordance with those of previous studies that found that intraoperative bleeding, directional deviation of incision, and moderate and large incisions are risk factors for post-EST hemorrhage [2 , 3 , 14 , 16 , 17].Williams et al.[14]deemed visible bleeding in the procedure a potential risk factor for hemorrhage.Furthermore, a recent study [2]reported that 9.3% of patients develop delayed hemorrhage after intraoperative bleeding.It is reasonable to believe that intraoperative bleeding increases the risk of postoperative hemorrhage.EST is generally operated in the 11-1 o’clock region in the longitudinal direction of the papilla fold [18].The direction of incision may skew in operation, and the distal common bile duct and duodenal papilla are supplied by the posterior duodenal artery, a branch of the superior pancreaticoduodenal artery.The artery is approximately 1-2 mm in diameter,and more than 15% of the duodenal posterior artery forms a vascular network at the duodenal wall near the papilla.Furthermore,most arteries are located on the left of the papilla fold.Therefore,it is easy to damage the vascular network when the incision is left at 11 o’clock, which leads to bleeding.Many studies [3 , 14 , 17]showed that a large incision significantly increased the risk of bleeding compared to a small or moderate-to-large incision for the following reasons.First, a large incision easily damages the blood vessels.Second, a deeper incision is likely to injure the arteries deep in the tissue [17].
Previous studies [9 , 19]suggested that age younger than 40 years old and female were risk factors for delayed hemorrhage.A series of studies recommended that more attention should be paid to young people because of the high possibility of bleeding [20].However, some studies believed that pediatric EST has a high degree of technical success and low rates of adverse events [21].Although we found that age was not a risk factor,there is a trend towards male being a risk factor in our study.
Hypertension has been proven to be significantly associated with post-EST delayed hemorrhage [3].Hypertension is also considered a high-risk factor for postoperative hemorrhage, as it is closely related to the vascular pressure of the intraoperative incision.In our study, all patients with hypertension were treated with antihypertensive drugs until the day of ERCP, and if their blood pressure was poorly controlled, the ERCP was canceled.Thus, theresults of our study showed that hypertension was not a risk factor for post-EST delayed hemorrhage.Diabetes with poor glycemic control is also considered a possible risk factor for postoperative hemorrhage.It may be associated with microvascular disease and the increased angiogenin caused by diabetes.Our study demonstrated that diabetes was related to delayed hemorrhage.

Table 3Risk factors for the delayed hemorrhage.
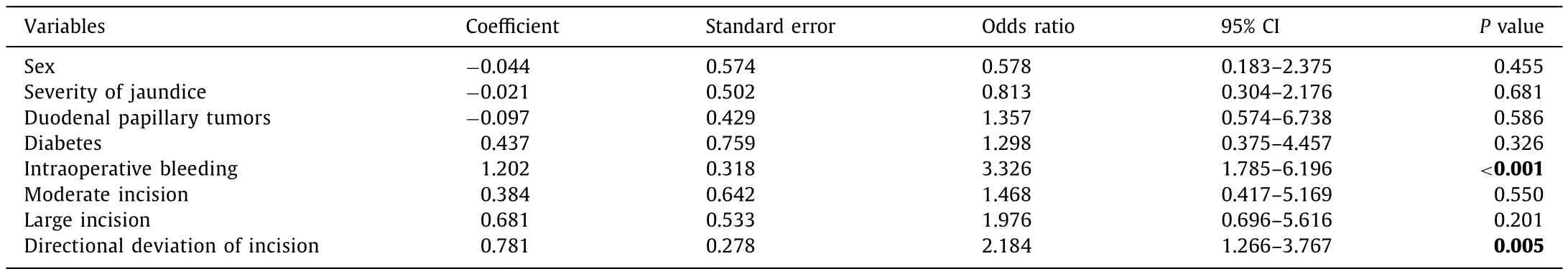
Table 4The results of multivariate analysis.
Reports regarding the relationship between bleeding and tumors are rare.The reason duodenal papillary adenoma and carcinoma are more inclined to bleed may be the richness of the blood supply, and the weakness of the mucosa or the erosion of the vessel by the tumor.A previous study stated that the bleeding risk is increased when EST is performed on papillary tumors [22].
As there is an absence of bile in the alimentary tract in obstructive jaundice, it also affects the absorption of vitamin K, which leads to a coagulation disorder [23].A study by Lin et al.[24]revealed that a high serum bilirubin level was associated with post-EST hemorrhage.Williams et al.[14]also found that a high bilirubin level is a potential risk factor for hemorrhage.
Many studies [25 -29]found that anticoagulants and coagulopathy are associated with risk factors for post-EST hemorrhage.And Ikarashi et al.[2]and Nakaji et al.[6]reported that hemodialysis was a strong risk factor for post-EST hemorrhage.These factors have been repeatedly identified as possible risk factors for post-EST hemorrhage.We did not do EST for the patients who took non-steroidal antiplatelet aggregation drugs and anticoagulant drugs before ERCP, or who had a PT prolonged past 6 s or an INR greater than 1.5 times the upper limit of normal, or who had renal insufficiency.
For experienced endoscopists, more than 90% of patients can be intubated successfully, but 5% −10% of patients are difficult to intubate [30 , 31].Pre-cutting is the main technique used if conventional intubation fails.Therefore, needle-knife sphincterotomy is a common pre-cutting technique.Some studies have demonstratedthat pre-cutting is related not only to post-ERCP pancreatitis but also to biliary bleeding and perforation, especially needle-knife sphincterotomy [14 , 22 , 32].Another study found that pre-cutting,including three different pre-cutting methods, was not a risk factor for post-EST hemorrhage [33].Navaneethan et al.[34]emphasized that a successful pre-cutting sphincterotomy is not associated with an increased risk of adverse events.This discrepancy can be explained by the different experience levels of the endoscopists.Our results also showed that pre-cutting was not a risk factor for post-EST delayed hemorrhage.
To explore the factors affecting post-EST hemorrhage is of vital importance, as is the sensible selection of patients for ERCP.Strategies to identify, minimize, and manage high-risk factors are necessary for the endoscopist.In this study, 60 patients with mild hemorrhage achieved control with drugs, and 76 patients with mild, moderate or severe hemorrhage were controlled with the combination of drugs and endoscopic hemostasis.One patient with severe bleeding was controlled by interventional therapy.All patients with hemorrhage successfully recovered.Any bleeding that occurs during EST increases the risk for the incidence of delayed hemorrhage, and it is suggested that appropriately controlling immediate bleeding may reduce the risk of delayed hemorrhage [8 , 9].Moreover, using a blended current reduced the risk of immediate bleeding [13].In addition, to prevent delayed hemorrhage, the endoscopists should avoid papilla with a large incision during operation, control the speed of the incision, and shorten incisions with the zipper type.With regard to therapy, the injection of epinephrine is the preferred endoscopic hemostasis method.The other endoscopic hemostasis methods include balloon tamponade, endoscopic clip placement, self-expandable metallic stents, bipolar or multipolar electrocoagulation, and angiographic embolization or surgery, if necessary [13 , 16 , 35 , 36].
In conclusion, delayed hemorrhage is the most common and dangerous complication of EST.Intraoperative bleeding and the directional deviation of incision were risk factors for delayed hemorrhage.For the relevant risk factors, careful observation after EST and application of the corresponding therapeutic measures are needed.
Acknowledgments
None.
CRediT authorship contribution statement
Jing Yan:Formal analysis, Investigation, Writing - original draft.Chun-Xia Zhou:Resources, Writing - review & editing.Chong Wang:Formal analysis.Yuan-Yuan Li:Supervision.Le-Ying Yang:Formal analysis.You-Xiang Chen:Conceptualization, Writing - review & editing.Jian-Jian Hu:Data curation.Guo-Hua Li:Conceptualization, Supervision, Writing - review & editing.
Funding
None.
Ethical approval
The study was approved by the institutional review board of the First Affiliated Hospital of Nanchang University.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Hepatobiliary&Pancreatic Diseases International
- No difference in mortality among ALPPS, two-staged hepatectomy, and portal vein embolization/ligation: A systematic review by updated traditional and network meta-analyses
- Telomerase reactivation is associated with hepatobiliary and pancreatic cancers
- Critical role of estrogen in the progression of chronic liver diseases
- Robotic isolated partial and complete hepatic caudate lobectomy: A single institution experience
- C -C motif chemokine ligand 16 inhibits the progression of liver cirrhosis via inactivating hepatic stellate cells