高龄孕妇妊娠晚期的常规心电图改变
2020-07-27周翠梅
周翠梅
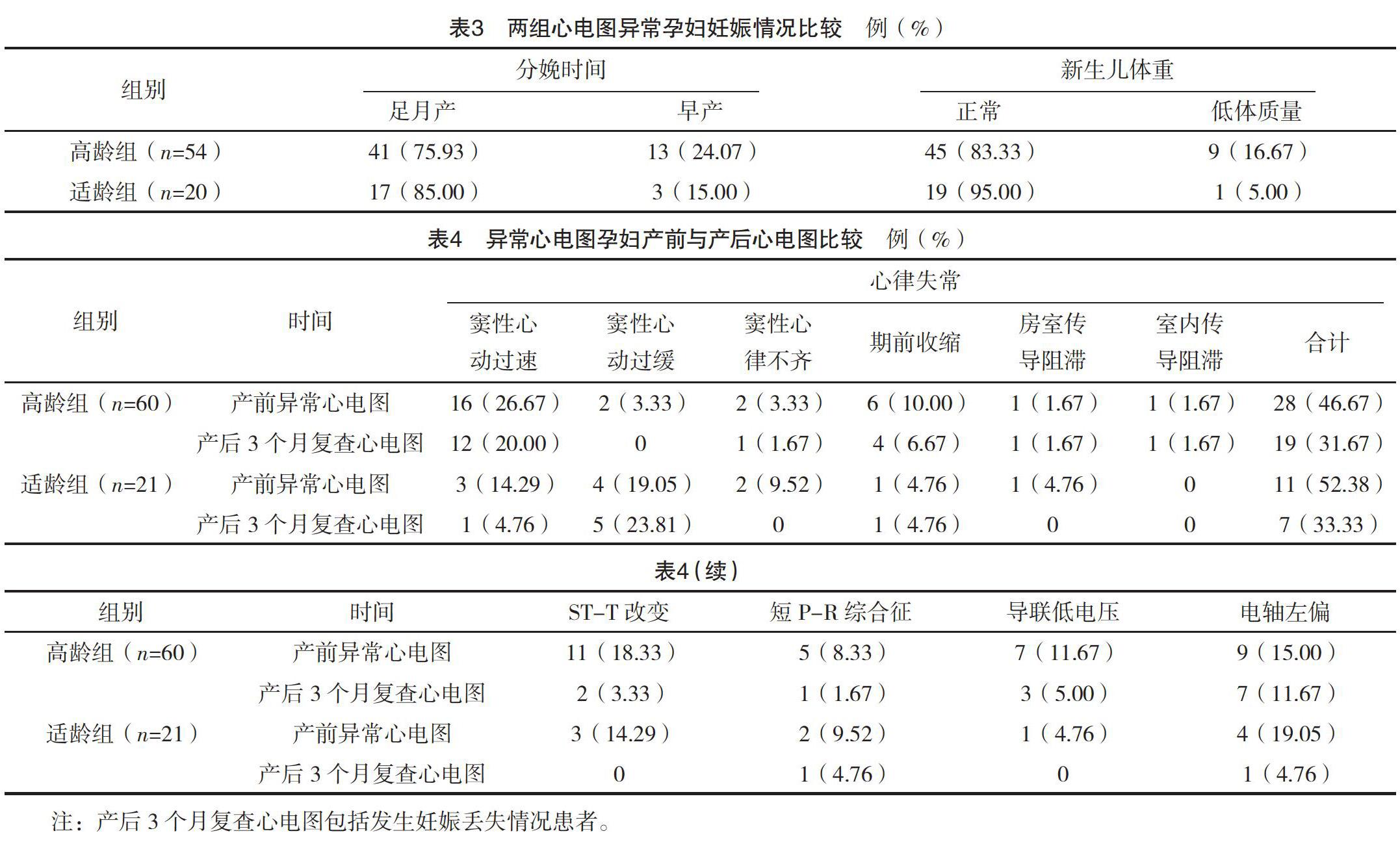

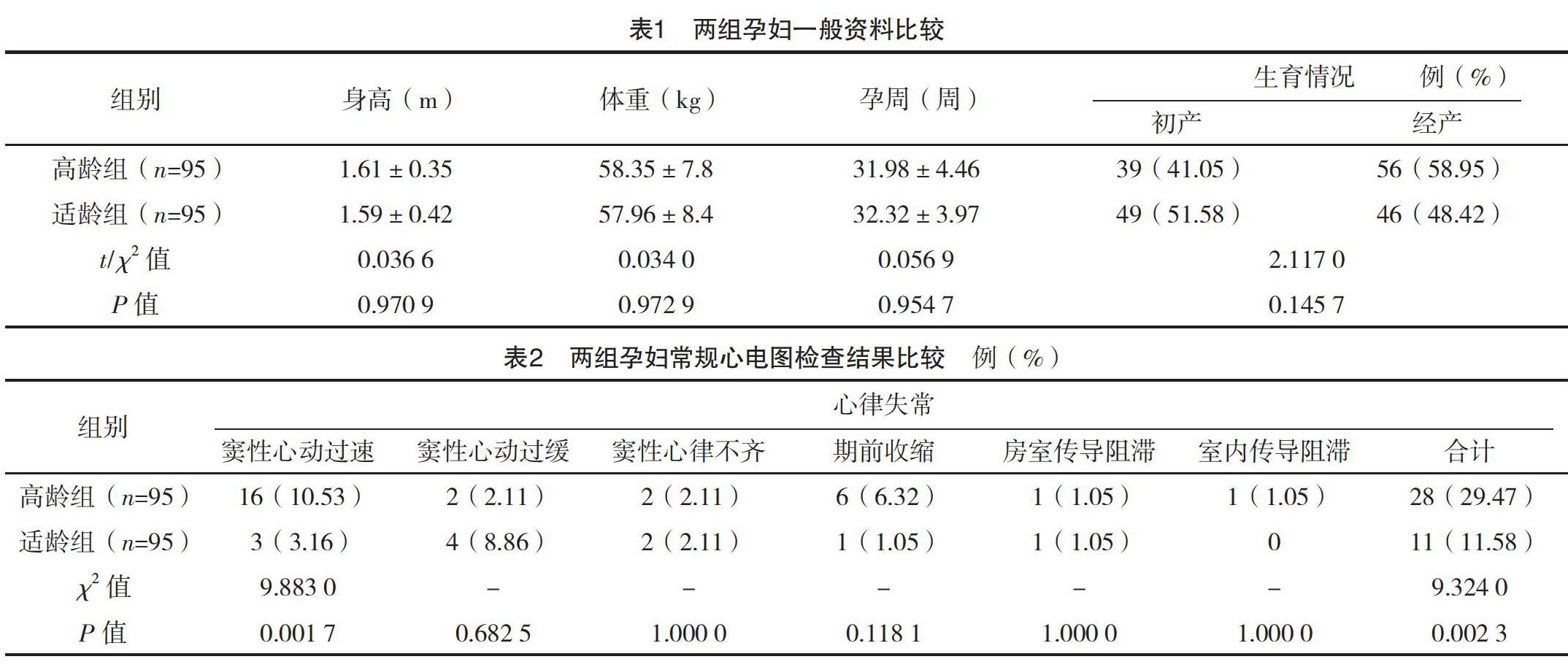
【摘要】 目的:探究高齡孕妇妊娠晚期的心电图特点,为临床提供指导。方法:选取2017年1月-2019年6月在本院行心电图检查的妊娠晚期孕妇190例。根据年龄进行分组,年龄≥35岁的95例孕妇作为高龄组,年龄<35岁的95例孕妇为适龄组。观察两组孕妇常规心电图检查结果,比较两组心电图异常孕妇妊娠情况及产前与产后心电图变化情况。结果:高龄组孕妇妊娠晚期异常心电图的发生率为63.16%,高于适龄组的22.11%,其中心律失常、窦性心律过速、ST-T改变、导联低电压的发生率均高于适龄组,差异均有统计学意义(P<0.05)。在心电图异常的两组孕妇中,高龄组60例,适龄组21例,高龄组的妊娠丢失率、早产率、新生儿低体质量发生率均略高于适龄组,但两组比较,差异均无统计学意义(P>0.05)。两组孕妇产后异常心电图检出率均低于产前,高龄组ST-T改变的检出率低于产前,差异均有统计学意义(P<0.05)。结论:高龄孕妇多为经产妇,且妊娠晚期易出现心律失常、ST-T等异常心电图改变。临床上需关注高龄孕妇妊娠晚期心电图变化,保证母婴的安全。
【关键词】 高龄孕妇 妊娠晚期 心电图 妊娠结局
[Abstract] Objective: To explore the characteristics of electrocardiogram of elderly pregnant women in the third trimester of pregnancy and provide guidance for clinical practice. Method: A total of 190 pregnant women in the third trimester who underwent electrocardiogram examination in our hospital from January 2017 to June 2019 were selected. They were grouped by age, 95 pregnant women aged ≥35 years old were regarded as the elderly group, 95 pregnant women under the age of 35 were in the age-appropriate group. The results of routine electrocardiogram of pregnant women in the two groups were observed. The two groups of pregnant women with abnormal electrocardiogram and the changes of electrocardiogram before and after delivery were compared. Result: The incidence of abnormal electrocardiogram in the third trimester of pregnancy in the elderly group was 63.16%, higher than 22.11% in the age-appropriate group, and the incidence of arrhythmia, sinus tachycardia, ST-T change and lead low voltage were all higher than those in the age-appropriate group, with statistically significant differences (P<0.05). Among the two groups of pregnant women with abnormal electrocardiogram, there were 60 cases in the elderly group and 21 cases in the age-appropriate group. The pregnancy loss rate, preterm birth rate and neonatal low body mass rate of the elderly group were slightly higher than those of the age-appropriate group, but the differences between the two groups were not statistically significant (P>0.05). The detection rate of abnormal electrocardiogram in both groups were lower than those of before birth, the detection rate of ST-T change in the elderly group was lower than that in the prenatal group, the differences were statistically significant (P<0.05). Conclusion: Elderly pregnant women are mostly transparietal mothers, and abnormal electrocardiogram changes such as arrhythmia and ST-T are easy to occur in the third trimester. Clinical attention should be paid to the changes of electrocardiogram in the third trimester of pregnancy in elderly pregnant women to ensure the safety of mothers and infants.
高龄组孕妇妊娠晚期异常心电图的发生率为63.16%,高于适龄组的22.11%,其中心律失常、窦性心律过速、ST-T改变、导联低电压的发生率均高于适龄组,差异均有统计学意义(P<0.05)。孕妇在妊娠晚期血容量逐渐增加,引起心排血量增多,心脏负荷增大易导致传导系统发生心律失常,以窦性心动过速为主[13]。ST-T改变多因为心脏负荷增加,且自主神经功能紊乱,交感神经张力增高导致耗氧量增多引起[14],本研究两组孕妇ST段都为压低,未发现抬高,表明其大多为慢性心肌缺血,无急性缺血性损伤,此类孕妇可以给予静卧休息,吸氧等处理。导联低电压多因为增大的子宫压迫了下腔静脉,限制了血液的回流,导致下肢甚至全身水肿[15]。高龄组孕妇的心脏代偿功能较适龄组低,且受家庭影响因素多,常出现焦虑、紧张等情绪[16-17],因此以上几种异常心电图的发生率更高。产后3个月,对产前存在异常心电图的产妇进行心電图复查,发现产后两组的异常心电图检出率均低于产前,且高龄组产后ST-T改变的发生率显著低于产前,差异均有统计学意义(P<0.05)。其他类型的异常心电图产后检出率虽也略低于产前,但差异均无统计学意义(P>0.05)。这表明两组孕妇妊娠晚期的一些异常心电活动在产后大多可以恢复,但部分产妇仍存在异常的心电活动,且高龄组的检出率(53.33%)高于适龄组(42.86%),再次暗示高龄产妇的心功能代偿力低于适龄组。而这部分分娩后仍存在异常心电图的妇女因定期复检心电图,预防并及时发现、处理可能出现的心脏病,保障其健康安全。与此同时,本研究发现存在异常心电图的高龄孕妇的妊娠丢失率和早产率虽均高于适龄组,但两组比较,差异均无统计学意义(P>0.05)。表明高龄因素合并心电图异常的孕妇可能会增加其妊娠的风险,高龄孕妇器官老化,心功能代偿能力低,供氧不足,影响胎儿的生长发育,长时间会引起胎儿低体质量、早产,甚至流产等妊娠不良结局[18-19]。且有研究表明,高龄产妇的剖宫产率较适龄产妇高[20]。
因此,临床上需密切关注高龄孕妇的心电图变化,异常心电图者及时配合相应的治疗,提高妊娠质量,避免不良妊娠结局的发生,保证母婴的健康及安全。
参考文献
[1]俞晓敏,古航.高龄孕妇妊娠合并症和并发症临床分析[J].第二军医大学学报,2018,39(2):159-164.
[2]陈芳,陈兰.高龄孕妇妊娠晚期的心电图改变及与妊娠结局的关系[J].中国妇幼保健,2016,31(13):2619-2621.
[3] Francesco R,Sabrina C,Alessandro O,et al.An Advanced Bio-Inspired PhotoPlethysmoGraphy (PPG) and ECG Pattern Recognition System for Medical Assessment[J].Sensors,2018,18(2):405.
[4]许忠宗,陈晨.高龄孕妇妊娠晚期的异常心电图表现及其与不良妊娠结局的关系[J].中国妇幼保健,2019,34(1):53-55.
[5]刘佳,徐阳.女性最佳生育年龄探讨[J].中国妇幼健康研究,2018,29(7):865-868.
[6]管付娟,李银萍.妊娠中晚期互动式干预对改变产妇分娩结局及认知行为的效果分析[J].实用临床医药杂志,2014,18(5):133-134,138.
[7]黎小兰,黄守章,成艳玲.子宫动脉超声多普勒血流监测在晚期高危妊娠孕妇中的价值分析[J].现代医用影像学,2019,28(10):2294-2295,2318.
[8]蓝诗艳,吴丹燕.妊娠晚期子痫前期发生的影响因素及其严重程度与凝血功能指标、血小板参数的相关性分析[J].中国实用医药,2019,14(34):16-18.
[9]刘志伟.超声在妊娠晚期产科出血病因诊断中的应用价值研究[J].系统医学,2019,4(18):115-117.
[10]高志凌,罗早红,谢萍.妊娠合并急性心肌梗死研究进展[J].心血管病学进展,2018,39(2):239-243.
[11]甘莉葵.高龄产妇的妊娠特点及影响安全分娩的因素分析[J].实用妇科内分泌杂志,2016,3(19):139-140.
[12]孙艳君.妊娠晚期合并羊水过少孕产妇与围产儿情况临床分析和护理[J/OL].实用妇科内分泌电子杂志,2019,6(27):144-146.
[13] Balajewicz-Nowak M,Furgala A,Pitynski K,et al.The dynamics of autonomic nervous system activity and hemodynamic changes in pregnant women[J].Neuro Endocrinol Lett,2016,37(1):70-77.
[14]杨芬.孕妇妊娠晚期心电图ST-T改变研究[J].吉林医学,2015,36(17):3884-3885.
[15]迟晔虹,刘晓艳,王雪绒,等.380例中晚期妊娠妇女心电图分析[J].江苏实用心电学杂志,2014,23(1):33-35.
[16]尚南,张华甫,董胜雯.妊娠晚期孕妇心理弹性与焦虑的相关性研究[J].天津护理,2019,27(5):509-513.
[17]孙丽丽,徐萌艳,金珊,等.120例二胎孕妇妊娠晚期压力调查及其影响因素和预防措施分析[J].中国妇幼保健,2019,34(19):4537-4540.
[18] Ntiloudi D,Zegkos T,Bazmpani M A,et al.Pregnancy outcome in women with congenital heart disease: A single-center experience[J].Hellenic J Cardiol,2018,59(3):155-159.
[19]甘丽芬,吴磊.高龄孕妇妊娠晚期心电图改变及其与妊娠结局的关系[J].实用临床医学,2019,20(8):47-49.
[20]张雅莉,刁云云,郝文斌,等.高龄孕妇妊娠期ECG异常对妊娠结局的影响[J].河北医药,2017,39(24):3792-3793,3796.
(收稿日期:2019-12-19) (本文编辑:姬思雨)
