Deceased donor liver transplantation for Budd-Chiari syndrome:Long-segmental thrombosis of the inferior vena cava with extensive collateral circulation
2020-07-07ZiXiLiuJiQiaoZhuJunMaJianTaoKouXianLiangLiQiangHe
Zi-Xi Liu , Ji-Qiao Zhu , Jun Ma, Jian-Tao Kou, Xian-Liang Li, Qiang He
Department of Hepatobiliary and Pancreaticosplenic Surgery, Beijing Chaoyang Hospital, Capital Medical University, No. 8 Gongtinan Road, Chaoyang District, Beijing 10 0 020, China
Budd-Chiari syndrome (BCS) is an infrequent clinical disease resulting from obstruction of the hepatic venous outflow tract anywhere from small hepatic veins to the inferior vena cava(IVC) [1] . Currently, step-wise treatment strategy has been proposed and widely adopted based on the patient’s status, which contains anticoagulation, thrombolysis, percutaneous recanalization, transjugular intrahepatic portosystemic shunt (TIPS) and surgical shunt [2] . It has been reported that up to 10% −20% of BCS patients still develop into liver function failure after the step-wise treatment [3] . Therefore, liver transplantation is the remaining rescue treatment in these patients. The five-year survival rate of BCS patients who underwent liver transplantation can reach as high as 80% [4 , 5] . Notably, very few BCS patients have been reported to have a long-segmental thrombus of IVC. Herein, we presented a patient with total obstruction of the IVC blocked by a longsegmental thrombus, where the common iliac veins and the renal veins were drained into the superior vena cava smoothly through collateral circulation.
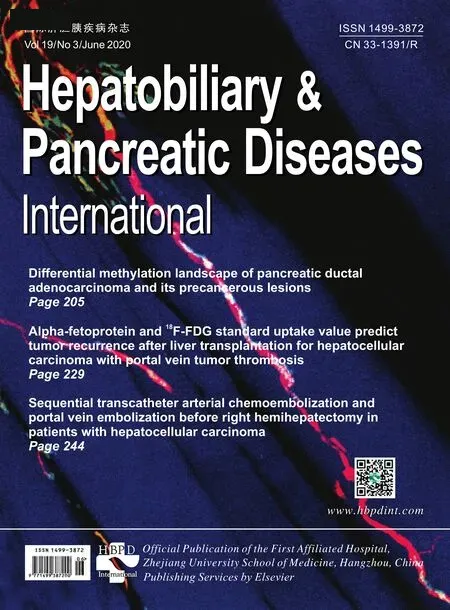
A 26-year-old Chinese male with end-stage liver disease was transferred to our hospital. He complained abdominal pain for 2 months, accompanied with a low fever and poor appetite.He denied any past medical history. Physical examination revealed massive ascites. Laboratory findings revealed: hemoglobin level, 16.8 g/dL; platelet count, 179 0 0 0/mm3; albumin level,3.2 g/dL; alanine aminotransferase (ALT), 514 U/L; aspartate aminotransferase (AST), 500 U/L; total bilirubin level, 105μmol/L; direct bilirubin level, 62μmol/L; international normalized ratio, 2.13;prothrombin activity, 35.8%; and tumor markers and renal function were within normal limits. The MELD score and the Child-Pugh score were 22 and 11, respectively. Abdominal enhanced magnetic resonance imaging (MRI) showed that the IVC was utterly obstructed by a long-segmental thrombus from the suprahepatic IVC to the confluence of the common iliac veins ( Fig. 1 ); the common iliac veins and the renal veins were both drained into the superior vena cava via the varicose azygos-hemi-azygos vein; besides, the right, middle and left hepatic veins were all completely thrombosed. Liver protection therapy, albumin infusion, coagulation regulation therapy, diuresis, and other relevant symptomatic treatments were given to the patient before transferred to our hospital. Unfortunately, the patient’s condition did not get better. As the patient had developed liver failure, and conservative treatment failed, deceased donor liver transplantation (DDLT) was scheduled after hospitalization.
The orthotopic liver transplantation was performed. During the operation, approximately 5 L of ascites and extensive collateral circulation were observed in the abdominal cavity. The thrombosed retrohepatic and suprahepatic IVC was resected together with the liver. Because of the extensive excision of the recipient’s suprahepatic IVC, the donor’s suprahepatic IVC had to be reserved long enough for anastomosis. Besides, the circumferential diaphragm of the recipient’s thoracic IVC was incised to expose the IVC, after that the healthy thoracic IVC was pulled down into the abdominal cavity carefully, and anastomosed with the donor’s suprahepatic IVC directly. The recipient’s distal subhepatic IVC was sutured because there was no blood backflow. The patient’s circulatory system was stable during the operation.
The postoperative course of the patient was uneventful without any complications. According to the pathological result, IVC and hepatic vein stenosis were serious. IVC and hepatic vein thrombosis secondary to congenital vascular stenosis were considered.By the end of the first postoperative month, abdominal enhanced computed tomography (CT) was done, which demonstrated that the common iliac veins and the renal veins were all drained into the superior vena cava via the varicose azygos-hemi-azygos vein smoothly ( Fig. 2 A and B and C); all the anastomotic vessels including the suprahepatic IVC were patent ( Fig. 2 C and D). Abdominal magnetic resonance angiography (MRA) was performed every 6 months to check whether the anastomotic vessels were patent.40 0 0 Axa IU low-molecular-weight heparin calcium was injected subcutaneously once a day for the first 3 weeks after liver transplantation. After that, 100 mg oral aspirin was given per day to prevent venous thrombosis. The laboratory results were all within the normal range during the 2-year follow-up.
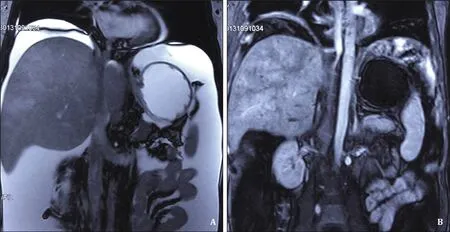
Fig. 1. Preoperative MRI. A: Coronal view. The IVC was totally blocked by a long-segmental thrombus from the suprahepatic IVC to the common iliac vein; B: venous phase.The IVC between the level of the suprahepatic IVC and the common iliac veins was not filled with contrast medium. IVC: inferior vena cava; MRI: magnetic resonance imaging.
Fig. 2. Anterior view of 3-dimensional reconstructed image by MIP of post-transplant CT. A: The right renal vein was drained into the superior vena cava via the varicose azygos-hemi-azygos vein; B: the left renal vein was drained into the superior vena cava through the varicose azygos-hemi-azygos vein; C: the common iliac veins were drained into the superior vena cava via the varicose azygos-hemi-azygos vein. The hepatic veins and the anastomotic portal vein were all patent; D: the anastomotic suprahepatic IVC and the hepatic veins were all patent. MIP: maximum intensity projection; CT: computed tomography.
BCS patients have to undergo liver transplantation due to cirrhosis and liver failure, which results from liver congestion.Congestion is induced by increased sinusoidal pressure, owing to the obstruction of the IVC and/or poor clinical outcomes of the step-wise treatment [6] . Normally, most of BCS patients just have short-segmental or partial obstruction of the IVC. Sun et al. reported that more than 80% of BCS patients have partial and shortsegmental obstruction of the IVC [7] . However, only a small number of BCS patients develop IVC thrombosis. Mentha et al. found that among BCS patients who underwent liver transplantation, less than 17% of patients had an IVC thrombus [5] . Therefore, it is even rarer for BCS patients to have a long-segmental complete thrombosed IVC. According to Karaca’s case series of BCS patients who underwent living donor liver transplantation (LDLT), only 3 patients progressed to complete obstruction of the IVC from the suprahepatic IVC to the renal veins [8] . In our case, the IVC was totally blocked from the suprahepatic IVC to the confluence of the common iliac veins. The venous blood flow from both kidneys and the lower extremities was drained into the superior vena cava via the varicose azygos-hemi-azygos venous system.
In addition, the most difficult challenge is the reconstruction of venous outflow during liver transplantation. Various methods have been described as follows: (1) surgeons may reconstruct venous drainage on the already stenosed and/or thrombosed IVC [8] ; (2)surgeons could prune a widedenovoorifice on the IVC [9] ; (3)cadaveric vessels could be used to reconstruct the IVC [ 9 , 10 ]; (4)in selected patients, the graft’s hepatic vein could be anastomosed to the right atrium directly [11] . As the IVC was totally blocked by a long-segmental thrombus in this patient, we had to remove the thrombosed retrohepatic and suprahepatic IVC simultaneously with the liver. Considering the normal renal function and normal both lower limbs, we ligatured and sutured the subhepatic IVC without changing the patient’s original hemodynamics of lower limbs and kidneys. Postoperative examination showed that the liver transplantation was successful.
In conclusion, the BCS patient’s collateral circulation and the range of venous obstruction should be adequately evaluated before the surgery, when surgeons determine how to reconstruct the blood vessels. Long-term postoperative anticoagulation therapy should be adopted to prevent thrombosis.
CRediT authorship contribution statement
Zi-Xi Liu:Investigation, Writing - original draft.Ji-Qiao Zhu:Investigation, Writing - original draft.Jun Ma:Investigation.Jian-Tao Kou:Investigation.Xian-Liang Li:Investigation.Qiang He:Conceptualization, Investigation, Supervision, Writing - review & editing.
Funding
None.
Ethical approval
The study was approved by the Institutional Review Board of Beijing Chaoyang Hospital. Written informed consent was obtained from the reported patient.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Transjugular intrahepatic portosystemic shunt for a patient with chylothorax in cryptogenic/metabolic cirrhosis
- Sinusoidal obstruction syndrome related to tacrolimus following liver transplantation
- Synergistic interaction between thioredoxin inhibitor 1-methylpropyl 2-imidazolyl disulfide and sorafenib in liver cancer cells
- Laparoscopic combined with thoracoscopic transdiaphragmatic hepatectomy for hepatitis B-related hepatocellular carcinoma located in segment VII or VIII
- Diagnostic value of contrast-enhanced ultrasonography for intrahepatic cholangiocarcinoma with tumor diameter larger than 5 cm
- Effect of six-stitch pancreaticojejunostomy on pancreatic fistula: A propensity score-matched comparative cohort study