Laparoscopic combined with thoracoscopic transdiaphragmatic hepatectomy for hepatitis B-related hepatocellular carcinoma located in segment VII or VIII
2020-07-07YuZhuZhenYuLiChunGuoWngZhePingFngWeiDongJiBioZhng
YuZhu Zhen-Yu Li Chun-Guo Wng Zhe-Ping Fng Wei-Dong Ji F-Bio Zhng ∗
a School of Medicine, Shandong University, Jinan 250012, China
b Division of Liver Surgery, The First Affiliated Hospital of USTC, Division of Life Sciences and Medicine, University of Science and Technology of China, Hefei 230 0 01, China
c Department of Hepatobiliary Surgery, Taizhou Hospital of Zhejiang Province, Wenzhou Medical University, Taizhou 3170 0 0, China
Laparoscopic hepatectomy (LH) is considered a safe and effective method of treating liver cancer because of its relatively low level of trauma, bleeding, pain, and short hospital stay as compared with traditional open surgery [1] . However, this is not ideal for tumors located in segment VII or VIII of the liver as these tumors are difficult to be exposed during laparoscopy, and the conversion rate is relatively high [2] . Although it has been reported that the thoracoscopic transdiaphragmatic segment VII or VIII hepatectomy can obtain better visual field and operation space [3] , it is difficult to control the bleeding of surgical wound. The application is therefore limited. To resolve this problem, we employed a laparoscope to dissect the left hepatic artery, hang over the hepatoduodenal ligament except the left hepatic artery to block liver blood flow and then resect the liver cancer by transdiaphragmatic thoracoscopy.
Six patients with liver tumors located below the diaphragm were selected. All of the patients were male, and two of them had a history of upper abdominal surgery. Primary liver cancer was diagnosed by magnetic resonance imaging (MRI) before the operation, and serum alpha-fetoprotein levels were elevated. All tumors were single and protruded the surface of the liver, and all six patients had histories of chronic hepatitis B and received antihepatitis B virus therapy with entecavir before and after operation. All patients provided their informed consent before the operation.
Take case 1 as an example, first, the patient was placed in a supine position and given general anesthesia, double lumen endotracheal intubation, and left one-lung ventilation. The CO 2 pneumoperitoneum was set up. Under laparoscope television (Karl Storz Endoskope, Tuttlingen, Germany) surveillance, two 5-mm trocars were placed at the xiphoid process and the right medioclavicular line, and one 10-mm trocar was placed at the left medioclavicular line ( Fig. 1 ). Laparoscopic liver surface exploration was performed. The left hepatic artery was dissected under laparoscopy,and the hepatoduodenal ligament was encircled with catheter except the left hepatic artery for inflow occlusion. The two ends of the catheter were elicited from the xiphoid trocar in order to conveniently relieve the obstruction of hepatoduodenal ligament. The location of the tumor was determined by laparoscopy above the diaphragm. Then, we removed the pneumoperitoneum and placed the patient in the left lateral position. A 12-mm incision was made between the sixth ribs of the right posterior axillary line. When the trocar and the thoracoscope were put in place, two additional 12-mm incisions were made in the third ribs of the right anterior axillary line and the eighth ribs of the right middle axillary line, and the operating instruments were placed ( Fig. 1 ). According to the size and position of the tumor, the diaphragm was cut into the abdominal cavity, the hepatoduodenal ligament was blocked using the Pringle method (hepatoduodenal ligament blood flow was opened every 15 min for 5 min), and left hepatic artery blood flow was retained to reduce the impact on the liver function of left lobe. The liver tumor was resected with Harmonic scalpel(Ethicon Endo-Surgery, Cincinnati, OH, USA), the blood vessels and bile ducts were ligated using vascular clamps (Hangzhou Kangji Medical Instrument Co., Ltd., Hangzhou, China), and tumor margin was no less than 1 cm. The mass was removed, and the diaphragm incision was sutured with 3-0 V-Loc (Ethicon, San Angelo, TX, USA). We put the thoracic closed drainage tube in place and closed the abdominal and thoracic incisions ( Fig. 2 ).
The intraoperative and postoperative characteristics of these patients were list in Table 1 . The median operative time for the serial of patients was 140 min (range 120-200). The median intraoperative bleeding was 60 mL (range 30-120). After the operation, flatus time after operation was 2 days (range 2-3), and median postoperative recovery time of serum total bilirubin level was 6 days (range 5-9). Median postoperative hospitalization time was 7 days (range 6-14). There was no gas or exudate in the thoracic cavities of five patients three days after the operation. In the remaining patient,the chest radiograph showed pleural effusion and the effusion was resolved after drainage, and the drainage tube was removed before discharge. All six cases were diagnosed with hepatocellular carcinoma by pathology. The median follow-up was 10 mon (range 4-26), and all the patients were in good health, with no tumor recurrence or metastasis during follow-up.

Fig. 1. Port positions and location of trocar: supine position ( A ) and left lateral position ( B ).

Table 1 The characteristics of six patients.
Liver masses located under the diaphragm are difficult to be exposed, although the liver segment can be disconnected from the right hepatorenal ligament, right hepatic triangular ligament, and right coronary ligament, and to fully separate the right liver to better expose it for hepatectomy. Chiow et al. [4] and Ogiso et al. [5]reported laparoscopic transabdominal with transdiaphragmatic access to resect posterosuperior liver lesions. However, the approach also requires trocar to enter the abdominal cavity through the diaphragm, which also has some trauma to the diaphragm and destroys part of the blood supply of the liver, thereby affecting the recovery of liver function after the operation [6] . Our approach may provide a better visual field after diaphragm incision, even without the need for free liver, which ensured a better blood supply of the liver. Among the six patients, there were no postoperative complications except pleural effusion in one case, indicating that the operation was safe. The recurrence of hepatocellular carcinoma is 50%-75% of patients after hepatectomy [7] . Some patients with recurrence of hepatocellular carcinoma may undergo secondary surgery. These patients may have abdominal adhesions which make the traditional laparoscopic surgery difficult, and the thoracoscopic transdiaphragmatic approach provides another surgical access. However, thoracoscopy alone cannot block blood flow from the hepatic portal. Thus, we used laparoscopy to block the hepatoduodenal ligament, which can compensate for the inability of thoracoscopy to control blood flow from the liver. In these 6 cases, we preserved left hepatic artery blood flow during liver dissection in order to protect the liver function of the left lobe.The transdiaphragmatic approach does not require the separation of right liver and thus, the blood flow, the right hepatic triangular ligament and the right coronary ligament were preserved. In China,most patients with liver cancer have hepatitis B infection and liver cirrhosis [8] , and the control of intraoperative bleeding and the recovery of postoperative liver function are of great significance to the rehabilitation of patients after operation [9] . Moreover, it is feasible to use laparoscopy to assess the abdominal cavity and to exclude the possibility of tumor metastasis. If the patient also has pulmonary oligo-metastases, then this technique can complete the resection of liver cancer and lung metastases simultaneously.
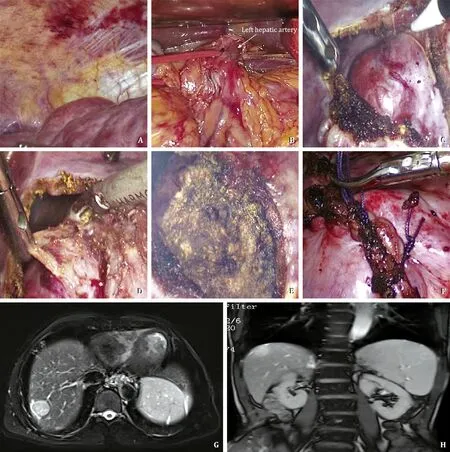
Fig. 2. Surgical procedure and image data. A : Laparoscopic liver surface exploration was performed; B : The left hepatic artery was dissected under laparoscopy; C : The diaphragm was cut into the abdominal cavity; D : The liver tumor was resected with an ultrasonic knife; E : The tumor was removed; F : The diaphragm incision was sutured;G and H : The location of tumor in magnetic resonance imaging.
There are several limitations of this technique. Due to the unilateral pulmonary ventilation during the operation, the operation cannot be performed if the patient is unable to tolerate the unilateral lung ventilation or has a history of the right thoracic operation.
This technique can be implemented in patients with 3-5 cm subphrenic tumors that are prominent on the surface of the liver,with large vessels adjacent to the liver but not close to the right hepatic vein or inferior vena cava. We hope that with the development of endoscopic technology and accumulation of surgical experience, this technique will be applicable to more patients.
Acknowledgments
We thank Dr. Xiao-Dong Zhu from Shanghai Zhongshan Hospital for his guidance on article writing.
CRediT authorship contribution statement
Yu Zhu:Data curation, Funding acquisition, Writing - original draft.Zhen-Yu Li:Data curation, Methodology.Chun-Guo Wang:Methodology.Zhe-Ping Fang:Methodology.Wei-Dong Jia:Writing - review & editing.Fa-Biao Zhang:Conceptualization, Writing -review & editing.
Funding
This study was supported by a grant from Taizhou Science and Technology Plan Project (1701KY05).
Ethical approval
This study was approved by the Ethics Committee of Taizhou Hospital of Zhejiang Province (X20151204).
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Transjugular intrahepatic portosystemic shunt for a patient with chylothorax in cryptogenic/metabolic cirrhosis
- Differential methylation landscape of pancreatic ductal adenocarcinoma and its precancerous lesions
- Hepatobiliary&Pancreatic Diseases International
- MicroRNAs and long non-coding RNAs in liver surgery: Diagnostic and therapeutic merits
- Alpha-fetoprotein and 18 F-FDG standard uptake value predict tumor recurrence after liver transplantation for hepatocellular carcinoma with portal vein tumor thrombosis: Preliminary experience
- Translationally controlled tumor protein exerts a proinflammatory role in acute rejection after liver transplantation