Effect of six-stitch pancreaticojejunostomy on pancreatic fistula: A propensity score-matched comparative cohort study
2020-07-07ZhaoLinZengYanSunDaXuePiLiLiuWangMingChenLeiZhang
Zhao-Lin Zeng, Yan Sun, Da Xue, Pi-Li Liu, Wang-Ming Chen, Lei Zhang
Department of General Surgery, the Second Affiliated Hospital of Harbin Medical University, Harbin 150086, China
Keywords:Duct-to-mucosa Pancreaticoduodenectomy Pancreaticojejunostomy Clinically relevant postoperative pancreatic fistula
A B S T R A C T Background: Clinically relevant postoperative pancreatic fistula (CR-POPF) is the most common and severe complication after pancreaticoduodenectomy (PD). Despite the development of numerous anastomotic surgical techniques to minimize CR-POPF, more than 30% of patients who undergo PD develop CR-POPF.Herein, we propose a novel pancreaticojejunostomy (PJ) technique and evaluate its efficacy and safety compared to traditional PJ.Methods: This retrospective study enrolled 164 consecutive patients who underwent PJ after PD between January 2012 and June 2017. Of them, 78 (47.6%) underwent traditional PJ and 86 (52.4%) underwent sixstitch PJ. The primary outcome was CR-POPF at 1-month follow-up defined according to the revised 2016 International Study Group on Pancreatic Fistula definition. To adjust for baseline differences and selection bias, patients were matched by propensity scores, which left 63 patients with traditional PJ and 63 with six-stitch PJ.Results: Compared to patients who underwent traditional PJ (mean age 56.2 ±9.4 years), patients who underwent six-stitch PJ (mean age 57.4 ±11.4 years) had a lower CR-POPF rate. The risk of CR-POPF among patients who underwent six-stitch PJ was decreased by 81.7% after adjustment for age, sex, body mass index, and disease severity compared to patients who underwent traditional PJ. Additionally, the surgery time was reduced from 29 min for traditional PJ to 15 min for six-stitch PJ ( P < 0.001). Adverse effects such as abdominal fluid collection, abdominal bleeding, and wound infection were similar between two groups.Conclusion: Six-stitch PJ may be an effective and efficient PJ technique for patients who undergo PD surgery.
Introduction
Pancreaticoduodenectomy (PD) is the most commonly performed surgery to remove benign and malignant lesions, in regions like head of the pancreas, duodenum, periampullary region, or the distal common bile duct. Although mortality associated with this surgery has decreased to<5% at major pancreatic centers in recent years [1 , 2] , nearly 30% −50% of patients experience significant postoperative morbidity [3 , 4] . Postoperative pancreatic fistula (POPF) is the most common complication after PD, often leading to other serious complications, such as delayed gastric emptying (DGE), intraabdominal infection, hemorrhage, or even death [5 , 6] . Currently,despite the numerous anastomosis techniques that have been developed in an attempt to minimize POPF, the optimal method remains up for debate [7] .
In 2015, we first proposed a novel pancreaticojejunostomy (PJ)technique called sealing PJ [8] , which is performed in combination with a ductal parenchyma to mucosal-seromuscular singlelayer anastomosis; thus, we named it the “six-stitch anastomosis”PJ (six-stitch PJ). The underlying principle is based on the fact that the pancreas is a hollow organ with a very tiny pancreatic duct cavity and very thick wall of pancreatic parenchyma. A connection between the pancreas and the intestine can be performed by creating an anastomosis between the two hollow organs. This technique is primarily a modification of conventional duct-to-mucosa anastomosis. Our preliminary study showed that six-stitch PJ provided good clinical outcomes with decreased POPF rates [8] , but there is a lack of comparative population evidence to evaluate its ability to decrease POPF rates. Therefore, we retrospectively summarized the clinical data from a single surgeon and compared the short-term postoperative outcomes of traditional PJ versus six-stitch PJ.
Methods
Patientsandstudydesign
We collected the data of 164 newly diagnosed patients aged between 16-83 years [64 (39%) women] who underwent PD in the Second Affiliated Hospital of Harbin Medical University between January 2012 and June 2017. None of the patients had received any other treatments before the surgery. Among them, 78 patients underwent traditional PJ between January 2012 and December 2014,while 86 underwent six-stitch PJ between January 2015 and June 2017.
We collected the clinical data of preoperative, intraoperative,and postoperative variables. The preoperative characteristics included age, sex, smoking history, alcohol use history, body mass index (BMI), history of type 2 diabetes mellitus, disease severity according to American Society of Anesthesiologists Physical Status Classification Scores (ASA scores 1-6: normal healthy patient,mild systemic disease, severe systemic disease. Severe systemic disease is a constant threat to life, moribund patient who is not expected to survive without the operation, brain-dead patient) [9] ,history of biliary drainage, and laboratory examinations (serum aspartate aminotransferase, alanine aminotransferase, total bilirubin,hemoglobin, albumin, and international normalized ratio). The intraoperative parameters included pancreatic texture (soft or hard)judged by surgeons, pancreatic duct diameter (mm), intraoperative blood loss volume, intraoperative blood transfusion, total operative time, presence of combined vascular resection and reconstruction,and PJ time. We also collected information about postoperative pathological findings, postoperative hospital stays, exhaust time, 1-month reoperation rate, morbidity of clinically relevant postoperative pancreatic fistula (CR-POPF), and mortality.
The primary outcome, CR-POPF, was defined and graded 1-month after surgery according to the 2016 International Study Group for Pancreatic Fistula criteria [10] . In this study, we focused on only grade B and C pancreatic fistula considering their clinical significance, while a biochemical leak (i.e. grade A) was considered no CR-POPF owing to its lack of clinical impact on outcomes.Secondary outcomes included other postoperative complications during 30 days after surgery including PJ anastomosis duration,time to first flatus, postoperative hospital stay, mortality, reoperation rate, overall complications, DGE, biliary fistula, abdominal fluid collection, abdominal bleeding, and wound infection.

Fig. 1. Schematic diagram of traditional pancreaticojejunostomy. A: posterior outer-layer suture; B: posterior inner-layer suture; C: anterior inner-layer suture; D: anterior outer-layer suture.
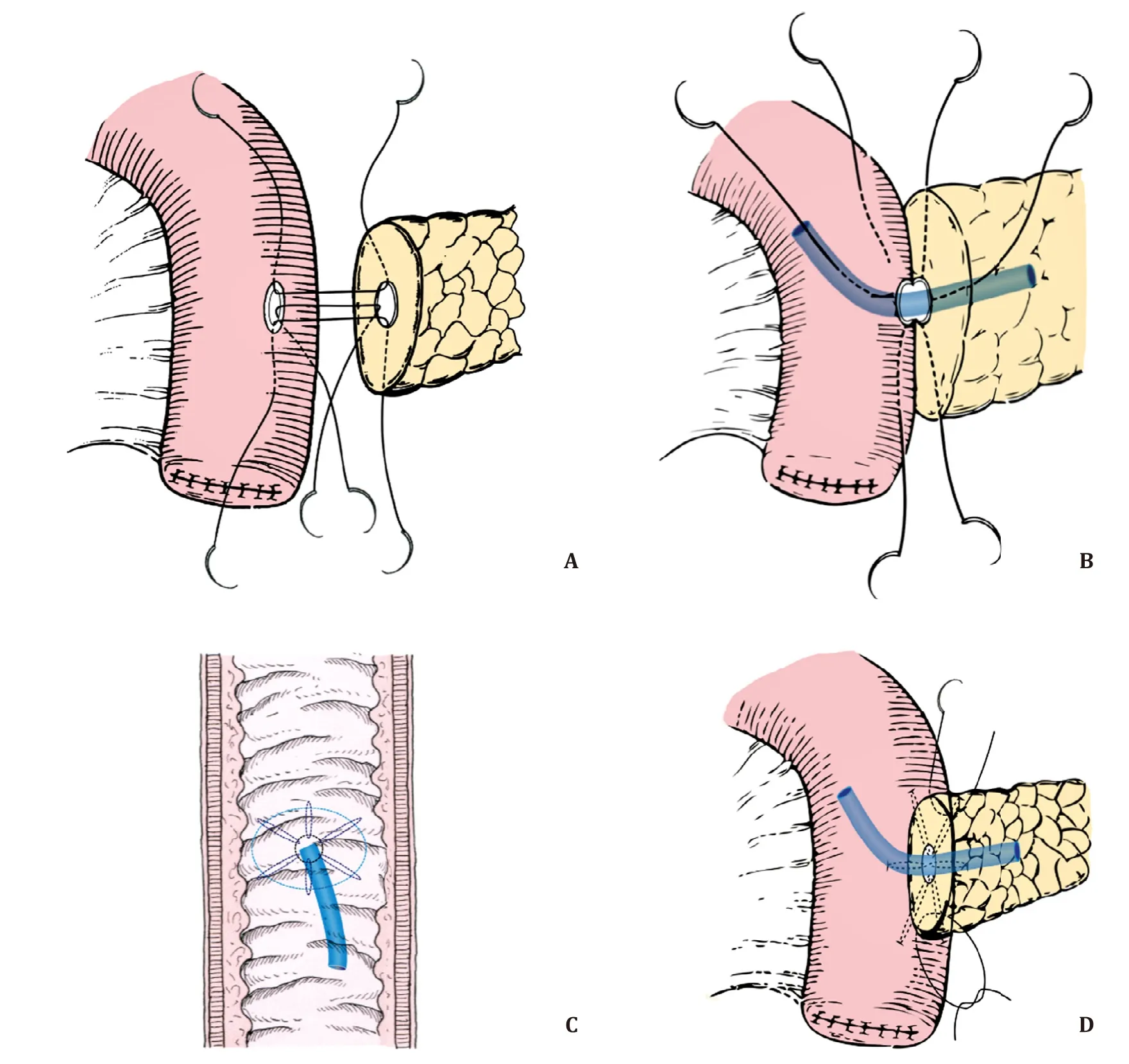
Fig. 2. Schematic diagram of six-stitch pancreaticojejunostomy. A: posterior layer suture with 3 interrupted sutures; B: anterior layer suture with 3 interrupted sutures; C:interior view of anastomosis in the intestinal cavity; D: upper and lower parts of the anastomosis are reinforced.
StandardPDprocedure
Each patient underwent standard PD according to the Chinese Society of Clinical Oncology guideline, which is similar to that of the American Society of Clinical Oncology clinical practice guideline [11] . Briefly, the lesions of the pancreatic head, distal bile duct, duodenum, distal stomach, and proximal intestine were resectedenbloc. When the pancreatic head could not be isolated from the portal or superior mesenteric veins, wedge or segment resections and vascular reconstructions were performed. Digestive reconstruction was performed as follows: end-to-side PJ, end-toside choledochojejunostomy, and side-to-side gastrojejunostomy.These anastomoses were executed in a single lifting jejunal loop.A stent was routinely inserted into the pancreatic duct for internal drainage, provided that the pancreatic duct could be identified. And two soft silicone drains were placed behind the PJ and the biliary-jejunal anastomosis (drainage 1) and in front of the PJ(drainage 2).
TraditionalPJprocedure
The traditional PJ was conducted as previously described [12] .Briefly, invagination anastomosis was performed in two layers.The sequence of anastomosis was as follows: outer posterior layer → inner posterior layer → inner anterior layer → outer anterior layer. The pancreatic remnant was buried in the jejunum, and anastomosis was completed using a continuous 4-0 absorbable monofilament suture ( Fig. 1 ).
Six-stitchPJprocedure
Six-stitch PJ was performed according to the standard protocol as described previously [8] . A small hole was created in the jejunum at the level of the pancreatic duct. The six-stitch anastomosis was carried out in a single layer. The six-stitch PJ was completed with interrupted 4-0 sutures passing through the pancreatic duct parenchyma and serosal mucosa of the jejunum. A total of 6 sutures were placed in the posterior and anterior walls at intervals of 60 °per pin, so the section of the pancreas was tightly attached to the serosa of the jejunum ( Fig. 2 ).
Standardperioperativetreatmentandnursing
The standard management was administered during the entire perioperative period. Each patient underwent routine preoperative laboratory and radiographic examinations. If the total bilirubin level exceeded 300μmol/L, we usually performed percutaneous transhepatic cholangial drainage to alleviate the jaundice.
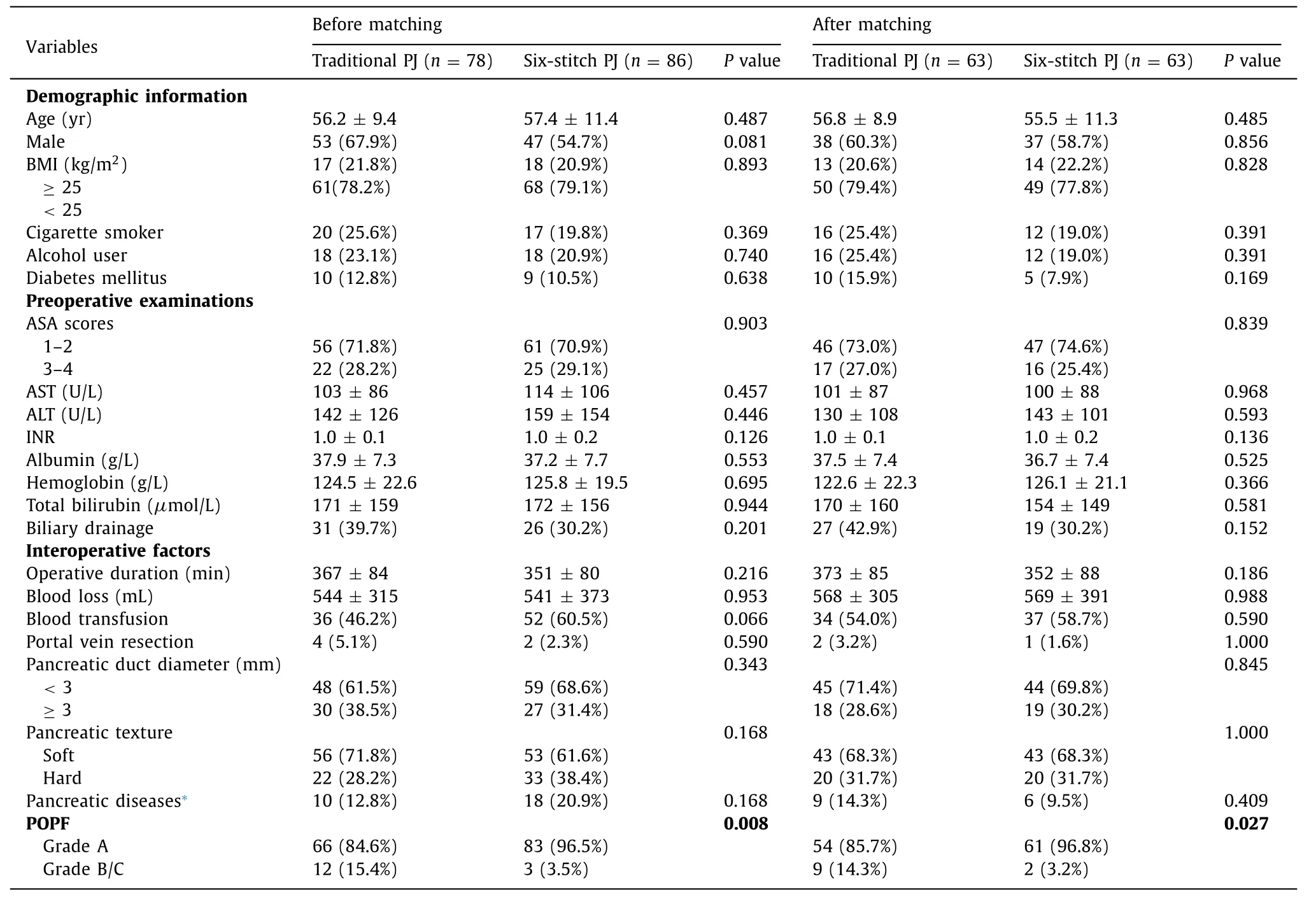
Table 1 Preoperative and intraoperative characteristics among 164 patients before and 63 paired patients after matching.
Within the first 72 h after surgery, patients were routinely given broad-spectrum antibiotics, acid-suppressing drugs, and total parenteral nutrition. Gastrointestinal decompression tubes were evacuated after the patients passed flatus. Amylase concentrations were measured on postoperative days 1, 3, and 5 as well as at subsequent time points if necessary. A computed tomography scan was performed if an intraabdominal fluid collection or possible infection was suspected. If there was no sign of POPF or other abdominal complications and the drainage fluid was<50 ml/d for two consecutive days, the peritoneal drainage tube would be removed. If POPF or other factors caused peritoneal fluid accumulation, ultrasound-guided percutaneous drainage was performed.Patients with DGE were treated with continuous gastrointestinal decompression and nutritional support. If bleeding was detected,selective intra-arterial digital subtraction angiography embolization or hemostasis by reoperation was performed according to hemorrhage severity.
Statisticalanalyses
We calculated the mean ± standard deviation, median (interquartile range), or count (percentage), whenever appropriate, for preoperative characteristics among patients who underwent traditional PJ and six-stitch PJ, which were compared using thet-test or Chi-square test, respectively. To better evaluate the effects of the PJ technique on the occurrence of CR-POPF and reduce any potential selection bias and confounding factors, nearest-neighbor 1:1 matching with a caliper size of 0.03 standard deviations of the logit of the propensity score was performed between the sixstitch PJ and traditional PJ groups. We used logistic regression of sex, age, ASA score, BMI, transfusion, pancreatic duct size, pancreatic texture, and pathological diagnosis to construct the propensity score for matching patients who underwent traditional PJ or six-stitch PJ. Using propensity score matching, 63 paired patients who underwent traditional PJ or six-stitch PJ were matched and included in the analyses. For the matched data analyses, we used the pairedt-test for continuous variables, McNemar’s test for binominal variables, and conditional logistic regression models for categorical variables to evaluate difference in CR-POPF and other postoperative complications between patients who underwent traditional PJ and those who underwent six-stitch PJ.
All statistical analyses were performed using Statistical Product and Service Solutions (SPSS) version 25.0 software (SPSS Inc., IBM,Armonk, NY, USA). All statistical tests were two-sided, and values ofP<0.05 were considered statistically significant.
Results
Patients’characteristics
A total of 78 patients (mean age 56.2 ± 9.4 years; 32.1%women) underwent traditional PJ and 86 patients (mean age 57.4 ±11.4 years; 45.3% women) underwent six-stitch PJ ( Table 1 ).After propensity score matching of the variables listed in Table 1 ,63 pairs of patients were included into our analyses. Most of the demographic characteristics, preoperative examinations, andinteroperative factors were comparable between traditional PJ patients and six-stitch PJ patients (P>0.05 for all).
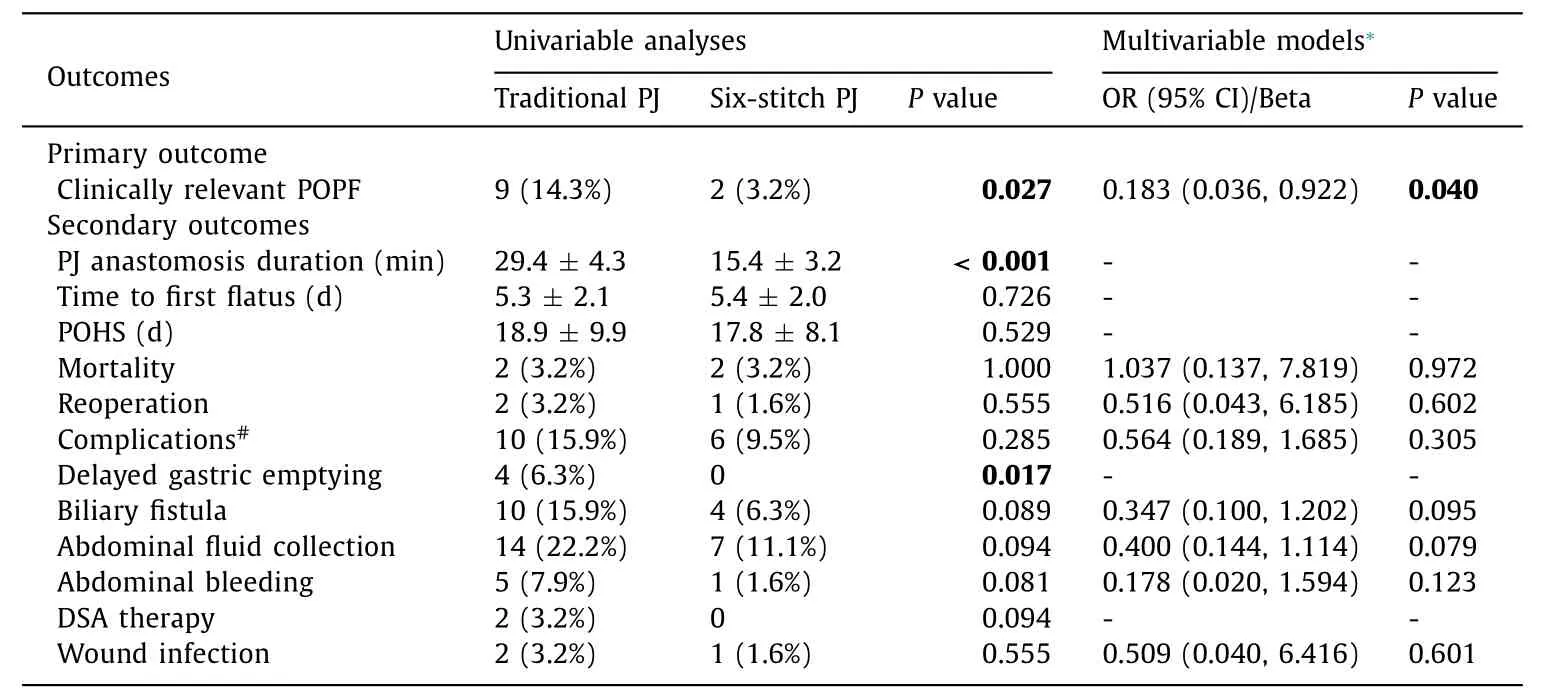
Table 2 The ORs (95% CIs) of six-stitch PJ vs. traditional PJ for clinically relevant POPF and secondary outcomes in 63 paired patients.
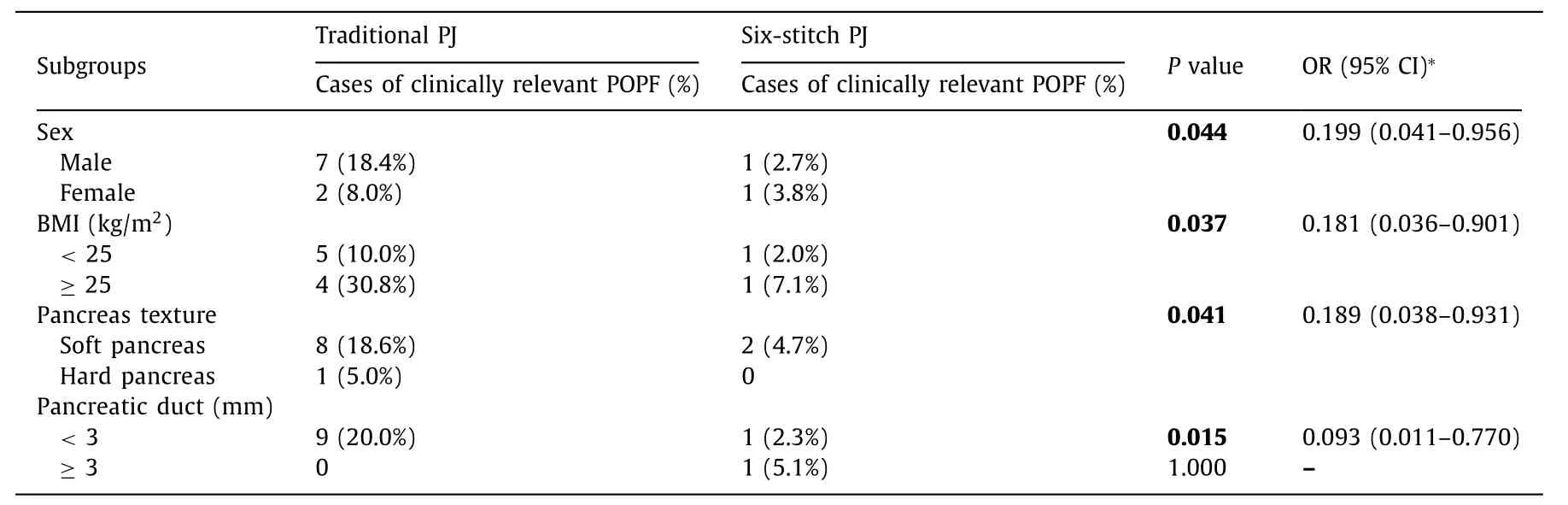
Table 3 The ORs (95% CIs) of six-stitch PJ vs. traditional PJ for clinically relevant POPF in subgroups.
CR-POPFrateandsecondaryoutcomes
Among the 63 paired patients, a total of 2 (3.2%) patients who underwent six-stitch PJ developed the CR-POPF, while 9(14.3%) patients who underwent traditional PJ experienced CRPOPF after 1-month of follow-up (P= 0.027). We further adjusted for age, sex, BMI, and disease severity and found that,compared with traditional PJ surgery, six-stitch PJ surgery significantly decreased the risk of CR-POPF by 81.7% [odds ratio(OR): 0.183; 95% confidence interval (CI): 0.036-0.922;P= 0.040]( Table 2 ).
We also observed that the mean duration for six-stitch PJ was 14 min shorter than that of traditional PJ (P<0.001); the anastomosis PJ times were 15.4 ±3.2 min for six-stitch PJ and 29.4 ±4.3 min for traditional PJ. DGE rate was lower in six-stitch PJ than in PJ (0 vs. 6.3%,P= 0.017). We also found lower rates of reoperation, biliary fistula, complications, postoperative hospital stays, abdominal fluid collection, abdominal bleeding, and wound infections in patients with traditional PJ compared with patients with six-stitch PJ, although the differences were insignificant. Also,the mortality and the time to first flatus for patients who underwent six-stitch PJ were similar to those of patients who underwent traditional PJ (P>0.05 for both).
Subgroupanalyses
The subgroup analyses by sex, BMI, pancreas texture, and pancreatic duct showed that the anastomosis method was related to the risk of CR-POPF ( Table 3 ). We found that a consistent protection of six-stitch PJ from CR-POPF among patients regardless of sex(OR: 0.199; 95% CI: 0.041-0.956), BMI (OR: 0.181; 95% CI: 0.036-0.901), and texture of pancreas (OR: 0.189; 95% CI: 0.038-0.931).For the pancreas with pancreatic duct<3 mm, six-stitch PJ also played a protective role (OR: 0.093; 95% CI: 0.011-0.770).
Discussion
The present study demonstrated that six-stitch PJ was better suited for CR-POPF and had a short PJ anastomosis time. Six-stitch PJ surgery had a similar time to first flatus, postoperative hospital stays, and mortality, reoperation, overall complications, biliary fistula, abdominal fluid collection, abdominal bleeding, and wound infections.
In our study, we routinely inserted a plastic tube into the pancreatic duct to provide internal drainage in both groups of patients.In addition to providing partial drainage of pancreatic juice and preventing accidental pancreatic duct closure, stenting guides the intestinal mucosal epithelial cells to move toward the pancreatic duct and promote anastomosis healing [13] . As a modified ductto-mucosa anastomosis technique, six-stitch anastomosis exhibits an advantage of traditional duct-to-mucosa anastomosis that can achieve an accurate PJ anastomosis; moreover, this single-layer suture minimizes the suture layer of PJ and prevents pancreatic leakage caused by a large numbers of needle sutures. A six-stitch suture with 60-degree intervals provides uniform stress, which effectively prevents tears in anastomosis due to a tiny pancreatic duct,leading to PJ failure. Thus, six-stitch PJ is appropriate for both softand hard-textured pancreatic tissues, whereas the traditional ductto-mucosa PJ technique might be more applicable in cases of dilated pancreatic ducts and hard-textured pancreatic tissues [14] .
The traditional invagination anastomosis is simple and easy to perform; however, the cut end of the pancreas is directly exposed to the intestinal cavity, and the intestinal fluid is able to activate the pancreatic enzymes, resulting in bleeding and scar contracture [15] . Six-stitch anastomosis effectively prevents direct contact between the pancreatic section and the irritating intestinal contents, and enables the serosa of the small intestine to cover the surface of the pancreas and achieve fast healing. Moreover,compared with invagination anastomosis, six-stitch anastomosis significantly reduces the occurrence of POPF after PD, especially in cases of CR-POPF (grades B and C); this PJ method is easy to perform and can greatly shorten the PJ time. The total reconstruction requires half the surgery time of traditional PJ, which decreases the risk of intraoperative bleeding, infections, and other long-term surgery-related complications.
Our data showed a 3.5% (3/86) CR-POPF rate of six-stitch anastomosis. This is consistent with those of other studies of the modified duct-to-mucosa anastomosis technique. Grobmyer et al. reported that modified Blumgart anastomosis, a variation of the duct-to-mucosa anastomosis, can lead to an overall POPF rate of 20.3%; only 6.9% of these cases were clinically related [16] .Kleespies and colleagues found a significantly decreased leakage rate after Blumgart anastomosis, which prompted them to discontinue using the traditional duct-to-mucosa anastomosis technique(4% vs. 13%) [17] . Miao also revealed that single-layer anastomosis was associated with an overall POPF rate of 13.5% and a grade B/C rate of 7.7% [18] .
Pancreaticoenteric anastomosis is often considered a key procedure during PD, which ensures normal postoperative function of the pancreas and intestine and plays a critical role in the development of CR-POPF. Invagination and duct-to-mucosa methods are the two most commonly used anastomosis techniques. Despite a variety of recent improvements in these surgical techniques,their quality remains unsatisfactory. Besides the pure technical factors, various potential factors including age, obesity, nutritional status, tumor type, pancreatic texture, pancreatic duct size, duration of operation, and intraoperative bleeding would directly and indirectly affect the risk of CR-POPF [19-22] . Obese or overweight patients with intraabdominal obesity and fat volume in the pancreas [23] are at high risk of developing CR-POPF [24-27] . The high risk of CR-POPF after PD among obese and overweight patients occurs mainly because of the difficulty of abdominal surgery in obese patients due to anatomical challenges, the softer pancreatic texture of obese patients [28] , and difficulty with anastomosis due to severe fatty infiltration; obesity decreases the pancreatic healing capacity and increases the risk of pancreatic fistula [29] . Similarily,we also found differences in the risk of developing CR-POPF among patients with a high versus low BMI.
Previous evidence suggested that pancreatic duct size and pancreatic texture contributed to CR-POPF [22 , 30] , which was also supported by our findings. In contrast to pancreases with wide ducts, soft pancreases often have small pancreatic ducts and vigorous exocrine function [31] . This makes the pancreas more susceptible to injury and increases pancreatic juice output. Upon assessing the risk factors of CR-POPF, researchers generally consider the specific pancreatic pathology and intraoperative blood loss [20] . However, we did not detect a significant influence of specific pathologies on the risk of CR-POPF.
Our study has several limitations. First, it was retrospective in nature; therefore, bias is inherent. Second, the six-stitch procedures were performed 3 years after the invagination PJ procedures,and the surgeons had gained more experience and expertise during this period. Thus, we cannot rule out the possibility that surgeon experience might impact the outcomes. However, the single surgeon involved in the present study was proficient and had more than 10 years’ experience with traditional PJ. Thus, although the influence of surgeon-related factors existed, it did not play a key role in this study. Finally, there was no long-term follow-up, and we compared only the six-stitch and invagination techniques.
In conclusion, the present study showed that six-stitch PJ is superior to traditional PJ surgery in reducing the risk of CR-POPF after PD. Also, the six-stitch surgical anastomosis technique was time-saving and featured similar or fewer postoperative complications and infections. Further well-designed large-scale randomized controlled studies are warranted to reconfirm the efficacy and safety of six-stitch PJ.
CRediT authorship contribution statement
Zhao-Lin Zeng:Formal analysis, Writing - original draft.Yan Sun:Formal analysis, Writing - original draft.Da Xue:Data curation. Pi-Li Liu: Data curation.Wang-Ming Chen:Data curation.Lei Zhang:Conceptualization, Formal analysis, Funding acquisition,Writing - original draft.
Funding
This study was supported by a grant from the National Natural Science Foundation of China ( 81571553 ).
Ethical approval
This study was approved by the Ethics Committee of the Second Affiliated Hospital of Harbin Medical University, and it followed the ethical guidelines of the 1975DeclarationofHelsinki. Each participant provided written informed consent.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Transjugular intrahepatic portosystemic shunt for a patient with chylothorax in cryptogenic/metabolic cirrhosis
- Sinusoidal obstruction syndrome related to tacrolimus following liver transplantation
- Synergistic interaction between thioredoxin inhibitor 1-methylpropyl 2-imidazolyl disulfide and sorafenib in liver cancer cells
- Laparoscopic combined with thoracoscopic transdiaphragmatic hepatectomy for hepatitis B-related hepatocellular carcinoma located in segment VII or VIII
- Deceased donor liver transplantation for Budd-Chiari syndrome:Long-segmental thrombosis of the inferior vena cava with extensive collateral circulation
- Diagnostic value of contrast-enhanced ultrasonography for intrahepatic cholangiocarcinoma with tumor diameter larger than 5 cm