Lifesaving transarterial embolization using absorbable gelatin sponge particles for massive bleeding of ruptured metastatic hepatic melanoma
2020-05-10PngiotisLinsGiorgiAmyRoGeorgeRfekMueMillereuxCrmelisDmmroPierreTrouillerSophieMitreIrhimDgher
Pngiotis Lins Giorgi Amy Ro George Rfek Mue Millereux Crmelis Dmmro Pierre Trouiller Sophie Mitre Irhim Dgher
a Department of Minimally Invasive Digestive Surgery, Antoine-Beclere Hospital, AP-HP, Clamart F-92140, France
b Paris-Saclay University, Orsay F-91405, France
c Department of Radiology, Antoine-Beclere Hospital, AP-HP, Clamart F-92140, France
d Department of Intensive Care Unit, Antoine-Beclere Hospital, AP-HP, Clamart F-92140, France
TotheEditor:
Melanoma is an aggressive malignant tumor that arises from melanocytic cells. It usually originates from the epithelial tissues of the skin, retina and anorectal canal. Melanoma is characterized by early metastases, even from thin primary tumors. The most common sites of distant metastasis are: skin, lung, brain, liver,bone and intestine. Liver involvement occurs in 14% to 20% of cases [1] , but the diagnosis is usually performed incidentally on imaging studies, since these lesions are seldom symptomatic.Rarely, metastatic hepatic melanoma can manifest as an acute condition of massive bleeding due to spontaneous rupture of one or more hepatic lesions, with disastrous outcomes for patients in most cases. In the current literature, very few cases of spontaneous rupture of metastatic hepatic melanoma have been reported, all with fatal outcomes [2-5] . Indeed, when such a condition occurs,prompt management and bleeding control strategies are essential for long-term survival of these patients.
Transarterial embolization (TAE) has become a valuable tool in the arsenal for bleeding control in cases of spontaneous ruptured metastatic tumors. In the current literature, non-absorbable embolizing agents such as polyvinyl alcohol (PVA) particles,cyanoacrylate glue and coils [6] , and more rarely absorbable embolizing agents such as gelatin sponge particles [4 , 5] have been used towards this purpose, with immediate post-TAE fatal outcomes for patients in most cases and extremely poor oncological outcomes in the remaining cases. In our hospital, we frequently use absorbable gelatin sponge (particles or powder form) for TAE in cases of vascular bleeding, with good results. However, we have been reluctant to use this embolizing agent for TAE in the context of massive hepatic bleeding. Furthermore, in the literature,there is only one case of TAE for ruptured hepatic metastatic melanoma, reporting a fatal patient outcome. Herein we reported an unusual case of a 32-year-old woman with massive bleeding due to ruptured hepatic metastases from cutaneous melanoma.The bleeding was successfully controlled by TAE with absorbable gelatin sponge particles.
A 32-year-old Caucasian woman presented to our Emergency Department with diffuse abdominal pain, vomit, altered consciousness and signs of hypotension. At physical examination, she was pale with diffuse abdominal tenderness. Three subcutaneous nodules were palpated on physical examination on presternal, right inguinal and left iliac fossa localizations. Vital signs were: blood pressure (BP) 82/45 mmHg, heart rate (HR) 131 bpm, temperature 36.5 °C and respiratory rate 17 per minute. Admission laboratory tests showed: hemoglobin (Hb) of 6.4 mg/dL, platelet count 160 ×109/L, prothrombin time (PT) 40%, aspartate aminotransferase (AST) 521 U/L, alanine aminotransferase (ALT) 334 U/L andγ-glutamyl transpeptidase (γ-GTP) 38 U/L. Abdominal contrastenhanced CT scan revealed multiple voluminous liver masses.There were two ruptured masses, one (65 mm) was between segments VI and VII and one (77 mm) in segment VII. The bleeding was active and there was a massive hemoperitoneum. The splenomesenteric trunk was completely blocked by thrombosis( Fig. 1 ). An informed consent was obtained from the patient prior to any other procedure. The patient was intubated and received an initial transfusion of 3 units of packed red blood cells and 1 unit of fresh frozen plasma.
Emergency TAE was performed by selective occlusion of the right hepatic artery with absorbable gelatin sponge particles(GelitasponR○, Gelitamedical, Eberbach, Germany) ( Fig. 2 ). Briefly,under general anesthesia, the patient was placed in a supine position. Under ultrasound and fluoroscopic control, a shepherd catheter was introduced through a femoral puncture. A celiac trunk arteriography was performed, showing diffuse irregular hypervascular lesions involving the right lobe with several foci of extravasation of contrast. The right hepatic artery was occluded using absorbable gelatin sponge particles injected through a 2.7 French catheter. Final control arteriography showed good contrast medium stagnation and absence of active bleeding. At the end of the procedure, the patient was hemodynamically stable, and a check angiogram showed successful embolization with no contrast leak.

Fig. 1. A: Contrast-enhanced abdominal computed tomography scan revealing enlarged metastatic nodules in the right liver with active bleeding in one of them (arrow);B: Thrombosis of the splenomesenteric trunk (arrow).
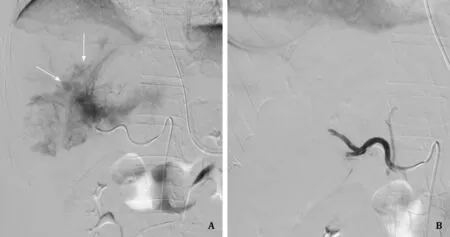
Fig. 2. A: Hepatic arteriography showing diffuse hypervascular lesions in the right hepatic lobe with several foci of contrast medium extravasation (arrows); B: Complete occlusion of the right hepatic artery after embolization with absorbable gelatin sponge particles.
Immediately after emergency TAE, the patient was hemodynamically stable and vital signs stabilized. Control abdominal CT scan showed no signs of active bleeding. Two days after TAE, the patient underwent laparoscopic peritoneal lavage and aspiration of 3 liters of residual hemoperitoneum. The presternal subcutaneous nodule was resected. Histology of this nodule revealed a BRAF V600E mutant metastatic melanoma. Brain, thoraco-abdominal and pelvic CT scans 4 days after TAE revealed: absence of brain metastasis; two pulmonary metastases; multiple bilobar hepatic metastases; partial tumoral thrombosis of the portal vein, the superior mesenteric vein and the splenic vein; enlarged lymph nodes in contact with a mass (probably carcinomatosis) at the splenic hilum. The patient initiated emergency treatment by immunotherapy with dabrafenib-trametinib 4 days after TAE. The postoperative course was marked by septicemia that was successfully treated with antibiotic therapy. The patient was discharged from our department after 18 days. Splenomesenteric and portal thrombosis were successfully treated by curative doses of low molecular weight heparin for a period of 3 months.
After 7 months of first-line treatment with dabrafenibtrametinib, a metabolic response in the lungs and abdomen was present but cerebral progression was noted with 3 metastatic lesions found on control CT-scan. Second-line treatment with ipilimumab and nivolumab was inititated (4 sessions, only nivolumab after every month) and stereotaxic radiotherapy of the three cerebral lesions was performed. The metastases of cerebral, pulmonary and abdominal lesions were regressed after 5 months of treatment. Nivolumab was administered every month thereafter and the metastases were successively controlled. MRI and CT scans confirmed complete response to treatment and absence of recurrence. The patient was in good health and without recurrence 3.5 years after TAE.
The incidence of malignant melanoma is rapidly increasing worldwide, with 4% of patients developing metastatic disease leading to poor prognosis, and a 5-year survival rate of 18% [7] .Liver involvement occurs in 14% to 20% of cases and is usually asymptomatic [1] . Metastatic melanoma to the liver is still difficult to treat and it is often associated with disseminated disease. In cases of limited and resectable lesions, R0 surgery followed by systemic adjuvant therapy is recommended [8] . Instead, in cases of non-resectable lesions or if there is evidence of residual disease,a systemic therapy should be performed [8] .
The prevalence of bleeding from hepatic tumors is only 1% [9] .It occurs more frequently in patients with hepatocellular carcinoma (HCC) and is associated with high mortality rates. Bleeding from liver metastases is unusual, with less than 50 cases described in literature. The spontaneous rupture of melanoma liver metastasis is an extremely rare entity, with only few cases reported in the literature all with fatal outcomes [2-5] . Currently the standard first-line treatment for patients with ruptured liver tumor is TAE,both in stable and unstable conditions. Surgery should be reserved for the most severe cases and should follow the principles of abbreviated damage control laparotomy [9] . Surgical techniques include hepatic resection, hepatic artery ligation and perihepatic packing. The aim is to achieve hemostasis and prevent recurrent hemorrhage. Bleeding is effectively controlled by selective TAE since liver tumors are often supplied only by the hepatic artery or one of its branches. Since the rest of the liver has a double blood supply, selective arterial embolization does not cause significant hepatic dysfunction [5] . One should however keep in mind that TAE can be difficult to perform in severe cases, especially in hemodynamically unstable patients. In fact, active contrast leakage is not easy to detect in patients with hypotension and the active bleeding site can be obscured by large intraperitoneal hemorrhage.
Common embolic agents used in the treatment of ruptured hepatic tumors are usually non-absorbable (such as PVA particles,cyanoacrylate glue, coils), but absorbable agents (gelatin sponge)have also been used towards this purpose. In our case, TAE was performed using absorbable gelatin sponge particles, which has no toxic or antigenic effects on the body, and can be absorbed completely within approximately one month. Absorbable gelatin sponge is a less invasive embolic agent compared to PVA particles or cyanoacrylate glue which adheres to the vessel wall and causes an acute inflammatory reaction and chronic vessel fibrosis. Another advantage of absorbable agents is that they can be repeatedly used if a second spontaneous bleeding occurs. Furthermore, our experience with portal vein embolization using absorbable gelatin sponge particles or powder shows that its accidental migration in the contralateral vessel during embolization is rapidly cleared by the portal flow, avoiding major complication or fatal outcome,while the leakage of permanent agents such as cyanoacrylate can often prove fatal for the patient [10] . This should also be the case for TAE, since arterial flow should allow dissolution of absorbable gelatin sponge particles but not of cyanoacrylate, the latter leading probably to disastrous outcomes if it migrates to the contralateral hepatic artery in the context of TAE for massive bleeding due to ruptured hepatic metastases. Finally, our patient had complete portal trunk thrombosis at the time of massive bleeding which made the non-absorbable material impossible. We believe that the absorbable gelatin sponge particles prevented a fatal outcome in our case, allowing healing and long-term survival of the patient.
It should be noted that although TAE has become the first-line treatment for spontaneous rupture of hepatic tumors in selected patients, it remains a demanding and potentially morbid procedure. For this reason, it should be performed only in specialized centers by well-trained and experienced interventional radiologists, backed up by experienced liver surgeons ready to intervene if necessary.
In conclusion, spontaneous rupture of hepatic metastases from cutaneous melanoma is a rare entity, associated with a high mortality rate. The first management options should be TAE, and surgery is for back up or for severe cases. TAE has proven to be an effective first-line treatment for ruptured hepatic tumors, even in presence of massive hemoperitoneum. Absorbable agents, such as gelatin sponge particles used in this case, may have numerous advantages compared to non-absorbable agents.
CRediT authorship contribution statement
Panagiotis Lainas:Conceptualization, Investigation, Writing -original draft.Giorgia Amy Rodda:Investigation, Writing - original draft.George Rafek:Data curation, Formal analysis.Maude Millereux:Data curation, Formal analysis.Carmelisa Dammaro:Investigation, Writing - original draft.Pierre Trouiller:Writing -review & editing.Sophie Maitre:Conceptualization, Writing - review & editing.Ibrahim Dagher:Supervision, Writing - review &editing.
Funding
None.
Ethical approval
This study was approved by the local Ethics Committee at Antoine-Beclere Hospital, Clamart, Paris, France.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- MEETINGS AND COURSES
- Liver transplantation for intrahepatic and perihilar cholangiocarcinoma: Current and future
- Pancreatic schwannoma: Imaging features and pathological findings
- Rare giant asymptomatic skull metastasis from intrahepatic cholangiocarcinoma
- Portal stent with endovascular brachytherapy improves the efficacy of TACE for hepatocellular carcinoma with main portal vein tumor thrombus
- Lumen-apposing metal stent deployment for walled-off necrosis using semi-free hand technique from the intestine
