Liver transplantation in a patient with massive polycystic liver disease
2020-05-10ZheYngBultAdrkhimovShuoWngQinFenXieLiZhungShuSenZheng
Zhe Yng , Bult Adrkhimov , Shuo Wng , Qin-Fen Xie , Li Zhung , Shu-Sen Zheng ,*
a Department of Hepatobiliary and Pancreatic Surgery, Department of Liver Transplantation, Shulan (Hangzhou) Hospital, Hangzhou 310022, China
b Zhejiang University School of Medicine, Hangzhou 310000, China
Polycystic liver disease (PLD) is a genetic disorder [1] that is diagnosed by presence of multiple hepatic cysts. Clinical manifestations of PLD are related to the size of hepatic cysts and associated complications. In the early stage, PLD rarely causes any symptoms.However, patients with advanced stage PLD have a variety of clinical manifestations and complications due to severe hepatomegaly.They include abdominal pain, abdominal distension, dyspepsia, ascites and many others that may result from compression of adjacent tissue or organ failure [ 2 , 3 ]. Surgical treatment of PLD includes: aspiration with or without sclerotherapy, cyst fenestration,hepatectomy and liver transplantation. Despite some researchers have concluded that cyst fenestration or hepatectomy is effective in treatment of PLD [4-6] , the only curative surgical option in severe patients is liver transplantation [ 7 , 8 ]. All other types of surgeries present a great challenge to a surgeon, having little or no effect when cysts are diffuse, or even contraindicated due to possibility of life-threatening complications arising during or after the procedure. Herein, we report a case of 51-year-old male diagnosed with massive PLD complicated by abdominal adhesion, liver cirrhosis, splanchnic varices and ascites that successfully underwent liver transplantation.
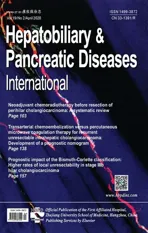
The patient came to our hospital with severe abdominal distension and edema of torso and lower extremities ( Fig. 1 A). He did not have any other symptoms such as abdominal pain, dyspepsia,and nausea. CT scan of the abdomen revealed PLD accompanied by cystic wall calcification, partial intracystic hemorrhage, liver cirrhosis, mild splenomegaly, splanchnic varices, ascites, bilateral renal cysts and pleural effusion ( Fig. 1 B). The patient has a remarkable surgical history. Twenty-seven years ago, he had hepatic cyst aspiration indicating that PLD has been present for at least several decades. One year ago, he underwent endoscopic variceal ligation and tissue glue injection due to upper gastrointestinal bleeding and ruptured gastroesophageal varices (hemoptysis: 10 0 0 mL).The patient was advised to undergo liver transplantation. After 5 months, liver transplantation was performed in the local hospital but was aborted due to severe abdominal adhesion and intraoperative hemorrhage.
The patient underwent modified piggyback liver transplantation in our hospital 8 months after the aborted transplantation. Intraoperative exploration revealed severe adhesion of abdominal cavity, prominent splanchnic varices, large-volume ascites (3500 mL),hepatomegaly and multiple cysts that covered the surface of the liver ( Fig. 1 C-E). In order to overcome severe adhesion, splanchnic varices and possible massive hemorrhage during liver transplantation, a quick hepatectomy and implantation technique was chosen. Upon completing the hilar dissection, we proceeded with the hepatectomy: infrahepatic inferior vena cava and suprahepatic inferior vena cava were clamped, after that we mobilized the liver and removed it. Then, a quick implantation technique was applied.Finally, we sequentially reperfused portal vein and hepatic artery to reduce the anhepatic phase. Graft revascularization time was 28 min, anhepatic phase was 60 min, intraoperative blood loss was 70 0 0 mL and red blood cell transfusion was 25 U.
Post-transplant immunosuppression was based on tacrolimus and intraoperative corticosteroid regimen. Mycophenolate sodium was administered as additional immunosuppressive agent. Liver function was recovered on the 4th day after liver transplantation.There was no graft rejection, biliary tree and vascular complications, and infections. The patient was discharged from the hospital 34 days after transplantation. Abdominal CT and CT angiography scans were performed at 3 and 6 months after liver transplantation; no abnormalities were found ( Fig. 2 ).
The patient was at a high-risk of intraoperative bleeding because of the presence of severe adhesion, splanchnic varices and portal hypertension. We applied a quick hepatectomy and implantation technique, which can significantly reduce intraoperative blood loss. Sequential reperfusion of portal vein and hepatic artery(initial portal revascularization) was chosen on the basis of reduction of anhepatic phase and revascularization time [9] . A recent study identified prolonged revascularization time as predictor of early allograft dysfunction and graft loss in liver transplantation,particularly for the marginal graft [10] . Small abdominal space,large grafts and lack of surgical skills are the risk factors for prolonged graft revascularization time.
There is no curative treatment option for severe PLD except liver transplantation. A quick hepatectomy and implantation technique can reduce anhepatic phase, revasculariation time, intraoperative hemorrhage, graft loss and improve patient outcome.
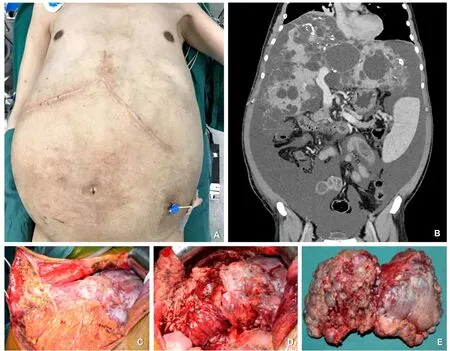
Fig. 1. ( A) Preoperative appearance of the abdomen: severe abdominal distension, λ-like scar from previous liver transplantation (aborted); ( B) Coronal CT scan of the abdomen on admission: hepatomegaly, hepatic cysts with cystic wall calcification, and ascites; ( C) Exposed abdominal cavity; ( D) Exposed liver. ( E) Specimen after hepatectomy:enlarged size, multiple cysts on the surface.
Fig. 2. CT and CT angiography scans were performed at 6 months after liver transplantation. ( A) Abdominal CT scan; ( B) CT angiography scan of hepatic artery; ( C) CT angiography scan of portal vein.
Zhe Yang:Data curation, Formal analysis, Funding acquisition,Resources, Writing - original draft.Bulat Abdrakhimov:Visualization, Writing - original draft, Writing - review & editing.Shuo Wang:Project administration, Resources.Qin-Fen Xie:Writing -review & editing.Li Zhuang:Data curation.Shu-Sen Zheng:Conceptualization, Funding acquisition, Supervision, Writing - review& editing.
Funding
This study was supported by grants from the National S&T Major Project (2017ZX10203205), the Medical Science and Technology Project of Zhejiang Province ( 2014KYA082 ), the Fundamental Research Funds for the Central Universities ( 2018FZA7002 ), and the Shulan Talent Foundation.
Ethical approval
This study was approved by the local ethics committee. Informed consent for publication was obtained from the reported patient.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Neoadjuvant chemoradiotherapy before resection of perihilar cholangiocarcinoma: A systematic review
- Hepatobiliary&Pancreatic Diseases International
- Human microbiome is a diagnostic biomarker in hepatocellular carcinoma
- Current practice of anticoagulant in the treatment of splanchnic vein thrombosis secondary to acute pancreatitis
- Enhanced recovery after surgery program in the patients undergoing hepatectomy for benign liver lesions
- Assessment of biological functions for C3A cells interacting with adverse environments of liver failure plasma