Enhanced recovery after surgery program in the patients undergoing hepatectomy for benign liver lesions
2020-05-10JiMinZhouXiGnHeMioWngYiMingZhoLinShuLongRongWngLuWngAnRongMo
Ji-Min Zhou , Xi-Gn He , Mio Wng , Yi-Ming Zho , Lin Shu , Long-Rong Wng ,Lu Wng , An-Rong Mo , *
a Department of Hepatic Surgery, Shanghai Cancer Center, Fudan University, Shanghai 200032, China
b Education Department, Huashan Hospital, Shanghai Medical College, Fudan University, Shanghai 200040, China
ABSTRACT
Keywords:
Enhanced recovery after surgery
Hepatectomy
Benign liver lesions
Laparoscopy
Liver function
Introduction
Enhanced recovery after surgery (ERAS) aims to reduce postoperative morbidity and improve recovery through reducing the postoperative undesirable sequelae caused by surgical stress response. It was first raised by Kehlet in the 1990s [1 , 2] . After more than two decades of clinical practice and development, the effectiveness of ERAS program has been widely proven in colorectal surgery [3] , urology surgery [4] , orthopedic surgery [5] , gynecology [6] , and many other surgical fields, in some of which guidelines and consensus have been established. The concept of ERAS was gradually introduced to China from Europe and America since the 21st century and was gradually spread in domestic. In the hepatic surgery, the practice and clinical application of ERAS were relatively lagging due to the high risk of hepatectomy [7] . The earliest clinical study exploring the application of ERAS in hepatic surgery can be traced back to 2008 [8] . Then, ERAS has gradually attracted attention in the clinical practice of hepatic surgery over the past decade. A large number of randomized controlled trials (RCTs) [9-11] and meta-analyses [12-16] have emerged domestic and overseas. On that basis, the guidelines and consensus special for hepatectomy were also established [17 , 18] . However, until now, almost all the ERAS studies focused on the ERAS perioperative management process and content of hepatectomy for liver tumors,in which the types of tumors were often mixed. Very few studies have specifically discussed the application characteristics and clinical outcomes of ERAS for a certain type of liver tumor and most of them were focusing on the malignant lesions including hepatocellular carcinoma, peri-hilar cholangiocarcinoma, colorectal cancer liver metastasis [19-21] and parasitic diseases [22] . So far,there has been no study to summarize the characteristics of ERAS in patients with benign liver lesions.
Benefit from the development of radiological technology,the early detection rate of benign liver lesions has been increasing [23] . Benign liver lesions mainly include hemangioma,focal nodular hyperplasia, hepatic adenoma, solitary necrotic nodules. Currently, hepatectomy is the main treatment for these diseases [24] . Liver benign lesions have the following clinical characteristics: follow-up observation is one of the treatment options as well; patients with benign liver lesions are usually without background of liver disease, which make the postoperative recovery easier; patients with benign liver lesions have relatively low acceptance threshold for perioperative adverse events. Higher surgical safety, better perioperative experience, fewer postoperative complications, and shorter hospital stay may show greater significance for patients with benign lesions who choose to receive hepatectomy compared with patients with malignant tumors. Therefore, it is important to explore if ERAS can achieve the expected results in such patient population.
Methods
From September 2016 to June 2019, 233 consecutive patients with pathologically confirmed benign liver lesions who underwent hepatectomy in our center were enrolled retrospectively. Benign liver tumor was defined as follows: hemangioma, focal nodular hyperplasia, solitary necrotic nodules, hepatic adenoma, and others, including angioleiomyolipoma, peliosishepatitis, hepatolithiasis, and inflammatory lesions, such as inflammatory pseudotumor and hepatic abscesses. The criteria of hepatectomy for benign liver diseases in our center are following: (1) tumor volume was larger than 5 cm, or tumor grew rapidly within a short period of time;(2) tumor compression or other conditions caused symptoms; (3)the patient required tumor removal with a strong desire; (4) tumor was suspected malignant from the examinations.
ERAS was implemented in our center since March 1st, 2018.Therefore, 109 patients from September 2016 to February 2018 were enrolled into the control group, and the subsequent 124 patients were enrolled in the ERAS group. ERAS management measures were introduced in Table 1 . The underlying diseases of patients were divided into three subgroups: no other morbidity;cardiovascular disease, hypertension or diabetes; others, included anemia, asthma, and history of other tumors and tuberculosis and so on. The last subgroup also included six patients in each of the two groups with a history of hepatitis B infection, hepatitis C infection, and schistosomiasis. The liver functions of all patients enrolled in the study were Child-Pugh classification A. All data were collected during hospital stay and within 30 days after surgery.Postoperative complications were defined and classified according to the Clavien-Dindo classification criteria. The pain score was classified according to the visual analogue scale (VAS) and score ≥4 was defined as severe pain requiring analgesic treatment. Postoperative recovery of liver function was evaluated by liver function related indicators, such as alanine aminotransferase (ALT),total bilirubin (TBil), prothrombin time (PT), and D -dimer. These indicators were recorded on postoperative day 3. This study was approved by the Ethics Committee of our center.
Statistical analysis was performed using SPSS 16.0 for Windows(SPSS Inc., Chicago, IL, USA) and Graphpad Prism 5 for Windows(Graphpad Software, Inc. San Diego, USA). Quantitative data were presented with mean ±standard error or median (interquartile range) and compared using two-sample Student’st-test or Mann-WhitneyUtest where appropriate. Qualitative data were compared using Pearson Chi-square test or Fisher’s exact test. APvalue of<0.05 was considered statistically significant.
Results
A total of 233 patients with benign liver lesions were recruited in this study. Among these, 109 patients (46.78%) who received traditional perioperative care were in the control group and 124 patients (53.22%) who received ERAS program were in the ERAS group. The clinicopathologic characteristics of the cohort were summarized in Table 2 . The age, sex, underlying diseases, ASA physical status, and BMI of patients in these two groups were similar. In terms of pathologic diagnosis and type of hepatectomy,there was also no significant difference between these two groups.However, a significantly higher proportion of patients underwent laparoscopic surgery in the ERAS group (79.84% vs. 58.72%,P<0.001).
The operative results and postoperative outcomes of these two groups in the whole patient population were listed in the Table 3 .As for the operation related indicators, both intraoperative blood loss and blood transfusion rate were significantly less in the ERAS group than those in the control group [10 0.0 0 (50.0 0-20 0.0 0) mL vs. 20 0.0 0 (10 0.0 0-487.50) mL,P<0.0 01 and 3.23% vs. 10.09%,P= 0.033]. The ERAS group had also shown shorter operative duration in spite of no significant difference [120.00 (90.00-150.00)min vs. 140.00 (95.00-179.75) min,P= 0.056]. As the indicators of postoperative liver function recovery, TBil was significantly lower in the ERAS group [17.10 (13.43-23.85) μmol/L vs. 21.00 (14.83-29.55) μmol/L,P= 0.041]. In terms of coagulation function, D -dimer was dramatically reduced in the ERAS group [2.08 (1.49-2.94) μg/mL vs. 2.57 (1.77-3.49) μg/mL,P= 0.031], while PT was similar in these two groups. For ERAS study common indicators,including days that semiliquid diet was allowed after surgery, abdominal drainage tube indwelling duration, and hospital stay after surgery, all these indicators were significantly shorter in the ERAS group (allP<0.05). In terms of pain score, the proportion of patients with pain score ≥4 was significantly lower than that in the control group within postoperative five days except the first two days after surgery (6.45% vs. 13.76%,P= 0.062 and 16.13% vs.24.77%,P= 0.101; Fig. 1 (A)). The hospital costs between these two groups were similar (P= 0.784). The postoperative complications in the study were also analyzed. In both groups, 30-day mortality was 0. According to the Clavien-Dindo classification criteria, the incidence of complications in the control group was significantly higher than that in the ERAS group (32.11% vs. 16.13%,P= 0.008).
Due to the uneven distribution of the patients underwent open surgery and laparoscopic surgery in these two groups, stratification analysis was further performed to evaluate the role of ERAS program in different operative methods. The clinicopathologic baselines of ERAS group and control group were comparable in patients underwent these two operative methods (Data not shown). The operative results and postoperative outcomes were shown in Tables 4 and 5 . For postoperative outcomes, ERAS group showed signi ficantly fewer days that semiliquid diet was allowed and hospital stay after surgery than the control group in both operative methods (allP<0.001). In patients underwent laparoscopic surgery,among other postoperative indicators, a significant difference was shown in the pain score on postoperative day 4 after surgery between ERAS and control group (P= 0.008; Fig. 1 (B)). Impressively,ALT level in the ERAS group was significantly higher than that in the control group [124.20 (67.60-215.10) U/L vs. 83.35 (51.13-158.18) U/L,P= 0.027] in patients underwent laparoscopic surgery.In patients underwent open surgery, the ERAS group demonstrated a significantly shorter operative duration (131.76 ±8.75 min vs.160.73 ±7.23 min,P= 0.016), less blood loss [20 0.0 0 (10 0.0 0-325.0 0) mL vs.450.0 0 (20 0.0 0-625.0 0) mL,P= 0.0 08], lower post-operative morbidity (16.00% vs. 4 4.4 4%,P= 0.040), and significantly different pain score on postoperative day 3 (P= 0.013;Fig. 1 (C)). There were different patterns of postoperative pain and analgesic effect between patients underwent laparoscopic and open surgery. In addition, ALT level in the ERAS group was lower than that in the control group, although with no significant difference [147.65 (62.05-179.08) U/L vs.220.90 (119.50-350.63) U/L,P= 0.060].
Discussion
This study explored the role of ERAS in patients underwent hepatectomy for benign liver lesions. Compared with traditional perioperative care, ERAS had shorter hospital stay, fewer postoperative complications, less intraoperative blood loss, and better postoperative liver function.
The demographic baseline between the two groups of this study was comparable. A significantly higher proportion of patients underwent laparoscopic surgery in the ERAS group (79.84% vs.58.72%). Ratti et al. [21] reported that laparoscopic approaches may be associated with reduced blood loss and postoperative morbidity,which was similar to the open surgery group treated with ERAS program. Laparoscopic hepatectomy itself may be an approach of ERAS and recommended by the consensus [18] .
The anesthesia strategy of our ERAS program specifically emphasized the low central venous pressure (CVP) technique(CVP<5 mmHg, systolic blood pressure>90 mmHg), which was extremely critical to the hepatectomy. Hughes et al. [25] verified that low CVP could significantly reduce the intraoperative blood loss and transfusion rates in hepatectomy. The low CVP strategy may provide a safer hepatectomy, a cleaner surgical field and an easier operation. A trend of shorter operative duration in the ERAS group with more laparoscopic surgeries in this study should also partially owe to low CVP. Another major objective of our study was to observe the change of liver function impairment after ERAS implement. In clinical practice, it has been shown that the peak liver damage occurs 3-4 days after surgery. All patients in our study showed normal preoperative liver function. Thus, we compared the results of liver and coagulation function tests in the third day after hepatectomy, and found that the TBil and D -dimer levels in the ERAS group were significantly lower which suggests that liver function impairment caused by hepatectomy may be milder in the ERAS group. The minor surgical trauma due to ERAS was the critical reason.
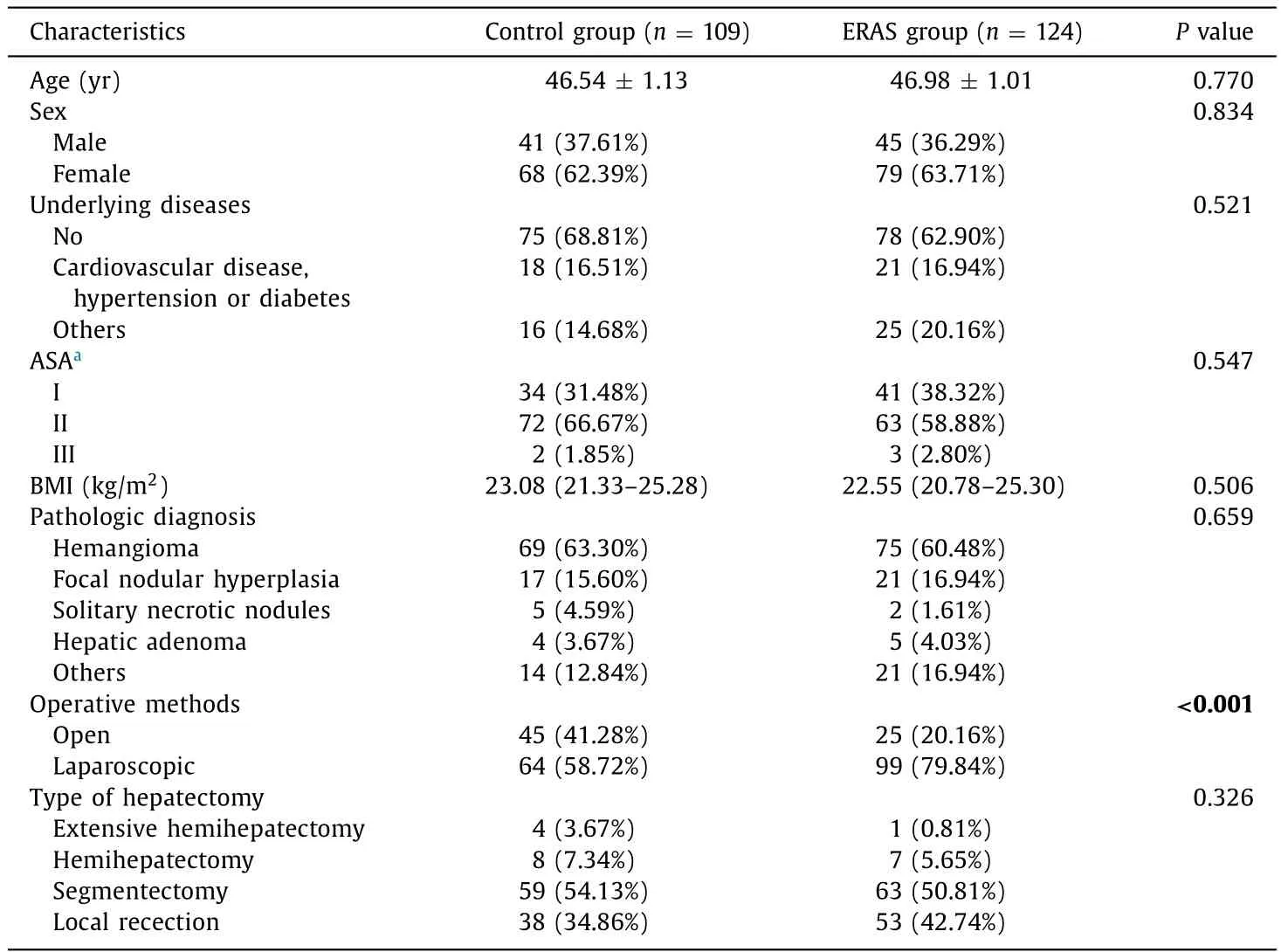
Table 2The clinicopathologic characteristics of patients.
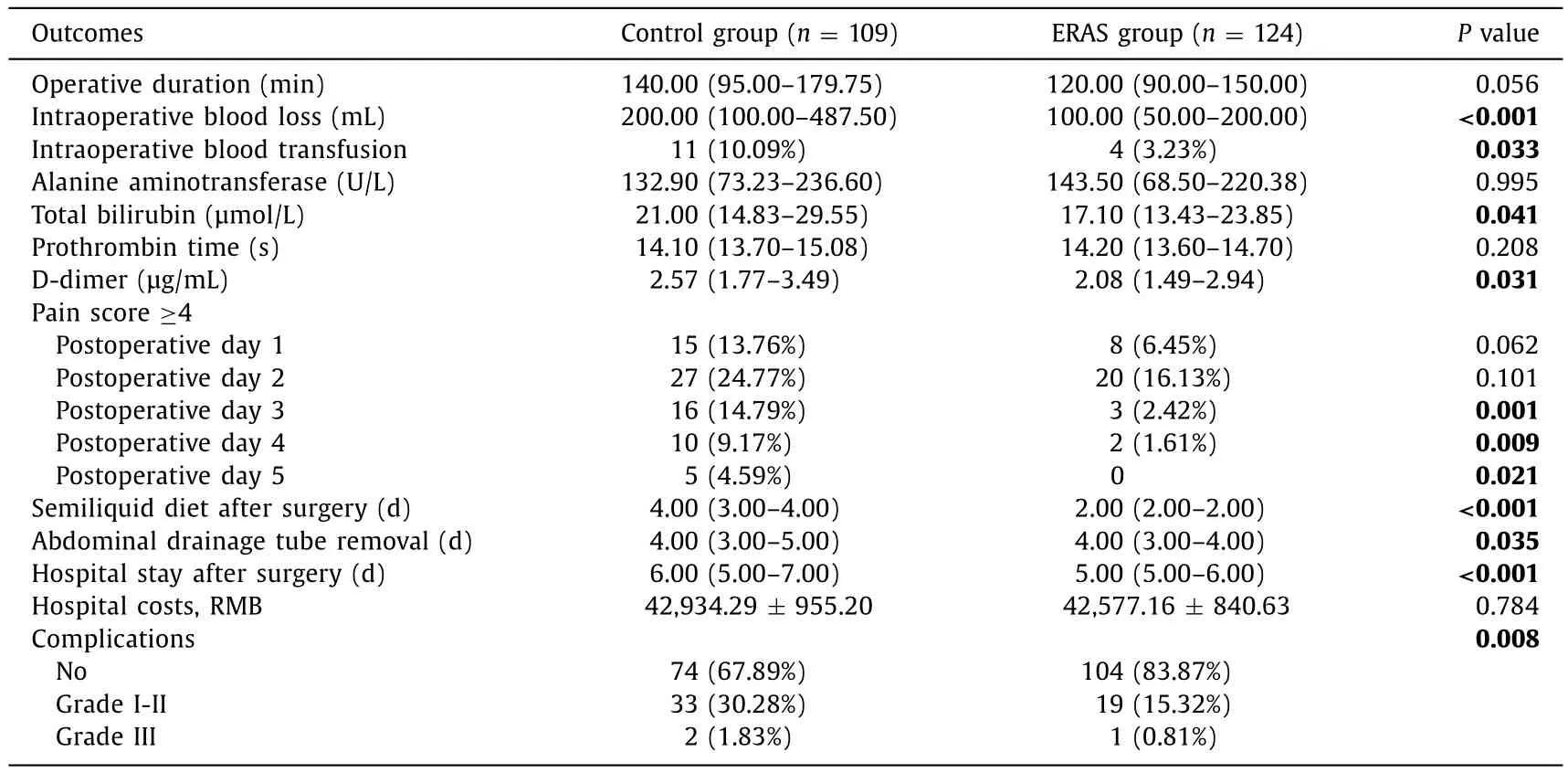
Table 3Operative results and postoperative outcomes in the whole patient population.
Mitigated postoperative pain, nausea and vomiting for the implement of ERAS may alleviate postoperative stress and improve the recovery of liver function. We have to mention that the patients in the ERAS group were routinely treated with lowmolecular-weight heparin (LMWH) for anticoagulation postoperatively. LMWH has been shown not to increase the risk of postoperative hemorrhage [18] . The PT level was not longer after the application of LMWH and impressively, the level of D -dimer wassignificantly reduced in the study and therefore, LMWH was safe and effective to be applied to relieve hypercoagulability and prevent thrombotic complications after operation without deteriorating coagulation function, although LMWH was not recommended by the consensus [18] . The reduced surgical trauma and accelerated postoperative recovery of liver function reflect the merit of ERAS in hepatectomy of patients with benign liver lesions.

Table 4Operative results and postoperative outcomes in patients underwent open surgery.
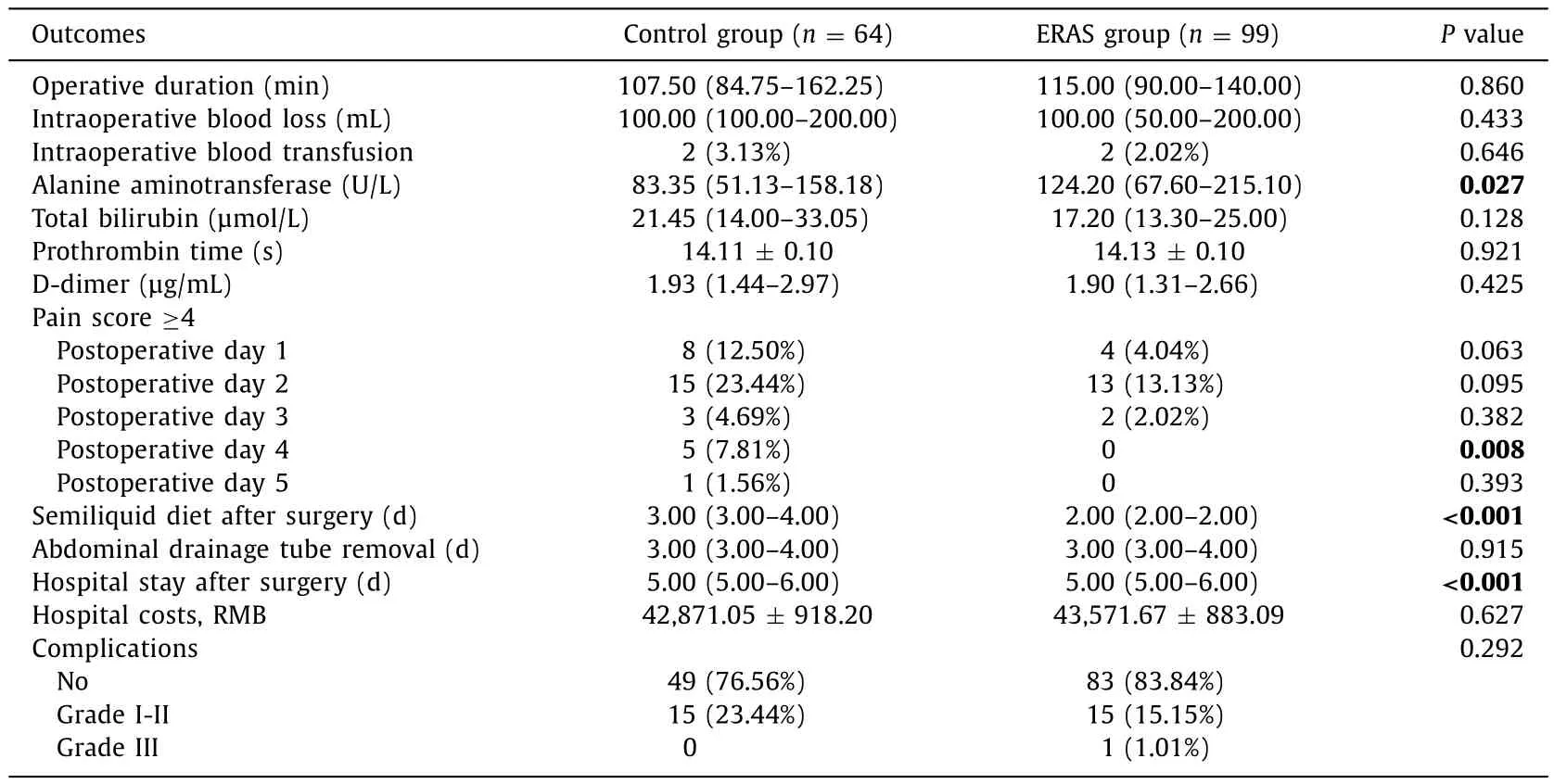
Table 5Operative results and postoperative outcomes of patients underwent laparoscopic surgery.
Patients with ERAS significantly shortened postoperative hospital stay, abdominal drainage tube removal, and semiliquid diet intake. Postoperative complications were reduced by almost half,with an incidence of 32.11% in the control group to 16.13% in the ERAS group. Our results were the same as the previous studies [12-16] . Most of these studies focused on malignancies such as hepatocellular carcinoma, and these results were similar to what we reported in the benign liver lesion populations.
Management of postoperative pain is a major component of ERAS. Our analgesia strategy was close to what Liang et al. [26] reported: routine analgesic pump one day + intravenous parecoxib sodium (Dynastat) twice a day. In the whole patient population,the proportion of patients requiring pharmaceutical intervention was reduced by 50% in the ERAS group compared with the control group for postoperative five consecutive days. Actually, a trend of difference had been shown at day one postoperatively. The reason why there was no difference at day two may be that this is the routine day withdrawal of analgesic pump. The analgesic function of intravenous parecoxib sodium was still not completely effective in part of insensitive patients. The pain could be controlled better in the following days. Further stratified analysis showed that the analgesic effect in patients underwent laparoscopic surgery was earlier than that in patients underwent open surgery. The results indicated the effectiveness of postoperative analgesia strategies in our ERAS program, which made the patients with benign diseases experience a better postoperative recovery.
For hospital costs, no difference was shown between the two groups. It might be due to a higher proportion of laparoscopic surgery in the ERAS group which is higher than that of open surgery. The total cost in our center was much lower than those reported in other centers [26-28] . Actually, the costs associated with treatment of benign liver diseases should be less than those with malignant tumors. Therefore, the hospital costs were relatively lower in our study.

Fig. 1. The proportion of patients with the score ≥4 in the control group and ERAS group within 5 days after operation. ( A) Whole patient population, the proportion of patients with severe pain was much lower in the ERAS group. ( B) Patients underwent laparoscopic surgery, a significant difference was shown at day 4 after surgery. ( C ) Patients underwent open surgery, the ERAS group demonstrated significantly less proportion of patients with severe pain at day 3 after surgery.*P < 0.05.
Due to the different proportion of laparoscopic surgeries, stratified analysis was further performed to explore the different roles of ERAS in patients underwent laparoscopic or open surgery for benign liver lesions. As expected, ERAS showed a more significant effect in the open surgery group. In addition to the shorter semifl uid diet intake day and postoperative hospital stay in both open and laparoscopic surgery group with ERAS implement, shorter operative duration, less blood loss, and less incidences of postoperative complications were revealed in the open surgery group as well. The results suggested that the effect of ERAS implement in the laparoscopic surgery and open surgery may be different. A previous meta-analysis [13] has revealed that the implement of ERAS in the patients underwent laparoscopic surgery could reduce the postoperative hospital stay and overall complications, but not the operative duration, intraoperative blood loss, nor blood transfusion.Recently, only Liang’s study confirmed the above conclusion [26] .In several other studies, ERAS implement in laparoscopic surgery could only reduce the hospital stay, not the postoperative complications, or neither [28 , 29] . Compared with laparoscopic surgery, although ERAS implement in open surgery was not superior to traditional perioperative care in the operative time and blood loss,ERAS implement shortened hospital stay and decreased complications [30] . As mentioned above, laparoscopic hepatectomy itself may be an approach of ERAS [21] and the postoperative surgical stress response was much lower than that of open surgery. Therefore, although parts of patients were not suitable for laparoscopic surgery, perioperative ERAS implement during open surgery could improve the patient outcomes.
In summary, ERAS program significantly improved the postoperative recovery and did not affect the hospital costs. Stratifi ed analysis unveiled that ERAS showed more advantages in the open surgery than the laparoscopic surgery. Therefore, ERAS program was suitable for the patients underwent hepatectomy, especially open surgery, for benign liver lesions. The limitation of this study is the retrospective nature which may lead to bias of results.Prospective large sample studies are necessary to further validate our data.
CRediT authorship contribution statement
Jia-Min Zhou:Data curation, Formal analysis, Writing - original draft.Xi-Gan He:Data curation, Formal analysis, Writing - original draft.Miao Wang:Data curation, Methodology.Yi-Ming Zhao:Methodology.Lian Shu:Data curation, Validation.Long-Rong Wang:Validation.Lu Wang:Conceptualization, Writing - review& editing.An-Rong Mao:Conceptualization, Supervision, Writing -review & editing.
Funding
None.
Ethical approval
This study was approved by the Ethics Committee of Shanghai Cancer Center, Fudan University. Written informed consent was obtained from all participants.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Neoadjuvant chemoradiotherapy before resection of perihilar cholangiocarcinoma: A systematic review
- Hepatobiliary&Pancreatic Diseases International
- Human microbiome is a diagnostic biomarker in hepatocellular carcinoma
- Current practice of anticoagulant in the treatment of splanchnic vein thrombosis secondary to acute pancreatitis
- Assessment of biological functions for C3A cells interacting with adverse environments of liver failure plasma
- Transarterial chemoembolization versus percutaneous microwave coagulation therapy for recurrent unresectable intrahepatic cholangiocarcinoma: Development of a prognostic nomogram