Survival improvement and prognostic factors in recent management of extrahepatic cholangiocarcinoma: A single-center study
2020-05-10JungWnChoeHyoJungKimJeSeonKim
Jung Wn Choe Hyo Jung Kim Je Seon Kim
a Division of Gastroenterology, Department of Internal Medicine, Korea University Ansan Hospital, Korea University College of Medicine, 516 Gojan-dong,Danwon-gu, Ansan-si, Gyeonggi-do, 15355, Korea
b Division of Gastroenterology, Department of Internal Medicine, Korea University Guro Hospital, Korea University College of Medicine, 148 Gurodong-ro,Guro-gu, Seoul 08308, Korea
ABSTRACT
Keywords:
Cholangiocarcinoma
Survival
Prognosis
Introduction
Cholangiocarcinoma (CC) has been studied with limitations,mainly due to the low incidence compared to other digestive malignancy. However, its incidence is increasing and patients have poor outcomes [1 , 2] . Until recently, only 20% of patients with biliary tract cancer were known to be eligible for surgical resection with curative intent. Nevertheless, recurrence rates of CC remain high even after radical resection, and the 5-year overall survival(OS) postoperatively has been reported in the range of 25%-35% [3] .
However, prognosis of CC should be subdivided according to classification of intrahepatic cholangiocarcinoma (ICC) and extrahepatic cholangiocarcinoma (ECC), to identify the prognostic factors, because CC represents a heterogeneous tumor with different risk factors and geographic variation [4 , 5] . The survival improvement in ECC is recently suggested with multidisciplinary management [6 , 7] .
Various studies have investigated ICC. However, most of the well-defined clinical studies on ECC are very limited to surgical patients although many patients were not eligible for surgery, because unresectable patients are difficult to stratify properly [8] . Therefore, this study aimed to investigate the survival improvement of ECC and determine prognostic factors in recent patients treated with advanced modality.
Methods
Patients
Patients diagnosed with ECC between January 2014 and December 2016 and followed at Korea University Guro Hospital were included. Eligible patients were aged ≥18 years and had histologically confirmed CC. Patients who had ICC, gallbladder cancer, ampullary cancer, and high-grade dysplasia or carcinomainsituwere excluded. Moreover, patients with a history of chronic biliary diseases, such as cholelithiasis, sclerosing cholangitis, and liver fluke, were excluded.
Patients’ clinicopathological data were retrospectively reviewed and analyzed. Tumor location was classified as the distal common bile duct (CBD) cancer, proximal CBD cancer, common hepatic duct cancer, and hilar cancer. In pathological analysis, presence of dysplasia was defined as combined high-grade dysplasia in resected bile duct. Past medical history was reviewed for previous cancer treatment and comorbidity such as chronic kidney disease, diabetes mellitus, liver cirrhosis, chronic obstructive pulmonary disease, coronary heart disease, and human immunodeficiency virus infection. The OS time was calculated from the date of hospital visit.
Statistical analysis
All statistical analyses were performed using the IBM SPSS software (version 22.0; SPSS Inc., Chicago, IL, USA). Survival analysis was presented using the Kaplan-Meier method. Survival rates between groups were compared using the log-rank test. The Cox regression proportional hazards model was used to identify independent prognostic factors.Pvalues of<0.05 were considered statistically significant.
Results
A total of 83 patients, consisting of 49 men and 34 women,with a median age of 73.3 (range 49-93) years, were included. Out of 83 patients, cancer was located at the distal CBD in 25, proximal CBD in 24, common hepatic duct in 20, and hilar in 14 patients.
Surgical treatment for resectable ECC
Surgical resection was possible in 54 patients (65%). Resection was performed in 80% (20/25) of distal CBD cancer, 79% (19/24) of proximal CBD cancer, 50% (10/20) of common hepatic duct cancer,and 36% (5/14) of hilar cancer. Dysplasia was detected in 34 of 54 surgical patients. Postoperative mortality occurred in 3 patients:one due to bleeding, one leakage, and one acute kidney injury.Adjuvant chemotherapy was performed in 29 of 54 patients with gemcitabine-based regimen.
Nonsurgical treatment for unresectable ECC
Tumors in 29 patients (35%) were unresectable. Biliary stenting for drainage was performed in all nonsurgical patients; however,only 7 of unresectable patients underwent palliative chemotherapy with gemcitabine and cisplatin as the first-line treatment.

Fig. 1. The survival curves of postoperative adjuvant chemotherapy, surgery only,palliative chemotherapy, and supportive care groups were significantly different( P < 0.05).

Table 1Univariate Cox regression analysis of survival in all patients.
History of malignancy or comorbidity
Twelve patients (14.5%) had history of another malignant neoplasm which was gastric cancer in 4 patients, colon cancer in 3, lung cancer in 2, bladder cancer in 1, cervical cancer in 1,and pharyngeal cancer in 1. Twenty patients (24.1%) had chronic illness, such as chronic kidney disease, diabetes mellitus, and chronic obstructive pulmonary disease.
Survival
The median OS in all patients was 30.9 (25.1-36.6) months.The median survival was 38.5 (32.1-45.0) months in the surgery group compared with 9.9 (7.0-12.9) months in the nonsurgery group (P<0.05). In the survival analysis based on the treatment modality, median survival of postoperative adjuvant chemotherapy,surgery only, palliative chemotherapy, and supportive care groups were 42.9 (34.8-51.0), 30.9 (21.8-40.1), 12.0 (10.3-13.8), and 8.9(5.5-12.5) months, respectively (P<0.05). The survival curves between surgery and nonsurgery groups were significantly different in terms of chemotherapy ( Fig. 1 ).
Cox proportional hazard analysis for risk factors associated with survival
The Cox regression model identified younger age, surgical resection, chemotherapy, and absence of comorbidity as good prognostic factors for survival ( Table 1 ). In a multivariate analysis, the comorbidity was only a risk factor (hazard ratio [HR] = 2.80; 95%CI: 1.32-5.95;P= 0.007) ( Table 2 ). In a subgroup analysis of surgical patients, the presence of dysplasia was a favorable prognostic factor for OS in the multivariable analysis, with HR of 0.29 (95% CI:0.09-0.91;P= 0.033) ( Tables 3 and 4 ).
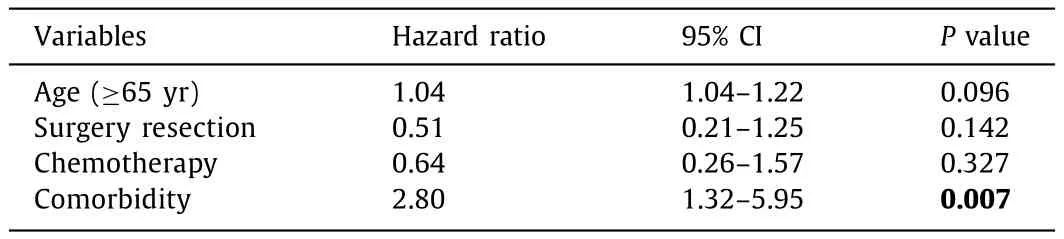
Table 2Multivariate cox regression analysis of overall survival in all patients.
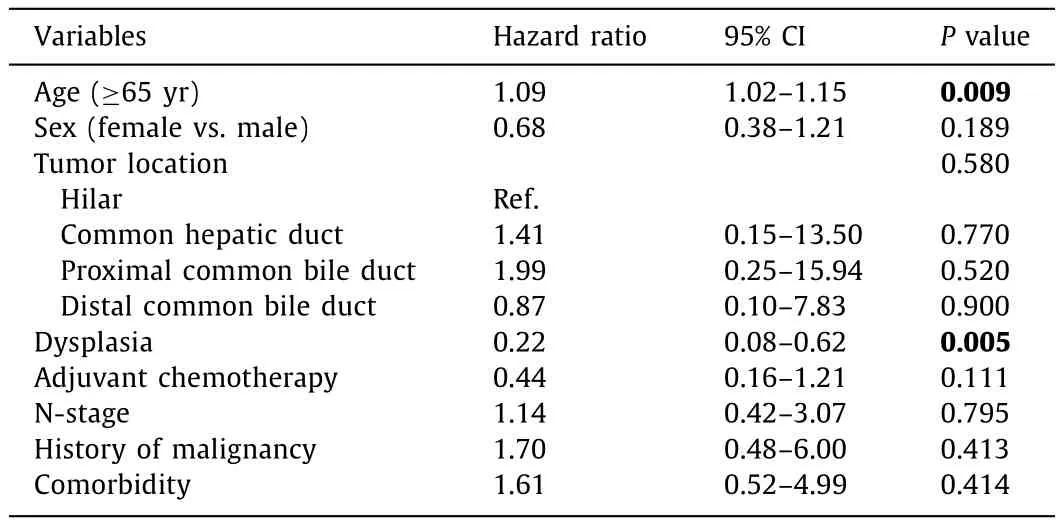
Table 3Univariate cox regression analysis of survival in surgical patients.
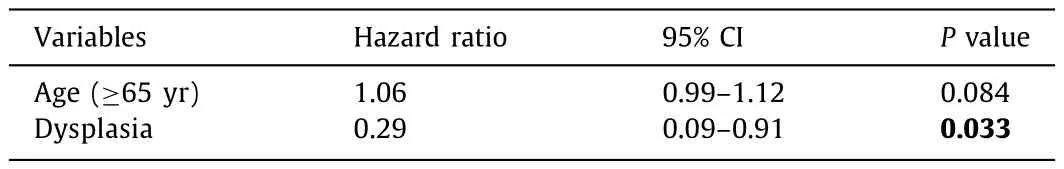
Table 4Multivariate cox regression analysis of overall survival in surgical patients.
Discussion
CC is known to have poor prognosis, because many patients present with advanced stage and relapse is very high even after the curative resection. A few randomized controlled trials have recently reported the survival benefit of adjuvant chemotherapy following the curative resection [3] ; however, most studies focused on the biliary tract cancer, not only CC but also gallbladder or ampullary cancer [9 , 10] . CC should be differentiated from biliary tract cancer, and distinction between ICC and ECC should also be identified.
Recent studies [11 , 12] have reported that adjuvant chemotherapy after the ICC resection improves survival; however, there was no improvement in resected ECC [12] . Until recently, the adjuvant treatment for ECC remains to be established because of limited and inconsistent results. The American Society of Clinical Oncology guideline recommends adjuvant chemotherapy for resected biliary tract cancer [10] ; however, reducing the local recurrence regardless of survival may be reasonable in patients with ECC or those who underwent R1 resection.
In our study, adjuvant chemotherapy improved survival after ECC resection. Korea has a high prevalence of CC, the 6th cause of cancer mortality. The incidence of liver fluke and ICC has decreased due to lifestyle modification and ultrasound screening, but that of ECC and surgical resection is increasing. Although a study on global trends in mortality reported that ECC mortality tended to decrease in most countries [6] , another nationwide cohort study reported that resection rates and use of palliative chemotherapy have increased, but OS remained stable at 10.4 months [13] . This study showed the survival improvement in ECC patients, and positive effect of chemotherapy on OS. It is suggested that chemotherapy could enhance the strategies for multidisciplinary treatment.
In this study, comorbidities were the only independent risk factor of survival with an HR of 2.80. Most patients with CC are older than those with other digestive cancers [14] . In addition,various locoregional problems were also frequently observed in patients with ECC, even after biliary metal stenting. Chronic comorbid medical conditions contribute to reduced performance status despite the optimal multidisciplinary care and influenced the risk for survival.
Several studies have reported the prognosis after ECC resection [15-18] . R1 margins and nodal metastasis are wellknown risk factors associated with survival. With advances in surgical treatment, noncurative R1 resection is frequently performed. However, studies on dysplasia and prognosis have been limited. In our surgical patients, presence of dysplasia was a favorable prognostic factor for survival (HR = 0.29). Until now, the clinical implication of presence of dysplasia was not fully assessed. It is suggested that presence of dysplasia as precancerous lesion shows stepwise progression from dysplasia to carcinoma, whereas aggressive carcinogenesis also occurs in dysplasia-negative lesion [19 , 20] .
This study has several strengths. First, the benefits of chemotherapy were compared in ECC patients with and without resection. Second, an in-depth analysis on the risks related to survival was performed. Effects of comorbidity and dysplasia were also evaluated to analysis the heterogeneous conditions of ECC patients. Thirdly, Korea provides a universal health coverage to cancer patients by paying only 5% of the costs through the national health insurance [21] . In this study, survival was fully assessed because high-quality medical care was provided for all patients.
However, this study has limitations. First, the number of enrolled patients was small because this study population was limited to recently treated patients with advanced modality. It is difficult to identify the prognostic factors in heterogeneous treatment modalities. Second, this study did not explore the racial and ethnic differences associated with ECC based on geographic differences in the prevalence and etiology. However, patients with chronic biliary diseases such as sclerosing cholangitis,cholelithiasis, or liver fluke, were excluded.
In conclusion, the OS of patients with ECC was quite high, i.e.,30.9 months, and chemotherapy was effective on survival. Absence of comorbidity and presence of dysplasia were good prognostic factors for survival.
CRediT authorship contribution statement
Jung Wan Choe:Data curation, Writing - original draft.Hyo Jung Kim:Conceptualization, Formal analysis, Writing -review & editing.Jae Seon Kim:Methodology, Validation.
Funding
None.
Ethical approval
This study was approved by the Ethics Committee of Korea University Guro Hospital (No. 2016GR0133).
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Neoadjuvant chemoradiotherapy before resection of perihilar cholangiocarcinoma: A systematic review
- Hepatobiliary&Pancreatic Diseases International
- Human microbiome is a diagnostic biomarker in hepatocellular carcinoma
- Current practice of anticoagulant in the treatment of splanchnic vein thrombosis secondary to acute pancreatitis
- Enhanced recovery after surgery program in the patients undergoing hepatectomy for benign liver lesions
- Assessment of biological functions for C3A cells interacting with adverse environments of liver failure plasma