Benefits and limitations of middle bile duct segmental resection for extrahepatic cholangiocarcinoma
2020-05-10MasayukiAkitaTetsuoAjikiKimihikoUenoDaisukeTsugawaMotofumiTanakaMasahiroKidoHirochikaToyamaTakumiFukumoto
Masayuki Akita, Tetsuo Ajiki , Kimihiko Ueno, Daisuke Tsugawa, Motofumi Tanaka,Masahiro Kido, Hirochika Toyama, Takumi Fukumoto
Department of Hepato-Biliary-Pancreatic Surgery, Kobe University Graduate School of Medicine, Kobe, 650-0017, Japan
ABSTRACT
Keywords:
Cholangiocarcinoma
Middle bile duct resection
Pancreaticoduodenectomy
Introduction
Surgical resection is the only way to achieve long-term survival in cholangiocarcinoma, and pancreaticoduodenectomy (PD)or hemihepatectomy with bile duct reconstruction is the standard procedure worldwide [1-3] . However, these extensive resections are highly invasive and often result in major morbidities, such as postoperative liver failure, bile leakage or pancreatic fistula [4-6] .
In a daily clinical setting, surgeons must assess the feasibility of operating on elderly patients or patients in a poor general condition. Because these patients tend to suffer from postoperative major complications, reoperation and re-admission, non-surgical treatments are often offered to them [7-11] .
Bile duct segmental resection (BDR) is undertaken with curative intent for some patients with bile duct cancers confined to the middle bile duct, but there are few reports on the success of this procedure [12 , 13] . Some investigators suggested that prognosis for BDR was similar to PD, but BDR resulted in more R1 resection and lower numbers of harvested lymph nodes [12 , 13] . Some prognostic factors were identified in patients with bile duct cancer, including preoperative cholangitis, duration of surgery, lymph node metastasis, lymph node count, and adjuvant chemotherapy [14-19] . The aim of this study was to compare clinicopathological features of bile duct segmental resection (BDR) with PD in patients with extrahepatic cholangiocarcinoma and validate the applicability of BDR for patients with middle bile duct cancer.

Table 1Clinical features between BDR and PD groups.

Fig. 1. CT image of a representative case in BDR group. A tumor was confined to the middle bile duct, and BDR was selected because of advanced age (83-year-old).Tumor extension was confirmed by the preoperative mapping biopsy, and BDR (left and right hepatic bile duct resection) was performed.
Patients and methods
Patient selection and surgical policy
This study was approved by the Ethics Committee of Kobe University Graduate School of Medicine. The study cohort consisted of 105 patients with bile duct cancer for whom R0 or R1 resection could be accomplished by BDR (n= 21) or PD (n= 84) at Kobe University Hospital between January 20 0 0 and December 2016.There was no patient with in-hospital death or with conversion from BDR to PD intraoperatively. Patients suspected of having bile duct cancer were preoperatively assessed by endoscopic retrograde cholangiopancreatography, computed tomography, magnetic resonance cholangiopancreatography, and positron emission tomography. BDR was selected for patients whose tumor was found to be confined to the middle bile duct by preoperative multimodality imaging and mapping biopsy (n= 10), or for patients in a poor general condition who were expected to acquire at least ductal margin with carcinomain-situ(R1cis) resection (n= 11) ( Fig. 1 ).Characteristics of those patients considered to be in a poor general condition were advanced age (n= 4), having severe heart disease (n= 3), severe systematic disease (primary macroglobulinemia,n= 1) or poor performance status (n= 3). Ductal margins were routinely controlled by intraoperative rapid pathological diagnosis, and additional resection was performed for R0 when possible. Lymph node dissection was performed in the BDR group for station 12 (hepatoduodenal ligament), 8 (common hepatic artery),and 13a (infra-pancreatic area) [20] .
Clinicopathological evaluation
Perioperative clinicopathological data were obtained from the electronic patient records. Preoperative presentation, serum tumor markers, surgery-associated data, pathological findings and prognosis were reviewed. Tumors were staged in accordance with the UICC/AJCC TNM classification, 7th edition [21] .
Statistical analysis
Continuous variables not showing a bell-shaped distribution were assessed using Mann-WhitneyUtest. Categorical variables in each group were compared using the Chi-square test or Fisher’s exact test. Overall and disease-free survivals were calculated using the Kaplan-Meier method. Cox regression analysis was performed using factors withP<0.10 in the univariate analysis to identify statistical significance in multivariate analysis of prognostic factors. JMP R ○12 (SAS Institute Inc., Cary, NC, USA) was used for the statistical analysis. APvalue<0.05 was considered statistically significant.
Results
Clinical characteristics
As shown in Table 1 , patients in the BDR group were signi ficantly older than those in the PD group (74 vs. 70 years,P= 0.04).The rates of preoperative jaundice and cholangitis were similar in the two groups (71% vs. 75%,P= 0.74 and 62% vs. 65%,P= 0.76,respectively). Preoperative biliary drainage was performed in 81%of BDR group patients and 88% of the PD group (P= 0.39). No significant differences were found for serum levels of tumor markers (carcinoembryonic antigen and carbohydrate antigen 19-9). Details of surgical procedures for PD were as follows: 19 conventionalPD, 10 pylorus-preserving PD (PPPD) and 55 subtotal stomachpreserving PD (SSPPD). Duration of surgery and blood loss were significantly less in the BDR group than in the PD group (421 vs.553 min,P<0.01 and 402 vs. 770 mL,P<0.01, respectively). Postoperative major complications (Clavien-Dindo>IIIa) were more frequently encountered with PD (46%) than BDR (10%) (P<0.01).Thus, pancreatic fistula (n= 29), intraabdominal abscess (n= 3),pneumonia (n= 2), deep venous thrombosis (n= 2), bile leakage(n= 1), wound dehiscence (n= 1), and pancreatojejunum anastomotic stenosis (n= 1) were seen in the PD group, but only two intraabdominal abscesses in the BDR group. Postoperative hospital stay was significantly shorter for patients in the BDR group (19 vs.30 days,P= 0.02). Adjuvant chemotherapy (gemcitabine or TS-1)was more commonly given to patients in the BDR group than in the PD group (62% vs. 38%,P= 0.04). In BDR group, 70% of patients with a good general condition (7/10) and 55% of those with a poor condition (6/11) received adjuvant chemotherapy (P= 0.46).

Table 2Pathological findings.
Pathological findings
There were no significant differences in tumor size, tumor differentiation status, lymphatic invasion, vascular invasion and perineural invasion between the two groups ( Table 2 ). In BDR group,length of resected bile duct was 42 mm (IQR 35-50). Tumors in the BDR group were diagnosed as earlier cancer according to the T classification (T1: 14%, T2: 76% and T3: 10%), whereas those in the PD group were more advanced (T3 + 4: 67%). Although the frequency of lymph node metastasis was similar in the two groups,the number of retrieved lymph nodes was significantly lower in the BDR group (8 vs. 13,P<0.01). Most metastases were observed in stations 12 and 13 located along the bile duct. In terms of resection margin status, in the BDR group, R0 resection was present in 8 cases, the rate of which was significantly lower comparing to the PD group (38% vs. 80%,P<0.01). R1 was seen in 13 patients in the BDR group (62%, one patient had 2 cancer positive margins): 4 R1cis (bile duct on the hepatic side:n= 1 and on the pancreatic side:n= 3) and 10 R1inv (on the hepatic side:n= 3, on the pan-creatic side:n= 5 and on the exfoliation area:n= 2). In the PD group, R1 was observed in 17 patients (20%, 2 patients had 2 cancer positive margins): R1cis (bile duct on the hepatic side:n= 2)and 17 R1inv (on the hepatic side:n= 8 and on the exfoliation area:n= 9).
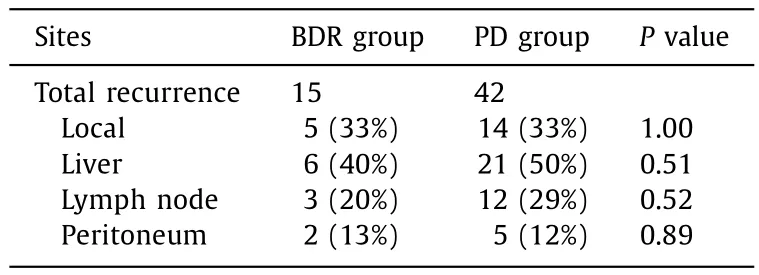
Table 3Primary recurrent sites.
Prognostic outcomes
The median follow-up period was 26 months (range 1-160).Median overall survivals were 37 months in the BDR group and 62 months in the PD group. The 5-year overall survival rates were similar in both groups (44% for BDR vs. 51% for PD,P= 0.72)( Fig. 2 A). During the follow-up period, 57 patients suffered recurrence (55%), with 5-year disease-free survival rates similar in the two groups (38% for BDR vs. 40% for PD,P= 0.99) ( Fig. 2 B). In patients with T1 and T2 cancers, there was no significant difference in overall survival between PD and BDR groups (44% vs. 68%at 5-year,P= 0.09) ( Fig. 2 C). Although BDR group was composed of patients with two different clinical backgrounds, good and poor general conditions, there was no significant prognostic difference between two types of patients (45% vs. 41% at 5-year,P= 0.69,respectively) ( Fig. 2 D). The site of most patients with recurrence was the liver (40% in the BDR group vs. 50% in the PD group), and again, there were no differences in recurrence between the two groups ( Table 3 ). In patients with T1 and T2, BDR group had more local recurrences than PD group (31% vs. 7%,P= 0.04).
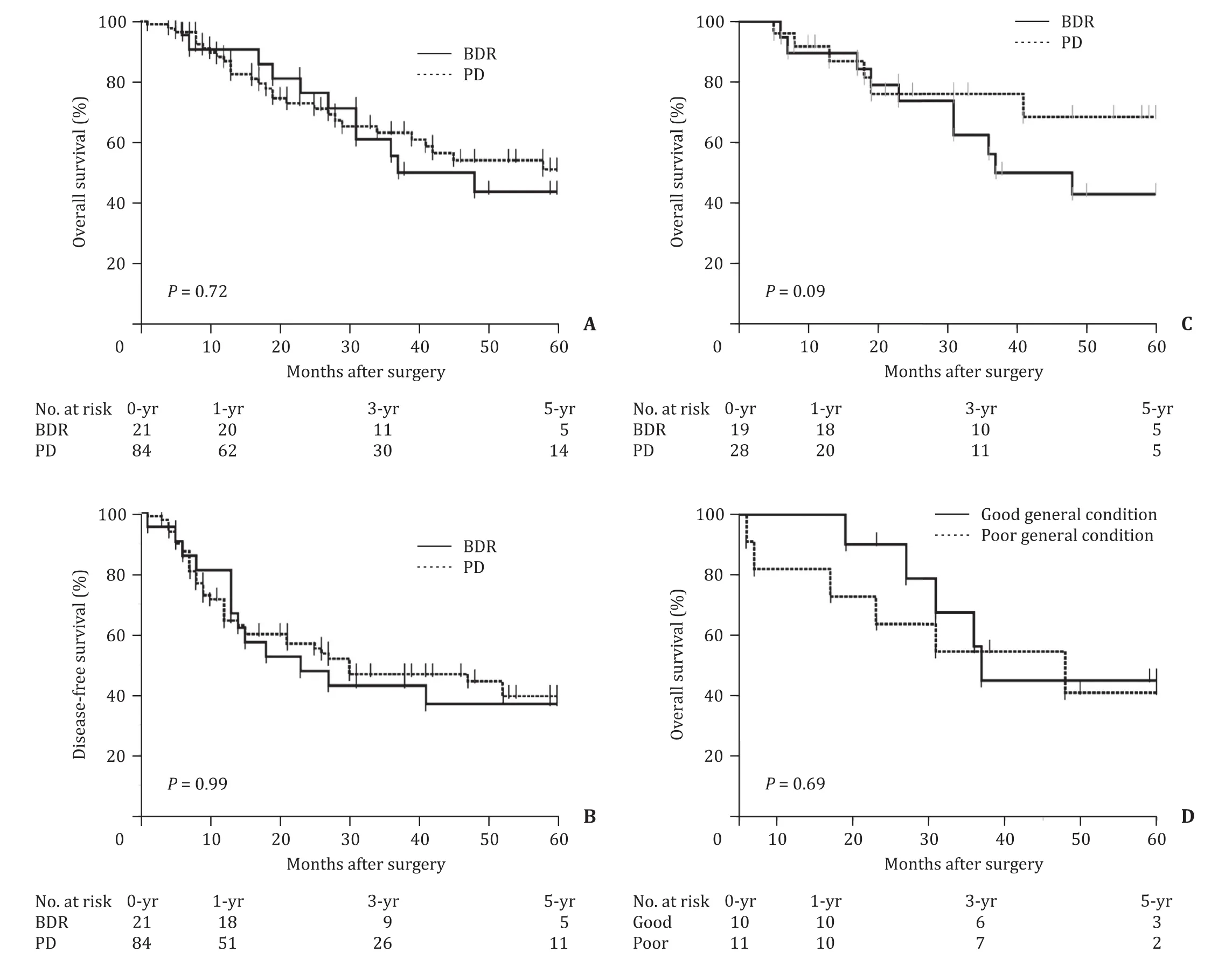
Fig. 2. Prognostic analyses. ( A and B) The 5-year overall and disease-free survival rates, these prognoses were similar between BDR and PD groups (44% vs. 51%, P = 0.72 and 38% vs. 40%, P = 0.99, respectively). ( C) Prognostic sub-analysis in patients with T1 and T2 cancers; there was no significant different between two groups ( P = 0.09).( D) Prognostic sub-analysis in patients with good and poor general conditions revealed no different survival rates ( P = 0.69).
Cox regression analysis revealed that elevated serum carcinoembryonic antigen level (hazard ratio: 2.98; 95% CI: 1.07-7.24;P= 0.04) and R1 resection (hazard ratio: 2.42; 95% CI: 1.26-4.64;P<0.01) were independent prognostic factors in this study cohort( Table 4 ). The nature of the surgical procedure (BDR vs. PD) was not identified as a prognostic factor.
Discussion
The present study has highlighted some advantages and disadvantages of BDR relative to PD. BDR was clearly a less invasive procedure than PD, with a shorter duration of surgery, less intraoperative blood loss, less postoperative complications, and a shorter hospital stay. However, disadvantages of BDR included a high rate of R1 resection and less harvested regional lymph nodes.
In general, curative surgery for distal cholangiocarcinoma requires PD. Because of the softness of the pancreatic parenchyma and narrowness of the pancreatic duct, many patients with distal bile duct cancer who underwent PD suffered from postoperative pancreatic fistula (33% -48%) which prolonged the hospital stay [22-24] . However, in the present study, the lesser invasiveness of BDR might have resulted in earlier discharge and then in the administration of adjuvant chemotherapy more often. This may be one of the possible explanations of a comparable prognosis of BDR group to that of PD group. BDR was performed especially often for patients in a poor general condition and was associated with more R1 resection, an independent prognostic factor for bile duct cancer.If these weakened patients had not undergone an operation, they might have been treated by systemic chemotherapy. Previous studies [25 , 26] on systemic chemotherapy for patients with advanced biliary tract cancer reported a median survival time of about 8 months for patients treated with gemcitabine and about 11 months for combined gemcitabine + cisplatin. These results are worse than seen here in the BDR group with R1 resection. Thus, patients with middle bile duct cancer who cannot tolerate PD or hepatectomy may be good candidates for BDR.
One of the disadvantages of BDR was a lower curative effect.However, in advanced extrahepatic cholangiocarcinoma, prognosis following R1cis or R0 resection is known to be similar [14 , 27 , 28] ,and 4 of 13 patients with R1 were able to achieve R1cis resectionin the present study. In our institution, bile duct margin was assessed by intraoperative frozen section analysis. For patients with positive ductal margin, additional bile duct resection was repeatedly performed to achieve R0 status, however some cases finally resulted in positive bile duct margin. Another study reported that R1cis was an independent prognostic factor in early cholangiocarcinoma [14] . With regard to patients with T1 and T2 in the present study, BDR group had more local recurrences than PD group (31% vs. 7%), which maybe came from high rate of R1 resection. However, there was no significance in prognosis between BDR and PD groups.

Table 4Prognostic factors assessed in uni- and multivariate analyses.
In terms of lymph node metastasis, nodal status is welldocumented as a prognostic factor. Several studies [17 , 18 , 29] reported that lymph node metastasis, positive lymph node ratio and lymph node count all had strong prognostic value. A major difference in lymph node dissection between BDR and PD is that the former procedure cannot retrieve a part of the peri-pancreatic lymph nodes (station 13, 17) and all of the superior mesenteric artery lymph node (station 14). In fact, the BDR group had less lymph nodes retrieved in this study, and one third of the patients who underwent PD had positive lymph nodes around the pancreatic head. Therefore, suspected lymph node metastasis in station 14 or 17 should be a contraindication for BDR.
There are some limitations to this study. It is a retrospective study in a single institution, and the BDR group sample size was small. In addition, a major inclusion criterion in the BDR group was a double standard: patients in poor condition and those with cancer confined to the middle bile duct. However, the proportion of BDR to PD was totally similar to other studies (about 20%) [12 , 13] .
In conclusion, BDR is a good option for patients with middle bile duct cancer, especially for those in a poor general condition.
CRediT authorship contribution statement
Masayuki Akita:Conceptualization, Investigation, Writing -original draft.Tetsuo Ajiki:Conceptualization, Supervision, Writing - original draft, Writing - review & editing.Kimihiko Ueno:Formal analysis, Resources, Writing - original draft.Daisuke Tsugawa:Formal analysis, Resources, Writing - original draft.Motofumi Tanaka:Formal analysis, Resources, Writing - original draft.Masahiro Kido:Formal analysis, Resources, Writing - original draft.Hirochika Toyama:Formal analysis, Resources, Writing - original draft.Takumi Fukumoto:Formal analysis, Resources, Writing -original draft.
Funding
None.
Ethical approval
This study was approved by the Ethics Committee of Kobe University Graduate School of Medicine (#180367).
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Neoadjuvant chemoradiotherapy before resection of perihilar cholangiocarcinoma: A systematic review
- Hepatobiliary&Pancreatic Diseases International
- Human microbiome is a diagnostic biomarker in hepatocellular carcinoma
- Current practice of anticoagulant in the treatment of splanchnic vein thrombosis secondary to acute pancreatitis
- Enhanced recovery after surgery program in the patients undergoing hepatectomy for benign liver lesions
- Assessment of biological functions for C3A cells interacting with adverse environments of liver failure plasma