Diagnosis and management strategy of syncope
2019-09-10.
.
[Abstract] Syncope is a common symptom due to various causes, ranging from benign to life-threatening conditions. According to the evaluation and management of patients with syncope, they can be classified as being at short- or long-term risk. Risk stratification during initial evaluation is important for guiding the treatment, and reducing long-term morbidity and mortality. This paper introduces the new progress in the etiology, risk stratification, diagnostic methods and treatment strategies of syncope, and elaborates on the selection of initial assessment tools for syncope patients. In order to elevate the diagnostic accuracy rate of syncope, a systematic and holistic analysis of syncope patients was proposed, including the initial assessment of outpatients and emergency services as well as the observation and treatment during subsequent hospitalization. This paper suggests the management of syncope be considered as a focus, such as establishing syncope management units, taking structured care pathways,etc. Finally, it is suggested to make more efforts in aspects of randomized controlled trials, treatment and collaborative research in the future.
[Key words] syncope; risk stratification; diagnosis; prognosis
1 Syncope causes
In normal situations of medical care, patients do not necessarily come with a convincing history of fainting, but typically come with a history of transient loss of consciousness(TLOC). And consequently, it is a must to ascertain first whether the patient truly loses consciousness rather than assuming it as a syncope event before taking clinical measures. Now there are many situations leading to the loss of consciousness which can be divided into three categories: (ⅰ) those induced by trauma which were not hot spots of discussion at present; (ⅱ) non-trauma related causes, further divided into syncope, intoxications, metabolic disorders,etc.; (ⅲ) false TLOC, a conditions that may be very confusing to practitioners. The most important form, and the most difficult one for practitioners to diagnose and to teach the patient about is psychogenic syncope and seizure disorder. Those situations are true syncope, true seizure or mimics of TLOC, but first and foremost, the true forms of syncope require constant vigilance.
This paper primarily concentrates on the true syncope situations. Syncope is generally divided into neurally-mediated syncope, orthostatic hypotension, arrhythmic syncope and organic heart disease. The classification is just for clinical utility without particular pathophysiological relationship to the conditions. Neurally-mediated syncope is the most common cause in clinic including vasovagal syncope, carotid sinus syndromes and situational syncope(such as cough syncope and swallow syncope). Orthostatic hypotension is very common and it is often iatrogenic, in other words, doctors create this problem by giving medication. How ever, in many cases, it can be fully explained as being based on a neurology underlying condition, such as orthostatic failure syndrome. Clinicians are suggested to be at least somewhat interested in and informed about these underlying conditions in order to both treat the patients and transfer them to an appropriate neurology consultant if necessary. Among arrhythmias giving rise to syncope, there are bradycardia(sinus node disease and atrio-ventricular block), tachycardia(supraventricular tachycardia and ventricular tachycardia) and ion channelopathy. Surprisingly, we found that structural heart diseases such as outflow- and inflow-tract obstruction are relatively uncommon causes of syncope. Embolism is probably one of the most important causes to consider.
In terms of the causes of syncope, they do vary by age. As shown in Fig.1, in young people under the age of 40 and middle-aged group between 40 and 60 years old, the proportion of patients with neurally-mediated syncope is still high; however, with the growth of age, the proportion of patients with orthostatic hypotension or structural heart disease increases[1]. Therefore, the elder population is prone to be attacked by the above two diseases, and is also considered as the key object in clinical evaluation. Clinicians should treat the physical examination seriously, and determine the cause of syncope for the patients at a corresponding age based on the age distribution of syncope causes and their own intuition as cost-effectively as possible.

Cited from reference [1]
2 Risk stratification and prognosis of syncope
Then what is the goal of evaluating these patients with syncope? It sounds obviously unrealistic in clinic to establish the cause of syncope or collapse with sufficient certainty of 100%. The author suggests clinicians to assess the prognosis confidently and to initiate preventive therapy; there is no need for them to make treating attempt unless they are pretty confident of the diagnosis. Establishing the cause of syncope is the substance of the whole evaluation. The treatment thereafter is often self-evident particularly with arrhythmias, not to mention neurally-mediated syncope. The diagnosis aims to determine the cause of syncope or collapse so as to confidently evaluate the prognosis including making risk stratification of recurrence, injury and mortality, educating patients and their families, and initiating effective preventive treatment.
According to the Framingham updated studies[2](Fig.2), those patients with cardiac-cause syncope had poor prognosis. During a follow-up of 15 years, the survival rate of patients with cardiac-cause syncope was lower than that of normal population, and was also lower than that of those with vasovagal syncope and other types of syncope[2]. It should be noted that the prognosis of syncope is not solely related to sudden death, but it may also be related to accident and injury. The patients with sudden death are more likely to fall into cardiac group, but the injury such as occupational hazard may not happen in all groups of syncope patients. The survival rate of patients with cardiac dysfunction is overwhelmingly negative, and therefore its inductive causes and necessary therapies should be focused on in clinical discussion in order to eliminate cardiac dysfunction.
Various academic societies have established diagnostic guidelines or expert consensus statement on the clinical management of syncope. This paper mainly discusses the one adopted from the European Society of Cardiology Task Force on Syncope in which the author fortunately participated for several years. Different from traditional practice, we are in favor of initiating the risk stratification of syncope at the first visit of the patient or when the emergency doctors first see them. Risk stratification would remain to be a research subject unless it has been thoroughly solved. Clinicians could perform a certain risk evaluation on TLOC patients. At present, short-term risk evaluation during one week or one month functions well, but a long-term capacity to assess the risk in those patients is still insufficient. Not every fainting or falling patient requires hospitalization, and therefore consultance and diagnosis are often limited within a short time period, maybe a couple of weeks. Certainly, all the cases with syncope or collapse should be made relatively proper risk evaluation. The flowchart of risk evaluation among patients with suspected syncope is shown in Fig.3[3].
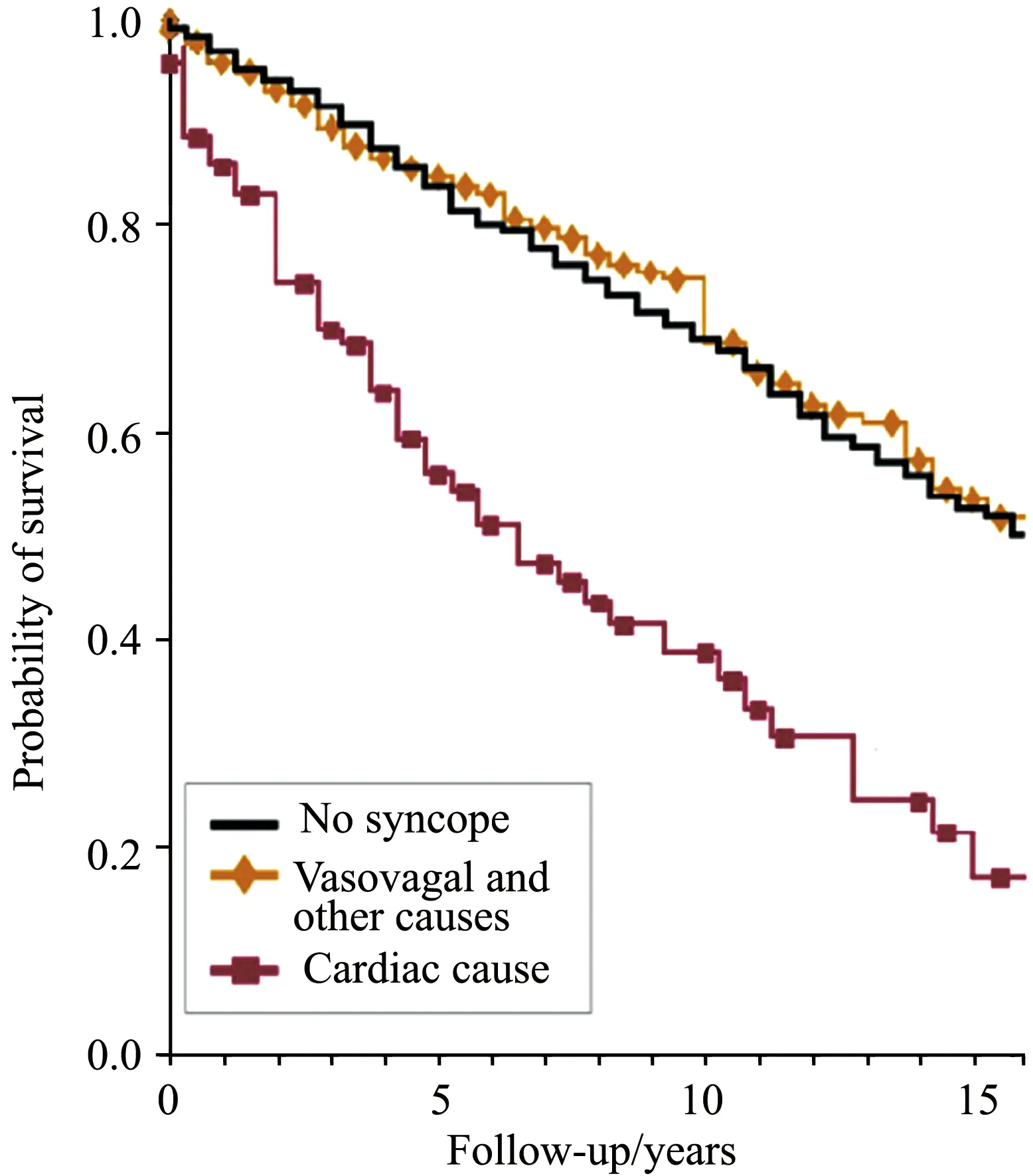
Cited from reference [2]
Certain clinical findings in patients might change the diagnostic or therapeutic plan for syncope. For this reason, it is necessary for us to make risk stratification of syncope patients to determine the necessity for immediate hospitalization and early intensive evaluation, and to clarify the nature of subsequent clinical management. And what is the near-term risk for syncope patients in terms of morbility and mortality? Their near-term risk(up to 30 days after syncope) is related to death rate, injury and recurrence of syncope; long-term risk is difficult to be well-defined, and underlying disease is a major contributor. The near-term prognosis of patients presenting with syncope is mainly related to the cause of syncope and the acute reversibility of the underlying condition; long-term prognosis is related to the effectiveness of therapy, and the severity and progression of underlying diseases, especially cardiac disease or end-stage disease. In clinical practice, the near-term risk evaluation is currently done well, but the long-term risk evaluation is not ideal.
In a meta-analysis carried out by D’Ascenzo F et al[4], the risk indicators or predictors of adverse outcome among syncope population were observed, including palpitations preceeding syncope(Fig.4). Among those falling down in the midst of running, the risk indicators of poor prognosis are extremely high while the risk is low in those fainting after exercise. Each of these findings including the presence of structural heart disease will probably tend to influence doctors’ treatment strategies such as whether the patient should be admit-ted to hospital and whether it is necessary to make initial evaluation after hospitalization. Outpatient evaluation can probably be initiated on the patients without these findings, which in fact could save the healthcare system much money. About 5 billion to 7 billion dollars, not a trivial amount of money, have to be spent on evaluating patients with syncope each year in the USA. By using more sophisticated and more universal risk stratification, the cost can be cut in half. But what kind of findings will push doctors to admit the patient at least as the first step? If a patient has no heart disease, significant ECG abnormality, syncope and severe injury during exercise as mentioned earlier, or social environmental triggers for syncope, they can absolutely take care of themselves at home.
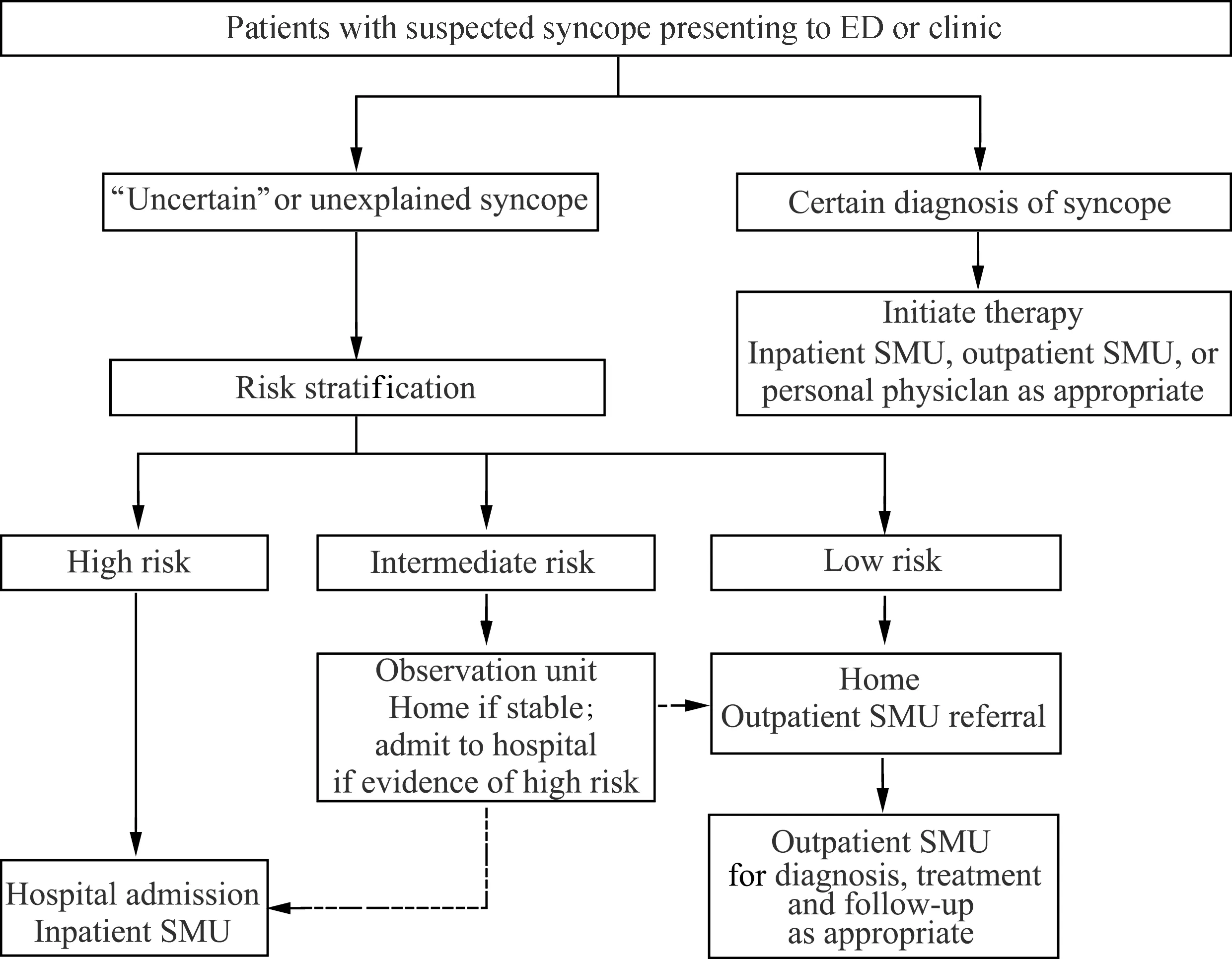
Cited from reference [3]

Cited from reference [4]
3 Diagnostic methods and treatment strategies for syncope
Various auxiliary examinations can be used in the risk evaluation of syncope, but the most important is to understand the detailed medical history before selecting physical examination, ECG, AECG, or further imaging examination(ultrasound, magnetic resonance imaging), electrophysiologic study and video electroencephalogram if appropriate. Syncope or collapse is one of clinical conditions where we strongly recommend a detailed historical query. It will provide us valuable clues to the diagnosis, otherwise we will end up fruitlessly working in the dark.
At present, there are many good diagnostic tools with various types for syncope in clinic. One of them is commonly used in western countries, particularly in the USA. These tools can be utilized at least in looking for causes of arrhythmic syncope or collapse if there is no need for hospitalization based on preliminary judgment. Of course, other types of vital sign monitoring are not open for use. For instance, blood pressure recording is not supportable in the monitoring system currently, but it can be expected to become reality in the near future. Many of these systems can be utilized in the mobile telemetry monitoring which facilitates patients to communicate back arrhythmia ECGs to central station and then to doctors for making interpretation and diagnosis. Among those patients whose symptoms occur not every day or every week, but maybe once or twice a year, implantable monitor functions in the same way as mobile telemetry monitor. Monitoring of these monitors will typically last for three years or more, and it proves to be very valuable in the recognization of infrequent but serious arrhythmias.
Overall, whether it is for family doctors or hospitalists, and whether it is for neurologists or cardiologists, the diagnosis rate of syncope is only about 50%. Benditt et al[5]carried out a sampling survey in the USA and the results are shown in Fig.5. The author participated in another sampling survey in Europe and came out with similar results. In terms of our expectation for evaluating syncope and updating an adequate diagnosis, a diagnosis rate of 50% is obviously far from enough, and therefore, we still have long way to go.

PCP:primary care providers; HOSP:hospitalists; Neuro:neurologists; NIC:non-implanting cardiologists; IC:implanting cardiologists
Arrhythmic syncope turns out to be the easiest to diagnose with pretty good monitors. By using implantable loop recorder(ILR) we can make a diagnosis straightforward: Fig.6A implies atrioventricular block at the lower end of His bundle while Fig.6B suggests polymorphic ventricular tachycardia. Therefore, at the presence of such arrhythmic events captured by the recorder, pacing, ablation or medication may be helpful for these patients based on accurate diagnosis, although there is a vast cohort of syncope patients for whom ideal treatment plan is still unavailable in clinic. For lack of effective monitoring tools, it is difficult for us to monitor neurally-mediated syncope and other related events.
Farwell et al[6]compared the success rate of syncope evaluation between routine ambulatory electrocardiography(AECG) diagnostic monitoring and ILR monitoring. They witnessed a marked improvement in the ability of patients or at least doctors to make diagnosis via ILR versus conventional monitoring. It follows that long-term monitoring in patients not requiring immediate hospitalization is definitely beneficial for making a diagnosis. From the above two trials, it can also be concluded that the curative effect of ILR-based therapy seems better(See Fig.7[7]). This is also one of the subjects of perspective studies at present.
In any research, laboratory testing method should always be selective rather than using every testing method in book. For example, ILR can provide information about whether arrhythmia occurs during syncope. However, there is no need for ILR implantation for a patient already being implanted with a pacemaker or defibrillator since these devices are equiped with function of arrhythmia recording by themselves. If the diagnosis is still unclear after initial evaluation, head-up tilt test(HUTT) may provide an alternative for patients with suspected vasovagal syncope. Referral to the neurology clinic for autonomic function evaluation can be useful to improve the accuracy of diagnosis and prognosis assessment in selected patients with syncope and known or suspected neurodegenerative disease. In a word,all the testing method should be selected on the patient-by-patient basis.
HUTT has certain value in studying patients with neurally-mediated syncope and other autonomic nerve disorders. It should be used selectively. Since the testing results may be difficult to be interpreted sometimes, the manipulator is required to be experienced. As shown in Fig.8, in the induction of vasovagal syncope during HUTT, blood pressure starts to decline at the arrow. The attack of vasovagal syncope during HUTT is fairly classic, but the most important point is whether this observation reproduces the patient’s symptoms? If the patient says yes, then the diagnosis is correct; but if the patient never had that happen before, then the diagnosis is in the wrong direction. Therefore, it is very important to correlate what we have found in the laboratory to the patient’s clinical symptoms on the street. We have to try our best to make that correlation to be 100% and be satisfied with the outcome, even if it is no easy to establish a correlation strong enough between them.
Conventional electrophysiological study has limited use. It is mainly applied in the examination of patients with structural heart disease manifested by syncope or collapse while it is inapplicable to the population without structural heart disease. The correlation between spontaneous fainting symptoms and laboratory testing results has not been affirmed yet at present. Both of long HV interval and inducible ventricular tachycardia require to be further studied.
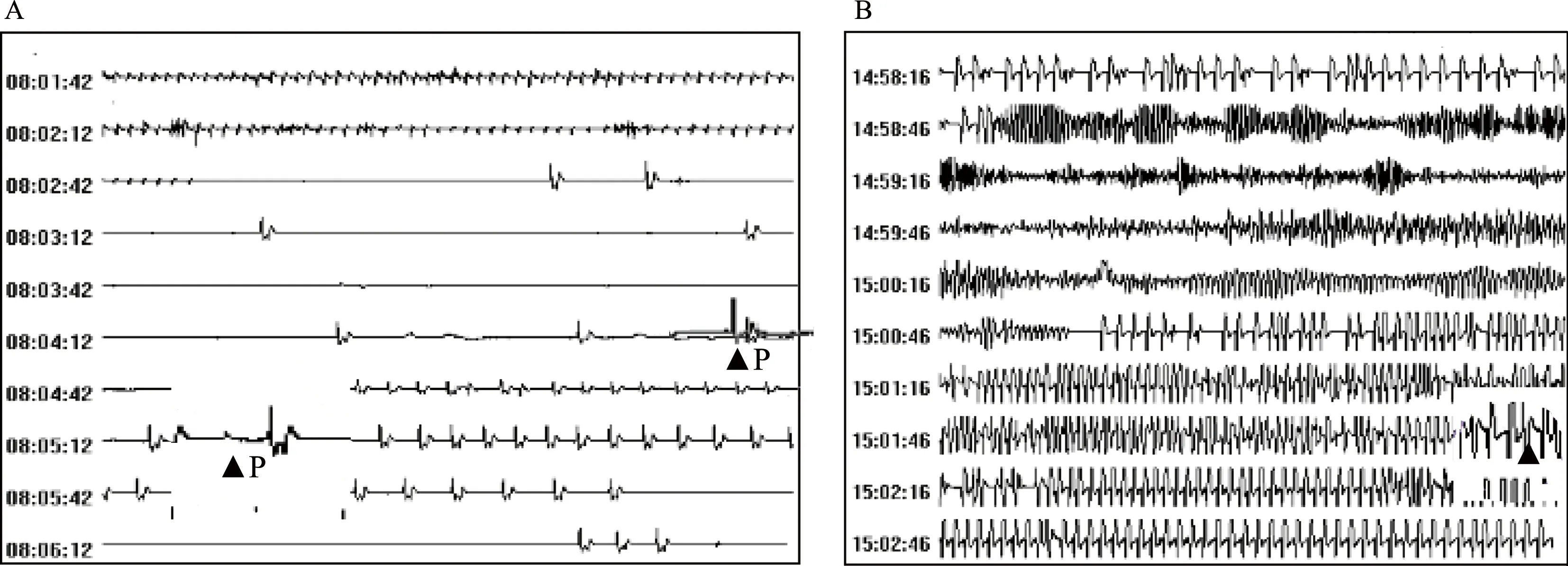
A:infra-Hisian atrioventricular block(implanted with dual chamber pacemaker); the “P” indicates when the patient activated the device; B:ventricular tachycardia and ventricular fibrillation(implanted with ICD); the triangle represents an auto-activated event
图.6ExamplesofECGrecordingsobtainedbytheReveal®ILRsystemin2symptomaticpatients
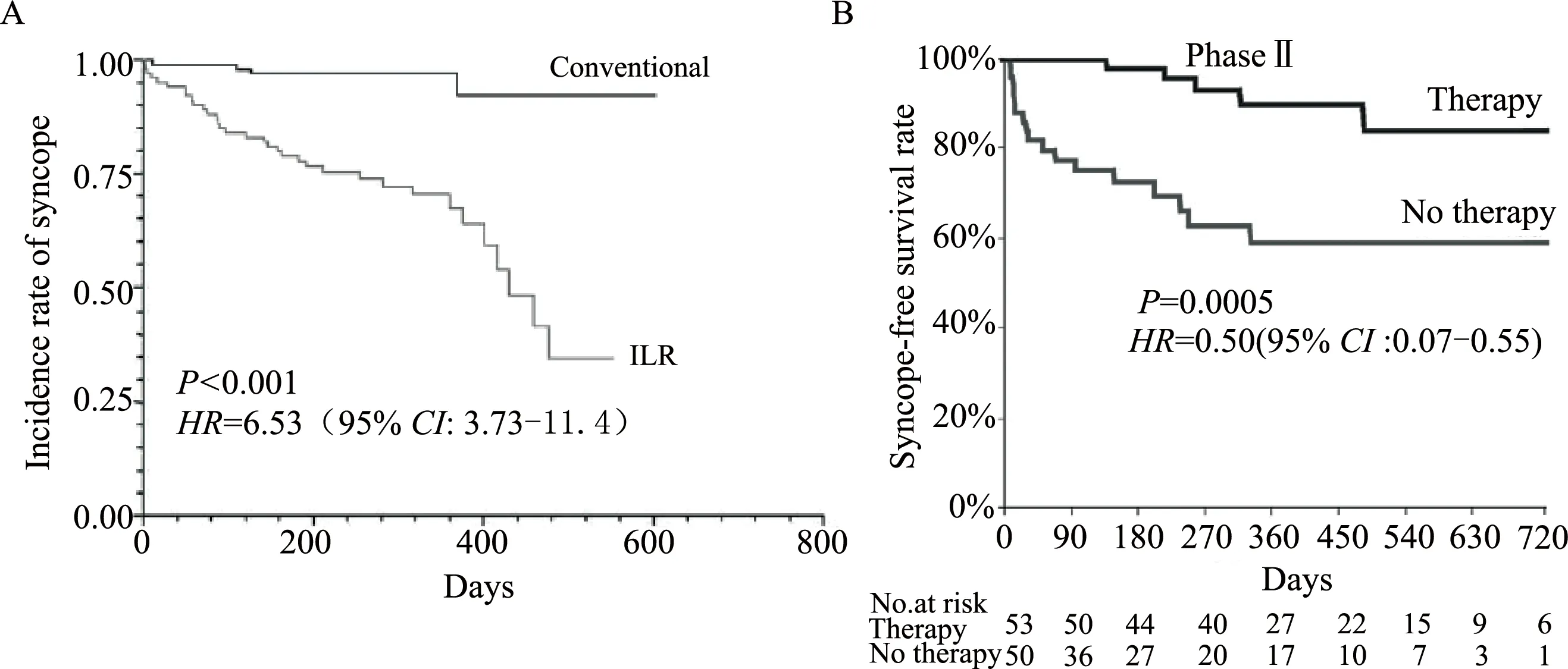
A: Eastbourne Syncope Assessment Study 1(EaSyAS 1)[6]; B: International Study on Syncope of Uncertain Etiology-2 (ISSUE-2), improved outcome with ILR-based therapy[7]

Provided by Wouter Wieling(Department of Internal Medicine, Academic Medical Centre, University of Amsterdam)
4 Future syncope needs
The diagnostic rate of syncope can be improved by taking structured care pathway[8]. It has been very important in the studies in Europe and a number of centers in the United States, especially more recently at the Mayo clinic. With a combination of structured care pathway and abundant clinical experience, we can not only determine the cause of disease, but also can improve the diagnostic rate of syncope drastically. In an EGSYS 2 study from Italy[9], the patients got remarked improvements in a fewer number of hospital days and increased diagnosis rates.
The adoption of structured care pathway or management units are important for the diagnosis and treatment of syncope or collapse in the future. Experienced clinicians are required to apply that technique in medical practice and be skilled in it. Diagnostic techniques do need to be improved, perhaps one of the most important would be the monitoring of blood pressure and ECG. A lot of work we have done in the past is empirical. Studies based on randomized controlled trials should be strengthened because they can provide evidences in all aspects for the diagnosis and treatment of syncope patients.
