高危型子痫前期孕妇行预防性抗凝治疗的相关研究
2019-09-02刘欣茹刘林丽齐碧如
刘欣茹 刘林丽 齐碧如
[摘要] 目的 探討高危型子痫前期孕妇在妊早期后的不同孕周开始口服小剂量阿司匹林抗凝治疗对妊娠期高血压疾病的预防作用。 方法 收集2016年3月~2018年8月我院妇产科门诊及住院病例1131例。根据孕周分成三组:A组(孕13~16周)409例,随机分为实验组(口服拜阿司匹林组(AⅠ组))211例和对照组(口服安慰剂组(AⅡ组)198例;B组(孕16+~20周)404例,随机分为BI组206例和BII组198例;C组(孕20+~24周)318例,随机分为CⅠ组158例和CⅡ组160例,观察孕妇的并发症、妊娠结局及围产儿结局。 结果 口服阿司匹林组的子痫前期、子痫、孕32~34周的早产及低出生体重儿的发生率明显低于对照组,其中阴道分娩率显著高于口服安慰组,差异有统计学意义。孕13~16周开始口服阿司匹林组的子痫前期、子痫、孕32~34周的早产及低出生体重儿的发生率低于16周后开始实验的孕妇,差异有统计学意义(P<0.05)。 结论 口服小剂量阿司匹林对高危型孕妇的子痫前期有干预和预防作用,不增加胎儿出血性疾病的风险,妊娠早期结束后尤其是16周之前开始口服阿司匹林益处更大。
[关键词] 子痫前期;阿司匹林;抗凝治疗;妊娠并发症;围产儿结局
[中图分类号] R714.2 [文献标识码] B [文章编号] 1673-9701(2019)19-0079-05
[Abstract] Objective To investigate the preventive effect of taking low-dose aspirin anticoagulant therapy from different gestational weeks after pregnancy on the prevention of hypertensive disorders of pregnancy in high-risk preeclampsia pregnant women. Methods A total of 1131 obstetrics and gynaecology outpatient and inpatient cases were collected from March 2016 to August 2018. According to the gestational age, they were divided into three groups: 409 patients in group A(13-16 weeks of gestation), who were randomly divided into 211 cases in experimental group(oral aspirin group (AⅠ group) and 198 cases in control group (oral placebo group (AⅡ group); 404 patients in group B (pregnancy 16+-20 weeks), who were randomly divided into 206 cases in BⅠ group and 198 cases in BⅡ group; 318 patients in group C (pregnancy 20+-24 weeks), who were randomly divided into 158 cases in CI group and 160 cases in CII group. The complications, pregnancy outcomes, and perinatal outcomes in pregnant women were observed. Results The incidence of preeclampsia, eclampsia, 32-34 weeks of preterm delivery and low birth weight infants in the oral aspirin group was significantly lower than that in the control group, and the vaginal delivery rate in the oral aspirin group was significantly higher than that in the oral placebo group, with statistically significant difference. The incidence of pre-eclampsia, eclampsia,32-34 weeks of preterm delivery and low birth weight infants in the starting oral aspirin at 13-16 weeks of gestation group was lower than that of the pregnant women who started the experiment after 16 weeks. The difference was statistically significant(P<0.05). Conclusion Oral low-dose aspirin has an intervention and prevention effect on pre-eclampsia in high-risk pregnant women, and does not increase the risk of fetal hemorrhagic disease. The benefit of oral aspirin is greater after the end of pregnancy, especially before 16 weeks.
[Key words] Preeclampsia; Aspirin; Anticoagulant therapy; Pregnancy complications; Perinatal outcomes
妊娠期高血压疾病严重威胁母婴健康,积极防治妊娠期高血压疾病是高危妊娠管理的重要任务。该病患者伴有一定量的凝血因子缺乏或变异所致的高凝血状态[1]。目前尚缺乏有效方法对高危人群进行预防和治疗。近年来,有研究表明小剂量阿司匹林抗凝治疗改变妊高症患者的高凝状态,促进胎盘灌注,改善妊娠结局[2]。本文通过前瞻性分析1131例高危型子痫前期患者的临床资料,分别记录不同孕周用药,高危孕妇的妊娠并发症、妊娠结局及新生儿情况,现报道如下。
1 资料与方法
1.1 一般资料
选取2016年3月~2018年8月就诊于我院妇产科门诊、孕周13~24周、存在子痫前期高危因素暴露的孕妇纳入研究。至少符合以下1个纳入标准:慢性高血压(伴或不伴有肾病;舒张压在90~110 mmHg);既往子痫史;既往妊娠期高血压病史;糖尿病史;肾脏疾病;羊水过多;羊水过少;肥胖;高脂血症;生育年龄过大(>35岁);距上次妊娠时间大于10年;多次妊娠史;有自身免疫性疾病病史;葡萄胎史。当同一个患者符合2个或以上标准时,医师必须确定该孕妇与哪一个指标最相关。排除标准:慢性病史(不包括高血压、肾脏疾病、不合并高血压和肾病的慢性糖尿病);在其他单位分娩;较严重的胎儿畸形;孕期抗凝治疗;已经参加其他预防子痫前期的研究。本研究征得本院伦理委员会同意,患者均签署知情同意书。
1.2 方法
根据不同孕周,先分为A组(孕13~16周)、B组(孕16+~20周)和C组(孕20+~24周),再根据随机原则,将A组孕妇随机分为AⅠ組(阿司匹林组)和AⅡ组(对照组);将B组孕妇随机分为BⅠ组(阿司匹林组)和BⅡ组(对照组);将C组孕妇随机分为CI组(阿司匹林组)和CII组(对照组)。阿司匹林组选用肠溶剂型(德国拜耳公司,国药准字J20130078,每粒75 mg,每天一次,每次口服75 mg,直至分娩;每天固定时间口服;对照组则以安慰剂替代(白色糖衣淀粉药片,由德国拜耳公司生产,剂型和服用方法均同阿司匹林)。
1.3 观察指标
纳入孕妇正规产检,根据病情变化增加产检次数。记录孕妇血尿常规、24 h尿蛋白、凝血功能、肝肾功能及产科超声等指标。同时记录分娩孕周及分娩方式、胎儿体重及出生时Apgar评分、孕期出现的早产、子痫前期、子痫、胎盘早剥等并发症等。其中Apgar评分是孩子出生后根据皮肤颜色、心搏速率、呼吸、肌张力及运动、反射五项体征进行评分。满10分者为正常新生儿,评分7分以下的新生儿考虑患有轻度窒息,评分在4分以下考虑患有重度窒息[28]。
1.4 统计学分析
采用SPSS19.0软件进行数据的统计与分析,用Kolmogorov-Smirnov test检验连续变量分布的正态性。连续计量资料采用(x±s)表示,两组间比较采用t检验,多组间比较采用ANOVA等。计数资料采用率表示,采用χ2检验,多组比较采用R×C χ2检验和Fisher确切概率法χ2检验等。P<0.05为差异有统计学意义。
2 结果
2.1 孕妇基本资料
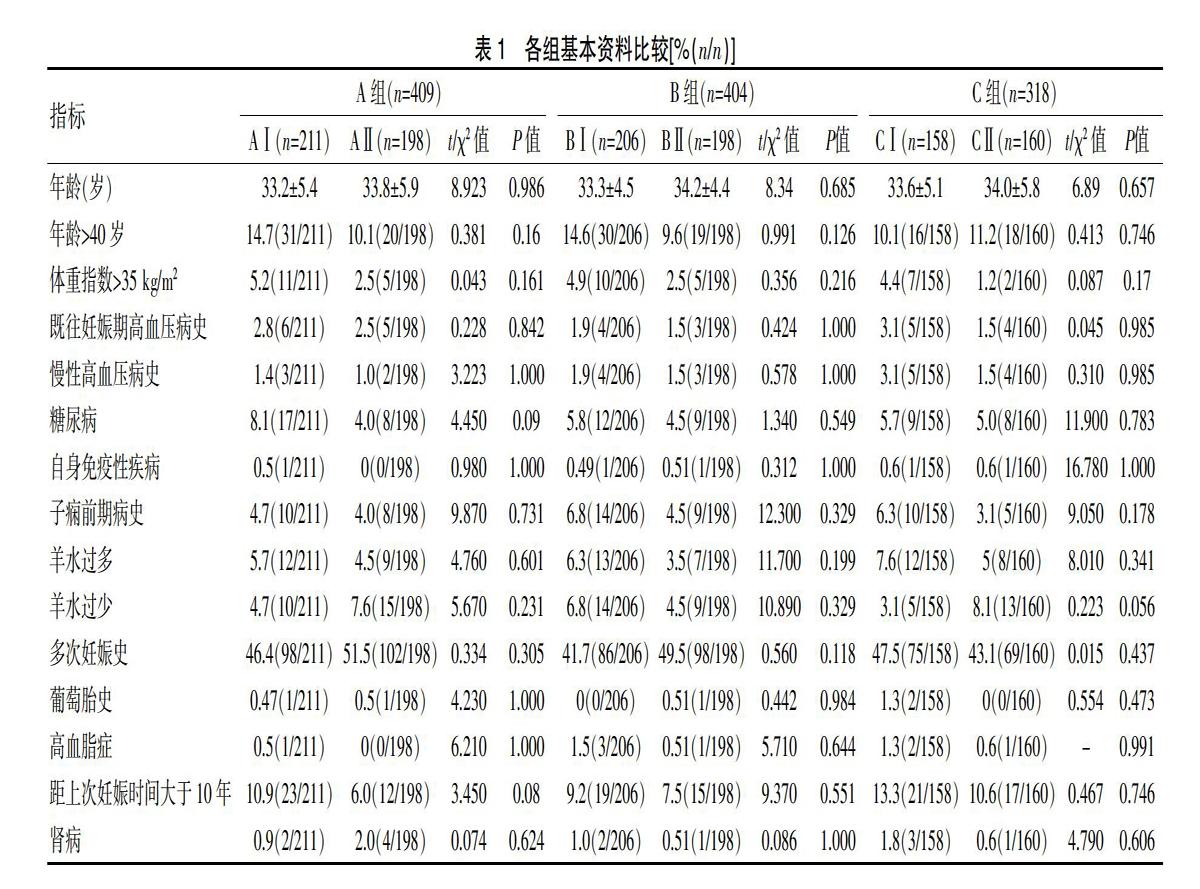
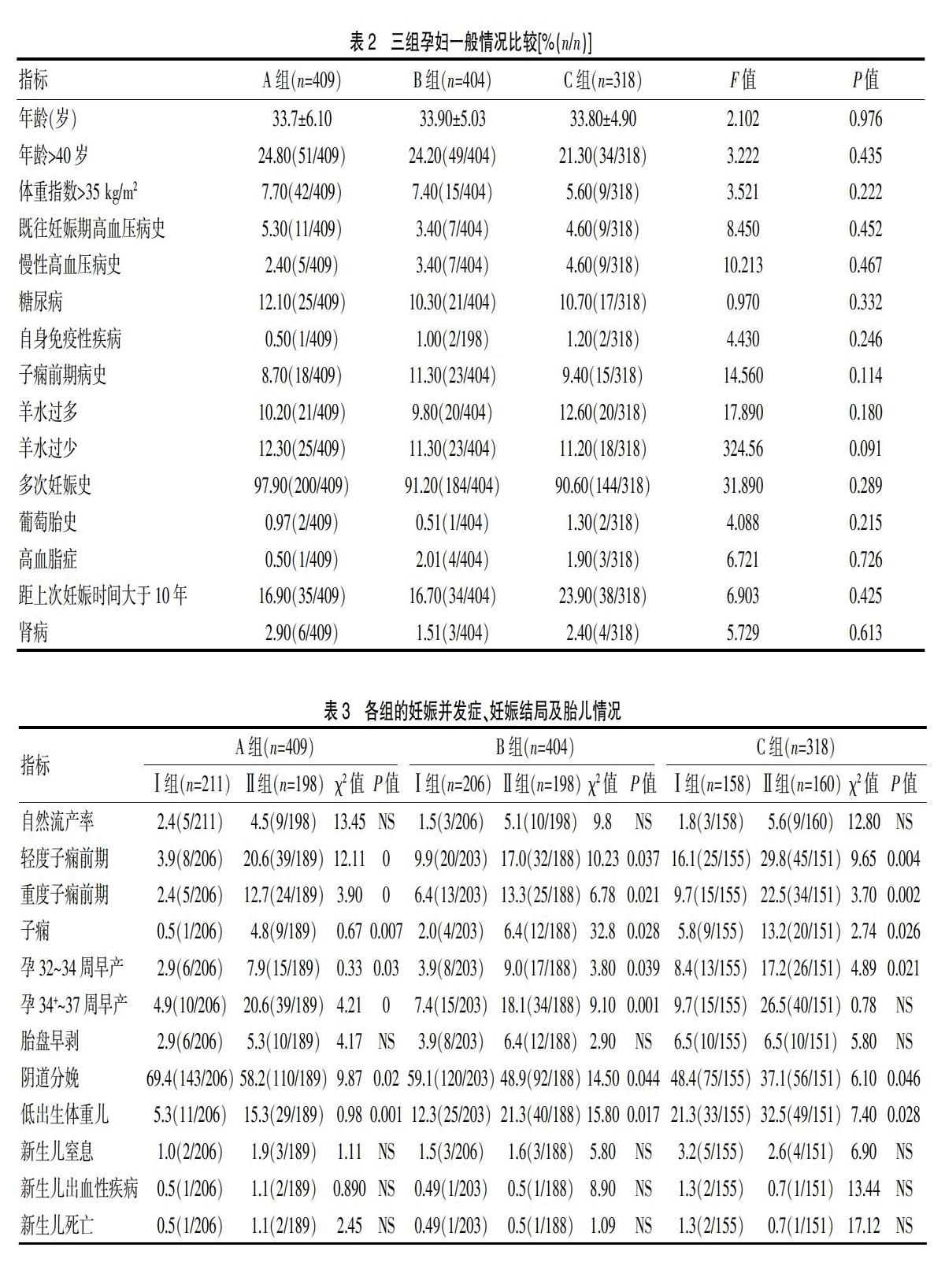
本研究所有调查者年龄介于21~46岁,约1/13肥胖、1/7高龄,无长期吸烟及吸毒史者。A、B、C三组孕妇一般情况比较,差异无统计学意义(P>0.05);且AⅠ和AⅡ;BⅠ和BⅡ;CⅠ和CⅡ各组内比较孕妇一般资料也无统计学差异。见表1、2。
2.2 各组的妊娠并发症、妊娠结局及胎儿情况
不同孕周组别间显示服用阿司匹林组子痫前期、子痫的发生率均低于对照组。出生孕周32~34周及<37周孕妇例数少于对照组,除CI组孕妇外,其余两组差异均有统计学意义(P<0.05)。三组中口服阿司匹林孕妇的阴道分娩率也是显著高于对应的安慰剂组,而低出生体重儿例数,所有阿司匹林组是明显少于对照组(P<0.05)。见表3。
本研究数据显示AⅠ、BⅠ两组阿司匹林组胎盘早剥的发生例数低于其对照组,但差异无统计学意义,而CI组中口服阿司匹林组胎盘早剥发生率与对照组一样。故未发现孕早期口服阿司匹林增加胎盘早剥的发生(表3)。阿司匹林组自然流产率、新生儿出血性疾病发生率、新生儿窒息发生率、围产儿死亡率与对照组均无统计学意义(P>0.05)。
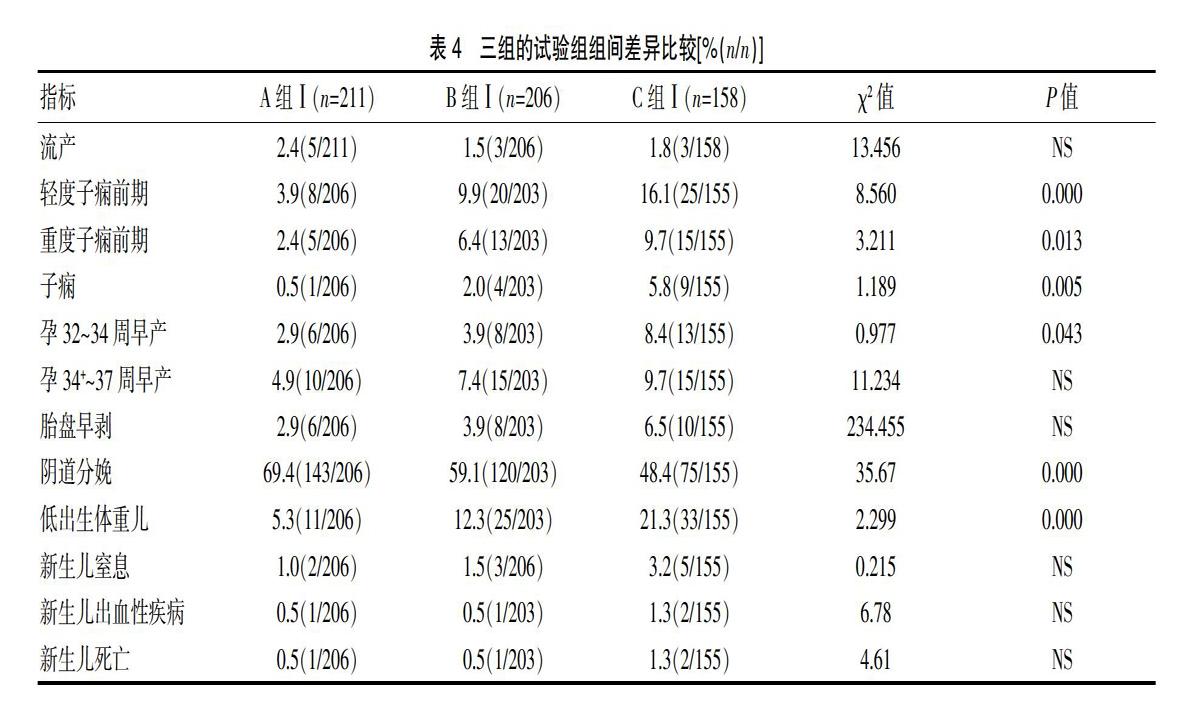
2.3 三组的试验组组间差异比较
A组Ⅰ、B组Ⅰ、C组Ⅰ组间各高高危因素间比较差异无统计学意义(P>0.05)。对于孕13~16周开始口服阿司匹林的孕妇,其子痫前期、子痫、早产及低出生体重儿发生率显著低于孕16~24周实验者。而阴道分娩率显著高于孕16~24周实验组。三组间胎盘早剥、自然流产率、新生儿出血性疾病发生率、新生儿窒息发生率、新生儿死亡率与对照组均无统计学意义(P>0.05)。见表4。
3 讨论
妊娠期高血压疾病对母婴危害极大,但其发病机制尚不明确。目前普遍认为主要是血管内皮细胞受损与血管活性物质失衡,凝血与纤溶平衡失调,可发生妊娠后果[1]。而阿司匹林能阻止血小板聚集和粘附,改善血液高凝状态[2],改善胎盘灌注[3],这就为选用阿司匹林抗凝治疗奠定了基础。
早在1978年有学者提出阿司匹林用于治疗复发性妊娠期高血压疾病,却因其不能预防子痫前期的发生[4],以及可能增加产后出血、胎盘早盘及新生儿颅内出血等风险而被否认[5,9,10,11],近年来,大量数据显示高危孕妇使用小剂量阿司匹林,其子痫前期的发病率降低同时不增加出血疾病风险[6-8]。我们推测阿司匹林有效地降低了妊娠诱发的高血压,与其本身增加胎盘早剥的作用效应抵消。Duley等随机对照试验中显示每天口服75 mg阿司匹林安全的同时可降低子痫前期的发病率,并不增加孕妇妊娠相关出血[12],可能是因为阿司匹林选择性抑制母血的血小板环氧合酶,如果提高剂量可能会增加疗效,其药物不良反应也会随之增加,故本研究选择75 mg口服剂量。结果显示,口服阿司匹林组的三组孕妇的新生儿窒息、新生儿死亡及新生儿出血性疾病的发生率同对照组相比,均无差异,与Askie LM[13]研究结果相一致。阿司匹林能够预防妊高症的发生,避免了因高血压等引起胎盘功能不良,扩张血管,降低周围循环阻力,改善胎儿的能量供应,从而预防了不良结局的发生。
近年来,各个学者对阿司匹林的用药时机各抒己见,有的学者认为确认妊娠后即开始使用,还有的学者则以16周或者20周为界,在此之前应用效果显著[14-22],本文为预防阿司匹林孕12周前致畸作用和影响胎盘形成,提倡孕13周以后进行预防干预,并扩大研究窗口,分别探讨了孕16+~20周及孕20+~24周开始服用阿司匹林孕妇及围产儿并发症的情况。结果显示孕13周后24周前,口服阿司匹林子痫前期、子痫、孕32~34周的早产及低出生体重儿的发生率明显低于对照组,其中阴道分娩率显著高于对照组。Stephanied等和Suzanne等[23-24]研究结论均支持本研究结果。同时我们还发现早孕结束后16周前服用的效果更加显著,A组Ⅰ的子癇前期、子痫、孕32~34周的早产及低出生体重儿的发生率低于16周后开始实验是孕妇,而阴道分娩率也显著高于B组Ⅰ及C组Ⅰ,差异有统计学意义。这可能是13周阿司匹林的干预使胎盘绒毛血管及绒毛间隙组织变薄,血流阻力下降,有利于胎儿生长发育[25]。妊娠期高血压疾病指南中建议高危孕妇在早孕期13周后尽快口服阿司匹林预防子痫前期的发生[26,27],因此本研究结果基本符合了指南用药时机的选择。
综上所述,我们认为高危型子痫前期孕妇口服小剂量阿司匹林能有效预防先兆子痫,而且安全可靠,不增加孕妇及新生儿出血性疾病的危险,同时增加了阴道分娩率,所以我们建议在孕13+~24周产检过程中,如发现为高危孕妇,应积极常规给予小剂量阿司匹林,特别是在13周后即开始[28]。考虑阿司匹林对凝血时间的影响,有加大围产期的出血风险,故对服用阿司匹林的孕妇,要定期检测其凝血功能,防止分娩过程中大出血的发生。
[参考文献]
[1] Kadyrov M,Kingdom JC,Huppertz B.Divergent trophoblast Invasion and apoptosis in placental bed spiral arteries from pregnancies complicated by maternalanemia and early-onse preeclampsia/intrauterine growth restriction[J] Am J Obstet Gynecol,2006,194(2):557-563.
[2] 刘敏,卢新,徐鸿雁.孕妇血清游离β-HCG 水平与早发型重度子痫前期的关系分析[J].中国优生与遗传杂志,2010,18(12):73-74.
[3] Rey E,Rivard GE.Is testing for aspirin response worthwhile in high-risk pregnancy[J].Eur J Obstet Gynecol Reprod Biol,2011,157(1):38-42.
[4] Rodrigo Ruano,Rosana S.Fontes,Marcelo Zugaib.Perwention of pre-eclampsia with L low-dose apirin-a ssystematic review and meta-analysis of the main randomized controlled trials[J].J Clinics,2005,60(5):407-414.
[5] De Berardis G,Lucisano G,DEttorre A,et al.Association of aspirin use with major bleedings in patients with and without diabetes[J].JAMA,2012,3(7): 2286-2294.
[6] Askie LM,Duley L,Henderson-Smart DJ,et al. Antiplateletagents for prevention of pre-eclampsia:A meta-analysis of indi vidual patient data[J].Lancet,2007,369(95):1791-1798.
[7] Marret S,Marchand L,Kaminski M,et al. Prenatal low-dose aspirin and neurobehavioral outcomes of children born very preterm[J].Pediatrics,2010,125(1):29-34.
[8] Hauth J,Cunningham F.Williams Obstetrics Supplement[J].1999,19(3):44-49.
[9] Barton JR,Witlin AG,Sibai BM.Management of mild preeclampsia[J].Clin Obstet Gynecol,1999,42(3):455-469.
[10] Witlin AG,Friedman SA,Sibai BM. The effect of magnesium sulfate therapy on the duration of labor in women with mild preeclampsia at term:A randomized, double-blind,placebo-controlled trial[J]. Am J Obstet Gynecol,1997,176(3):623-627.
[11] Xiang Hong Qin.Low-dose apirin preventing pre-eclampsia[J].New engl J Med,2013,34(17):1213-1221.
[12] Duley L,Henderson-Smart DJ,Meher S,et al.Antiplatelet agents for preventing pre-eclampsia and its complications[J].Cochrane Database Syst Rev,2007,18(2):341-347.
[13] Askie LM,Duley L,Henderson-Smart DJ,et al. Antiplatelet agents for prevention of pre-eclampsia:A meta-analysiso find Ividual Patient data[J]. Lancet,2007, 369(9):1791-1798.
[14] Wallenburg HC,Dekker GA,Makovitz JW,et al. Low-dose aspirin prevents pregnancy-induced hypertension and pre-eclampsia in angiotensin-sensitive primigravidae[J]. Lancet,1986,1(8471):1-3.
[15] Norgard B,Puho E,Czeizel AE,et al. Aspirin use duringearly pregnancy and the risk of congenital abnormalities:Apopulation-based case-control study[J]. Am J Obstet Gynecol,2005,192(3):922-923.
[16] Duley L,Henderson-smart DJ,Meher S,et al.Antiplatelet agents for preventing pre-eclampsia and its complications[J].Cochrane Database Syst Rev,2007(2):CD004659.
[17] Beaufils M,et.Prevention of preeclampsia by early antiplatelet therapy[J].Lancet,1985,1(33):843-840.
[18] Rossi AC,Mullin PM. Prevention of pre-eclampsia with low-dose aspirin or vitamins C and E in women at high or low risk:A systematic review with meta-analysis[J]. Eur J Obstet Gynecol Reprod Biol,2011,158(1):9-16.
[19] Marret S,Marchand L,Kaminski M,et al. Prenatal low-dose aspirin and neurobehavioral outcomes of children born very preterm[J]. Pediatrics,2010,125(1):e29-e34.
[20] Buiold E,Roberge s,Lacase Y,et al.Prevention of preeclampsia and intrauterine growth restriction wuih aspirin started in early pregnancy:a meta-analysis[J].Obstet Gynecol,2010,116(21):402-414.
[21] Buiold E, Prevention of pre-eclampsia with low dose aspirin[J].J postgrad Med,2011,57(2):89-90.
[22] Duley L,Henderson-Smart DJ,Meher S,et al. Antiplateletagents for preventing pre-eclampsia and its complications[J].Cochrane Database Syst Rev,2007,18(2):341-347.
[23] Stephanied Roberge,MSc;Suzanne Demers,MD;Emmanuel Bujold, MD, MSc;Universite' Laval;Que 'bec,Canada. Low-Dose Aspirin for Prevention of Morbidity and Mortality From Preeclampsia[J]. Annals of Internal Medicine,2014,161(8):613-616.
[24] Suzanne Demers,Ste 'phanie Roberge,Emmanuel Bujold.Low-dose aspirin for the prevention of adverse pregnancy outcomes inwomen with elevated alpha-fetoprotein[J]. J Matern Fetal Neonatal Med,2014,12(25):1476-7058.
[25] Panagiota Pietri,Charalambos,Vlachopoulos,et al.Beneficial effects of low-dose aspirin on aortic stiffness in hypertensive patients[J]. J Vascular Medicine,2014,19(6):452-457.
[26] Friedman AM,Cleary KL.Prediction and prevention of ischemic placental disease[J]. Semin Perinatol,2014,38(3):177-182.
[27] Redman CWG.Hypertension in pregnancy:The NICE guidelines[J]. Heart,2011,97(23):1967-1969.
[28] 邵肖梅,葉鸿瑁,丘小汕.实用新生儿学[M].北京:人民卫生出版社,2011:222-225.
(收稿日期:2019-03-01)
