Mesenchymal stem cells, implications for pain therapy
2019-07-18ElenaTrallori,CarlaGhelardini,LorenzoDiCesareMannelli
History and biology of mesenchymal stem cell (MSC):
MSCs were firstly described around 1970s by Friedenstein and his collaborators as a subpopulation of colony forming,clonogenic, plastic adherent stromal bone marrow derived cells, with the capacity to regenerate other tissues (Murphy et al., 2013). Caplan (1991) proposed that these mesenchymal cells were “stem” because of their ability to differentiate to any lineage of mesodermal cells. The richest sources of MSCs are bone marrow and adipose tissue, but they can also be isolated from synovial fluid, periosteum, fetal organs, placenta, umbilical cord blood and amniotic fluid (Murphy et al., 2013; Sherman et al., 2015).
MSCs therapeutic use:MSCs were initially studied and therapeutically proposed only for regenerative aims, due to their differentiation competence, but new correlated functionalities have been recently gaining ground: cell-delivery system and paracrine activity (Brini et al., 2017). Regarding the first function, MSC homing ability is exploited to modulate the release of growth factors and cytokines at the desired site and, moreover, MSCs can be bioengineered by insertion of nucleic acid sequences (e.g., messenger RNA and noncoding RNA), drugs or oncolytic viruses (e.g., myxoma virus to kill glioblastoma cells), to deliver their content to inflammatory areas or tumours, where they can produce or release therapeutic molecules (Sherman et al., 2015). Paracrine activity is linked to the cell-delivery system: the “paracrine hypothesis” states that MSCs are mostly effective through their secretome, which contains trophic, anti-inflammatory,immunomodulatory and antiapoptotic molecules, such as fibroblast growth factor, vascular endothelial growth factor(VEGF)-A, nerve growth factor, transforming growth factor-β and interleukin-10 (Murphy et al., 2013; Zhou et al.,2016; Brini et al., 2017). By virtue of these qualities, MSCs have been investigated as a valid treatment against several pathologies, among which the socially relevant painful neuropathies: cellular therapy would stimulate tissue repair and act paracrinely on inflammation, immune system and nervous system signaling (Brini et al., 2017; Di Cesare Mannelli et al., 2018).
Chronic pain:Chronic pain is a major public health problem which has detrimental effects on economic and social issues: in the USA, it hits more than 100 million people and it costs more than $635 million per year. Pain is inter-related to biological, psychological and social issues which, in turn,affect quality of patients' life. It often worsens social interactions, reduces leisure activities and limits family contacts. It is bidirectionally linked to low physical activity and to the absence of sleep, which in turn negatively influences the psychological mood of the patient. In the economic framework,chronic pain produces high prolonged costs for the health care system and an extended use of primary resources from it; besides, patients' absenteeism from their job may drop the outcome of the company. Neuropathies generally goes together with chronic pain, which in this case is usually treated by antidepressants, antiepileptics and opioids. Opioids misuse and abuse is causing, especially in the USA, drug tolerance and drug-induced hyperalgesia; while the other two lines of medication are limitedly effective. Therefore, there is an urgent need for new treatments and MSCs appeared to be a valid alternative to the existing ones (Dueñas et al., 2016;Hua et al., 2016).
MSC-based treatment and neuropathic pain:Currently,rationalization of MSC-based therapy is being guided by the “paracrine hypothesis”: several studies, carried out on neuropathic pain induced by sciatic nerve ligation, reported that MSC-derived molecules reduce astrocyte reactivity and modulate microglia phenotype switching to an anti-inflammatory M2 behaviour; other papers on diabetic neuropathy proved that MSC secretome is able to significantly lessen neuroinflammation and to restore inflammatory cytokines and signaling molecules balance (Brini et al., 2017; Mukhamedshina et al., 2019). The modulating capability of MSC was one of the focal points raised by our recent study on rat adipose-derived stem cells (rASCs)-based therapy to treat oxaliplatin-induced neuropathic pain in rats (Di Cesare Mannelli et al., 2018); to our knowledge, the first work to prove the efficacy of MSC-based treatments in the field of chemotherapy-induced neuropathy. Intravenous administration of rASCs (2 × 106cells) improved hyperalgesia and allodynia: a 5-day long analgesic effect which was replied also by sustained injections. A strongly positive result was obtained also by intrathecal injections, indicating rASCs modulation of pain perception at central nervous system level. rASCs conditioned medium alone did not ameliorate the hypersensitive state of oxaliplatin-treated rats, thus suggesting the necessary presence of stem cells to exert their anti-nociceptive effect. As mentioned above, MSCs represent a source of signaling molecules, cytokines and growth factors, some of which are correlated to pain modulation and neuroprotection, like the VEGF-A (Zhou et al., 2016). We reported that VEGF-A increased in plasma of oxaliplatin-treated rats and rASCs injections resulted in a strong reduction of its plasmatic levels; we also observed that rASC injections brought down pan-VEGF-A and isoform VEGF165b levels, which were altered in plasma and spinal cord of treated animals,respectively. Moreover, the isoform VEGF165b itself, when injected peripherally, showed a pro-algesic effect, while antibody-mediated blockage of VEGF-A or VEGF165b produced an opposite outcome. Our data confirmed the use of MSCs as a novel mechanism of modulation of surrounding cells activity and proposed VEGF-A signaling as a new target for pain relief (Figure 1).
Conclusions - pros and cons of MSC therapeutic use:Cellular therapy by MSCs shows many positive aspects:immunosuppressive action which reduces allogeneic lymphocyte response in case of transplantation; minimal ethical concerns; a wide number of tissues to collect MSCs from; an easy in vitro expansion; the ability to autonomously reach the sites of inflammation, due to the expression of chemotactic receptors, where they stimulate tissue repair, release therapeutic molecules or modulate the release of molecules from surrounding cells. Next to the advantages which these putative therapeutic agents have, there are also drawbacks which should be carefully debated and confounding factors which need to be elucidated. First, technical aspects of the experimental studies on this therapeutic tool: the lack of MSCs tracking techniques in humans and, as a result, the consequent difficulties in understanding the fate of the exogenous stem cells and the consequent toxic potential; the absence of common agreement on the isolation method, as many laboratories have their own home-made protocols;different methods of stem cells injection; the correlation of MSC source to a single type of disease or to any of them;the differentiation stage, e.g., a multipotent cell will live longer than a partly differentiated, which will rapidly undergo senescence. Second, issues referring to the therapeutic application itself: different sources of MSCs may correspond to different capabilities; in vitro expansion may lead to accumulation of genetic mutations which could result in cancerogenesis, even if there is no reported case of transformation occurred in vitro (Sherman et al., 2015). In conclusion,this promising therapeutic approach still needs some work around it, to answer these unsolved issues and to ameliorate its use, to exploit it in the most profitable way.
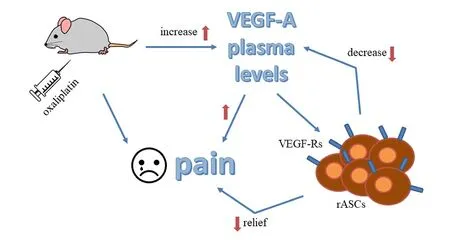
Figure 1 VEGF-A mechanism inchemotherapy-induced neuropathic pain modulation.VEGF-A: Vascular endothelial growth factor A; VEGF-R: VEGF receptor;rASCs: rat adipose-derived stem cells.
Elena Trallori, Carla Ghelardini, Lorenzo Di Cesare Mannelli*Dipartimento di Neuroscienze, Psicologia, Area del Farmaco e Salute del Bambino - Neurofarba - Sezione di Farmacologia e Tossicologia, Università degli Studi di Firenze, Florence, Italy
*Correspondence to: Lorenzo Di Cesare Mannelli, PhD,lorenzo.mannelli@unifi.it.
orcid: 0000-0001-8374-4432 (Lorenzo Di Cesare Mannelli)
Received: February 1, 2019
Accepted: May 14, 2019
doi: 10.4103/1673-5374.259615
Copyright license agreement:The Copyright License Agreement has been signed by all authors before publication.
Plagiarism check:Checked twice by iThenticate.
Peer review: Externally peer reviewed.
Open access statement:This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
Open peer reviewer:Tharkika Nagendran, University of North Carolina at Chapel Hill, USA.
Additional file:Open peer review report 1.
杂志排行
中国神经再生研究(英文版)的其它文章
- Etomidate affects the anti-oxidant pathway to protect retinal ganglion cells after optic nerve transection
- Normal tension glaucoma: from the brain to the eye or the inverse?
- Mesenchymal stromal cell therapy for damaged retinal ganglion cells, is gold all that glitters?
- MicroRNAs as biomarkers of diabetic retinopathy and disease progression
- Diabetic neuropathy research: from mouse models to targets for treatment
- Potential therapeutic roles of retinoids for prevention of neuroinflammation and neurodegeneration in Alzheimer's disease
