Tuberculous esophagomediastinal fistula with concomitant mediastinal bronchial artery aneurysm-acute upper gastrointestinal bleeding: A case report
2019-05-13SultanAlharbi
Sultan R Alharbi
Abstra c t
Key words: Mediastinal bronchial artery aneurysm; Esophagomediastinal fistula; Upper gastrointestinal bleeding; Mediastinal tuberculosis; Case report
INTRODUCTION
M ed iastinal tubercu losis (TB) lym phadenitis is a rare clinical m anifestation of TB in adu lts, and it usually occu rs secondary to pu lm onary TB. Extrapu lm onary lym ph node TB was reported to be 17.6% o f all TB cases[1]. Esophagom ed iastinal fistu la form ation secondary to m ediastinal TB lym phadenitis is an unusual com p lication that develops as a consequence of erosion of ad jacen t organs[2]. M ed iastinal bronchial artery aneu rysm s are extrem ely rare and can be id iopathic or secondary. Secondary aneu rysm s are usually related to an underly ing in flamm atory p rocess like bronchiectasis, chronic bronchitis, or system ic vascu lar d isease[3,4]. Bronchial artery aneu rysm w ith an esophageal fistu la is an extrem ely rare and poten tially fatal d iagnosis, and there are few case reports in literatu re[5].
CASE PRESENTATION
A 19-year-old m ed ically free patient p resented to ou r em ergency departm ent w ith 1-d histo ry o f 5 ep isodes o f hem atem esis w ith m oderate am oun t associated w ith ep igastric pain. H is m ed ical history is significan t for ch ronic cough w ith occasional hem op tysis and w eight loss for 5 m o. H is vital signs are stable. Patient was pale, bu t there was no jaund ice or cyanosis. Chest and abd om inal exam inations are unrem arkable. Laboratory investigations show norm al resu lts excep t low hem oglobin level of 8 g/d L. Tw o units of packed red blood cells (PRBCs) w ere transfused. Upper gastrointestinal (GI) endoscopy show s an opening in the m id-esophagus w ithout clot,bleed ing, or m ucosal lesions, otherw ise a norm al esophagus, stom ach, and duodenum(Figu re 1). Tracheoesophageal fistu la was suspected, and no defin ite sou rce o f bleed ing was identified.
Bronchoscopy was perform ed and show ed no tracheoesophageal fistu la bu t edem atous m ucosa w ith nodu lar lesions in the left low er lobe bronchus. Biopsy was perform ed. Initial chest X-ray show s cavitary left lung lesion. Three spu tum sam p les w ere sen t for Zieh l-Neelsen (ZN) staining and w ere negative. Chest com pu ted tom og raphy (CT) w ith IV con trast was perfo rm ed and show ed ev idence o f esophagom ed iastinal fistu la, m u ltip le necrotic m ed iastinal lym ph nodes, cavitary lung lesion, and tw o sm all m ed iastinal bronchial artery aneu rysm s ind icating pu lm onary and m ed iastinum TB (Figu re 2). Patien t had ano ther ep isode o f hem atem esis w ith m oderate am oun t. Up per GI endoscopy was repeated and un rem arkable excep t a sm all opening in the m id-esophagus. Another tw o units o f PRBC w ere transfused. Conven tional angiography was perform ed and show ed bronchial artery arising from the left subclavian artery w ith tw o sm all m ed iastinal bronchial artery aneu rysm s. Em bolization was perform ed using coils (Figu re 3).H istopathological resu lts o f bronchial biopsy show ed necrotizing granu lom atous in flamm ation suggesting TB, and tw o add itional spu tum sam p les w ere sent for ZN staining and w ere positive. An ti-TB m ed ication was started. Patien t d id not have hem atem esis or m elena after em bolization. Patient was d ischarged in good cond ition w ith an ti-TB m ed ications. A t 3-m o of follow-up, patient was asym p tom atic and had no ep isode of GI bleed ing. Follow-up chest X-ray show s interval im p rovem ent (Figure 4).
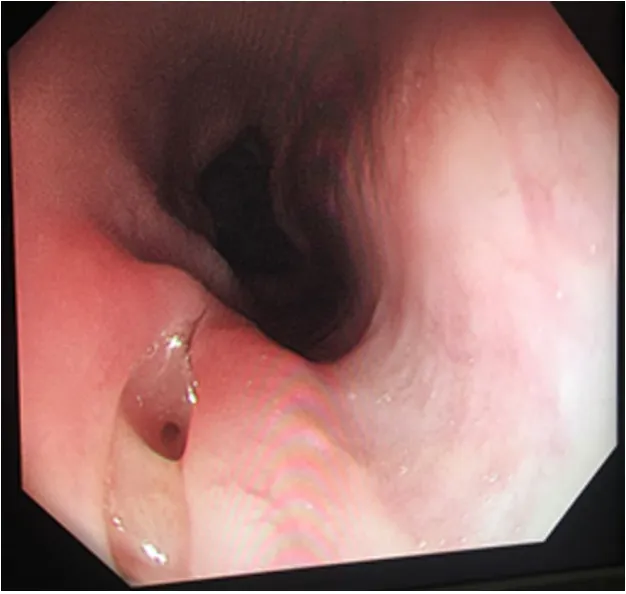
Figure 1 Endoscopy image: An opening is seen in the mid-esophagus without active bleeding or clots.
FINAL DIAGNOSIS
Tubercu lous esophagom ed iastinal fistu la w ith m ed iastinal b ronch ial artery aneu rysm.
TREATMENT
Patien t was treated by m ed iastinal bronchial artery aneu rysm trans catheter coil em bolization and antitubercu lar m ed ications.
OUTCOME AND FOLLOW-UP
A fter 3 m o of m ed iastinal bronchial artery aneu rysm em bolization and initiation of antitubercu lar m ed ication, patient becom e asym p tom atic and no fu rther ep isode of GI bleed ing was encountered. Follow-up chest X-ray show s in terval resolu tion of lung cavity.
DISCUSSION
Esophageal involvem ent in TB is extrem ely rare in otherw ise healthy ind ividuals. It m ostly affects the m id-esophagus and is secondary to d irect extension from the su rround ing structu res such as m ed iastinal lym ph nodes, lungs, and vertebrae. The usual p resen ting sym p tom s are d ysphagia or odynophagia[2]. There are several reports on esophageal TB that appeared as subm ucosal lesions m im icking a m ass,u lcer, d iverticu lum, or on ly sinus opening[1].
Bronchial artery aneu rysm is a rare cond ition w ith reported rate of < 1% in selective bronchial arteriogram[6]. It is can be classified accord ing to location as m ed iastinal or intrapu lm onary. Clinical p resen tation is variab le depend ing on the size, location,concom itan t d isease and if it is rup tu red or not. A lthough it usually detected incidentally on chest CT, the m ost frequent sym p tom s are hem op tysis, chest pain, and hem om ed iastinum[7]. Chest CT is greatly help fu l in detecting TB m anifestation in the chest and m ed iastinal lym ph nodes as w ell as associated fistu la form ation[8]. CT angiography and conven tional angiography are comm on ly used tools to d iagnose m ed iastinal bronchial aneu rysm[3].
M ed iastinal bronchial artery aneu rysm s are fatal and even asym p tom atic, requiring treatm en t regard less of the d iam eter. Endovascu lar em bolization is the first line o f treatm en t, and su rgery is reserved as the last op tion for som e patien ts w ith con traind ication to endovascu lar therapy[3,5,7]. An ti-TB m ed ication is the m ainstay treatm ent of m ed iastinal TB. A large esophageal fistu la secondary to TB cou ld be treated by surgery or endoscopic clipp ing[2,8].
In this case report, although TB was suspected from the beginning, the p resence of acu te upper GI b leed ing m ade it challenging to determ ine its sou rce and treat it.Endoscopy and bronchoscopy - the exam inations of choice for upper GI bleed ing and suspected tracheoesophageal fistu la - failed to identify the sou rce. Chest CT w ith IV contrast and conventional angiography follow ed by coil em bolization w ere of great value for d iagnosis and treatm ent o f such a rare cond ition. W e believe that TB is ap rim ary d isease that involves the lung and then extends to the m ed iastinum and leads to esophageal fistu la and m ed iastinal bronchial artery aneu rysm form ation. This rare p resen tation of acu te upper GI bleed ing is m ost likely due to m ed iastinal bronchial artery aneu rysm that cau sed b leed ing and d rained in to the esop hagus by the esophagom ed iastinal fistu la.
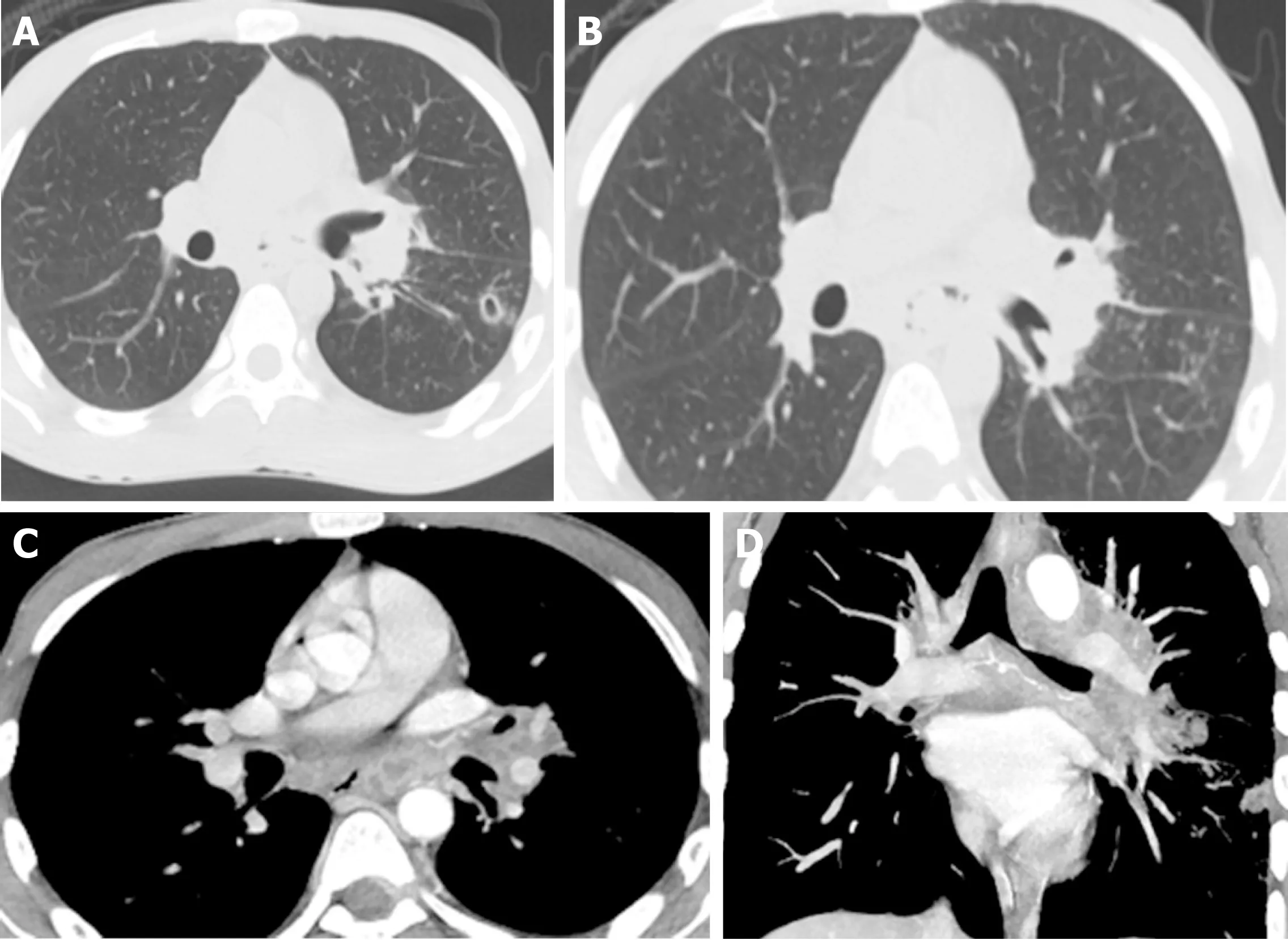
Figure 2 Computed tomography chest. A: Computed tomography lung window axial image shows left lower lobe lung cavitary lesion with multiple nodules in tree-in-bud configuration, a classical sign of lung tuberculosis; B: Chest computed tomography lung window axial image shows multiple mediastinal air pockets anterior to the esophagus,indicating an esophageal fistula; C: Computed tomography chest with IV contrast mediastinal window axial image shows multiple mediastinal necrotic lymph nodes and mediastinal air pocket anterior to esophagus indicating mediastinal tuberculosis and esophageal fistula; D: Computed tomography chest with IV contrast maximum intensity projection coronal reformatted image shows mediastinal bronchial artery aneurysm.
CONCLUSION
We successfu lly treated a patient w ho p resented w ith acu te upper GI bleed ing due to tubercu lous esophagom ed iastinal fistu la and m ed iastinal bronchial artery aneu rysm using transcatheter coil em bolization.

Figure 3 Conventional angiography. A: Selective angiogram of the bronchial artery showing 2 small mediastinal aneurysms; B: Post-coil-embolization angiogram shows complete occlusion of the artery and aneurysms.

Figure 4 Follow-up chest X-ray shows resolution of cavitary lesion and no consolidation. Coils are seen in the mediastinum.
Figure 4
杂志排行
World Journal of Gastroenterology的其它文章
- Microbial metabolites in non-alcoholic fatty liver disease
- Recent advances in gastric cancer early diagnosis
- Evolving screening and surveillance techniques for Barrett's esophagus
- Proton pump inhibitor: The dual role in gastric cancer
- Herbs-partitioned moxibustion alleviates aberrant intestinal epithelial cell apoptosis by upregulating A20 expression in a mouse model of Crohn’s disease
- Analysis of the autophagy gene expression profile of pancreatic cancer based on autophagy-related protein microtubule-associated protein 1A/1B-light chain 3
