Chronic functional constipation is strongly linked to vitamin D deficiency
2019-05-08AlbaPanareseFrancescoPescePieroPorcelliGiuseppeRiezzoPalmaAureliaIacovazziCarlaMariaLeoneMassimoDeCarneCaterinaMammoneRinaldiEndritShahini
Alba Panarese, Francesco Pesce, Piero Porcelli, Giuseppe Riezzo, Palma Aurelia Iacovazzi, Carla Maria Leone,Massimo De Carne, Caterina Mammone Rinaldi, Endrit Shahini
Abstrac t BACKGROUND Few studies have examined intestinal motility disorders, which are disabling conditions associated with chronic functional constipation, whose pathogenesis is actually not well-defined.AIM To investigate the relationship between serum 25-hydroxyvitamin D levels and functional chronic constipation associated to intestinal motility disorders.METHODS We performed a prospective case-control study, from May-June to November 2017. Glucose/lactulose breath tests, radiopaque markers (multiple capsule techniques) and wireless motility capsule analysis were used to assess colonic and oro-cecal transit time, after excluding small-intestinal bacterial overgrowth condition. Then, we measured 25-hydroxyvitamin D levels in patients with intestinal motility disorders and we further evaluated the influence of intestinal motility disorders on psychological symptoms/quality of life using validated questionnaires, the Irritable Bowel Syndrome Quality of life (IBS-QOL), the Short Form Health Survey 12, and the Hospital Anxiety and Depression Scale 14(HADS-14 A and HADS-14 D).RESULTS We enrolled 86 patients with chronic functional constipation associated to intestinal motility disorders and 86 matched healthy subjects. Patients with intestinal motility disorders had lower 25-hydroxyvitamin D levels (P < 0.001), and they showed a significant impairment of all health-related quality of life and psychological tests (IBS-QOL, Short Form Health Survey 12-Physical Component Summary, Short Form Health Survey 12-Mental Component Summary, HADS-14 A and HADS-14 D), as compared to the control group (P < 0.001), which significantly correlated with low vitamin D levels (r = - 0.57, P < 0.001; r = 0.21, P = 0.01; r = - 0.48, P < 0.001; r = - 0.57, P < 0.001; r = - 0.29, P < 0.001, respectively). At multivariate analysis vitamin D low levels remained a significant independent risk factor for the occurrence of intestinal motility disorder (odds ratio = 1.19; 95% confidence interval: 1.14-1.26, P < 0.001).CONCLUSION Vitamin D deficiency, anxiety and depression symptoms are commonly associated with chronic functional constipation induced by intestinal motility disorders. Vitamin D serum levels should be routinely measured in these patients.
Key words: Chronic constipation; Intestinal motility; Vitamin D; Quality of life; Anxiety; Depression
INTRODUCTION
The term “Constipation” has a broad definition both for physicians and patients[1].The most common form is functional chronic constipation, which is a gastrointestinal disorder defined by symptom criteria, after the exclusion of secondary causes[2-4]. This clinical condition usually affects women, older subjects, particularly those of lower socioeconomic status[5], and has a prevalence ranging between 2% and 27% in western countries with a high burden on global health-care system[2,6,7]. The main symptoms of functional chronic constipation are difficulty with evacuation, bloating, abdominal pain, discomfort or hard stools that significantly impair health-related quality of life[2,8]. Since d ep ression has been commonly observed in p atients w ith the constipation variant of irritable bowel syndrome (IBS), specific questionnaires have been end orsed to evaluate some aspects of the quality of life of these patients,especially the IBS Quality of life (IBS-QOL), the Short Form Health Survey 12 (SF-12),and the Hospital Anxiety and Depression Scale 14 (HADS-14-A/D)[9-12]. Moreover,previous stud ies show ed a possible role of vitamin D d eficiency in the pathophysiology of IBS and depression, and also beneficial effects of vitamin D supplementation in alleviating d epression and certain gastrointestinal symptoms in a p opulation of study prevalently affected by diarrhea or by alternating subtype, and the minority by constipation symptoms[13-20]. Normal transit constipation is probably the most common form, and it frequently overlaps w ith the constipation variant of IBS[9].
Among patients w ith functional chronic constipation, intestinal motility disord ers have been reported. Although the overall prevalence of intestinal motility disorders is not currently w ell-d efined[2], it involves more commonly patients affected by slow transit constipation (STC)[2], and rarely subjects w ith d elayed oro-cecal transit time[21],In addition, defecation disorders significantly overlap with normal and STC[9,22]. While STC is characterized by an altered colonic motor activity, and reduced reaction after a meal and w hen w aking up, decreased “high amplitud e prop agated contractions”,which have been associated to altered regulation of enteric nervous system, reduction of neurons and axons in the myenteric p lexus[2,22-24], d elayed oro-cecal transit time could be partially associated with an underlying small-intestinal bacterial overgrow th(SIBO)[25].
Moreover, the most severe form of intestinal motility disorder may be considered chronic intestinal pseudo-obstruction, w hich is a symptomatic and disabling disease,related to a visceral myopathy or/and neuropathy[26]. Hence, colonic transit time could be objectively measured by rad iopaque markers (single or multiple capsule techniques), and this d iagnostic tool is also used to rule out d yssynergia d efecation[2,23]. Radiopaque markers studies are useful, inexpensive and w idely available[2,23].In addition, even if not definitively recommended by guidelines, lactulose breath test(LBT) and glucose breath test (GBT), are commonly used in clinical p ractice to evaluate the presence of SIBO as well as small-bowel motility by estimating oral-cecal transit time[25,27]. Other exp ensive tests such as colonic scintigrap hy and w ireless ingestible motility capsule, measure more accurately overall transit time[23,27], w hereas advanced physiologic tests identify anorectal dysfunctions in patients not responding to initial therapy[2,27]. In this paper w e hypothesized that serum vitamin D deficiency could be associated w ith chronic functional constip ation second ary to d elayed intestinal transit time and consequently w e investigated this relationship and the related psychological aspects.
MATERIALS AND METHODS
Study design
This case-control study w as p erformed from May-June to November 2017, in the Outpatients Clinic of our Institution, in Apulia, a Med iterranean region located in southeast of Italy. As shown in Figure 1, w e enrolled 86 subjects from a population of 152 consecutive constipated patients affected by intestinal motility disorders.
Inclusion criteria were the following: Caucasian subjects ≥ 18 years old, body mass index (BMI) ≥ 18.5 kg/m2, affected by functional chronic constipation associated to delayed intestinal transit time, supported by Roma IV criteria[8,26,28]. Exclusion criteria were the follow ing: Subjects > 75 years old, IBS, pregnancy, significant comorbidities such as card iac, respiratory, chronic renal insufficiency, anorectal and p elvic floor d ysfunctions, metabolic/end ocrine (d iabetes mellitus, hypothyroid ism, hyp ercalcaemia, p anhypopituitarism), med ications (op iates, antihypertensive agents, iron p rep arations, anti-ep ilep tic d rugs, tryciclic antid epressants, anticholinergics or dopaminergics), organic (extra-intestinal mass, colorectal cancer, ischaemic or surgical stenosis, anal fissure, anal strictures, inflammatory bow el d isease, intestinal malabsorption and diverticular diseases), neurological (Parkinson disease, multiple sclerosis, parap legia, autonomic neuropathy, chronic intestinal pseud o-obstruction,gastrop aresis, Hirschsp rung d isease and stroke), p ast p sychiatric d isease, and myogenic (scleroderma, amyloid osis and myotonic d ystrophy d ermatomyositis)[2,21,26].In addition, we also assessed a control group of 86 healthy subjects (sex, age and BMI matched), recruited from a pop ulation-based cohort study of 150 healthy subjects,which underw ent routine clinical exams in our Institute to check their healthy status,after excluding the presence of a functional chronic constip ation during the clinical interview.
Our research w as carried out in compliance w ith the Helsinki Declaration and proced ures received ap p roval by the Institutional review board of the National Institute of Gastroenterology “S. De Bellis” Research Hospital (0807/16) and by the Research Ethics Committee of the National Oncological Institute of Bari(CAAE:147/16) (Trial registration number: NCT03096704). Informed consent w as obtained from all participants of the study. The statistical review of the study w as performed by a biomedical statistician.
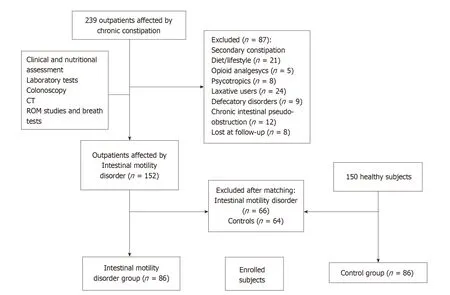
Figure 1 Flow diagram describing the process of patients' selection. CT: Computerized tomography; ROM: Radiopaque markers.
Definition of functional chronic constipation
All selected patients were inquired, before, for any possible secondary causes of functional chronic constipation, including alarm features, lifestyle factors and medical treatments and we also identified the response (or lack of) to previous treatment about constipation symptoms, by interviewing patients. Then, they were considered affected by functional chronic constipation only when they showed a frequency of evacuation less than tw ice a week with increased stool consistency[8,26,28]. All the selected patients underwent blood tests, colonoscopy, nutritional assessment (with daily food frequency questionnaires), stool frequency diary, LBT, GBT, wireless motility testing, radiopaque markers studies, and when required, tests for pelvic floor dysfunction, and psychological tests exploring patient's quality of life.
Accordingly, when not eligible, patients were excluded (Figure 1): 152 consecutive subjects affected by functional chronic constipation with intestinal motility disorders met the eligibility criteria, along with 150 healthy subjects. Patients and controls in each group were first randomly sampled from the pool of available individuals (152 with intestinal motility disorders and 150 controls) and, then matched for age, sex and BMI, using MatchIt[29]. This analysis resulted in 86 patients and 86 matched controls that were enrolled for the study. Our patients did not receive any pharmacological treatment before all evaluations.
Colonic transit time, breath tests and wireless motility analysis
The colon transit time was measured with radiopaque markers, using multiple capsule techniques (P and A Mauch CH-4142 Munchenstein). The patient ingested 1 capsule a day (at 9.00 am, during breakfast) for 3 consecutive days and each capsule with 24 different shaped radio-opaque polyurethane markers, and then performed abdominal x-rays (100KV) on day 7, at 9.00 am, to reconstruct the colon activity during the last week[30,31]. Normal transit time was considered about 30-40 h, whereas the upper limit, above 70 h. Markers scattered about the colon was due most likely to STC, w hereas markers gathered in the recto-sigmoid tract w as considered a defecatory disorder[5,27](Supplementary material).
Moreover, LBT and GBT were used for measuring oro-cecal transit time. A rise in hydrogen of ≥ 20 ppm by 90 min was considered the cut-off value used to exclude SIBO for both tests[25]. Time to the second peak and rise of 5-10 ppm of hydrogen, or a level of positivity for methane ≥ 10 ppm on a breath test, were considered useful in estimating oro-cecal transit time[25,27,32](Supplementary material). Wireless motility analysis w as also used to quantify oro-cecal transit time (Smartpill, Med tronic,Sunnyvale, California, United States), in ord er to d efine the presence of a d elayed small intestinal transit time. Normal small-bowel transit should be 6 hours or less[25](Supp lementary material). Finally, STC and/or d elayed oro-cecal transit time w ere definitively endorsed w hen radiopaque markers and/or breath tests w ith w ireless motility analysis identified a specific intestinal motility disorder[27].
Questionnaires for the evaluation of quality of life in patients with intestinal motility disorders
The IBS-QOL questionnaire is a 34-item tool validated to quantify quality of life in non-subtyped IBS patients, but also used to assess the severity of IBS-like symptoms,and psychological factors[10]. The SF-12 includes a subset of 12 items, used to assess the physical and mental health domain in many diseases. All these scores are converted into a standardized 0-100 score. Higher scores indicate a better self-reported health status[11]. Furthermore, the HADS-14 represents a global measure of psychological distress and includes 14 items, 7 of them evaluate anxiety symptoms, and 7 depressive ones. Each item is coded from 0 to 3. The total scores for anxiety and depression can range between 0-21, based on symptoms characteristics[12].
Vitamin D and parathyroid hormone levels measurement
Serum 25-hydroxyvitamin D [25-(OH)-D] (Supplementary material) and parathyroid hormone (PTH) levels w ere measured in patients and healthy controls within 1 hour from blood draw. Overall subjects were enrolled in the interval time of the year w ith major sunlight exposition, w hen 25-(OH)-D values are usually higher[13]. The 25-(OH)-D levels status was categorized as usually proposed by experts in literature: using a stand ard ized cut-off (d eficiency less than 20 ng/m L, insufficiency from 20 to 29 ng/mL and sufficient when equal or higher than 30 ng/mL)[13].
Statistical analysis
Screened patients and controls in each group w ere matched for age, sex and BMI using the nearest neighbor matching algorithm implemented in MatchIt[29]. Normal distribution of continuous variables was assessed with the Shapiro-Wilk test and data were expressed as mean and standard deviation and compared using Student's t-test.Categorical variables w ere rep orted as p ercentages and comp ared using the Chisquared test or Fisher's exact test, w hen needed.
Sp earman's test w as performed to evaluate p ossible correlations of vitamin D values w ith quality of life scores and psychological functions (IBS-QOL, SF12-PCS,SF12-MCS, HADS-14 A and HADS-14 D). The imp act of the vitamin D levels on patient's risk to have intestinal motility disorders w as analysed using univariate and multivariate logistic regression analyses. The association betw een each explanatory variable and the outcome (intestinal motility d isorders occurrence) was tested using the likelihood ratio test. We includ ed in the multivariate mod el all exp lanatory variables showing a P < 0.05 at univariate analysis. For each variable includ ed in the multivariate mod el, w e calculated both unad justed and ad justed od ds ratios (OR),w ith their 95% confid ence intervals (CI), and the level of significance (using the likelihood ratio test). Statistical significance was set at P < 0.05. All statistical analyses w ere performed using SPSS 23.0 software (SPSS, Chicago, IL, United States) and R version 3.4.3 (http://www.R-project.org/).
RESULTS
Characteristics of patients with intestinal motility disorders
As show n in Figure 1, 86 patients along w ith 86 healthy matched subjects, were finally enrolled. The characteristics of patients are show n in Table 1. About 85% of patients suffering from intestinal motility disorders were female, and mean age was 49.9 ± 17.4 years. Patients w ith intestinal motility disorders had significantly low er intermed iate and bachelor schooling d egree, as compared to the control group (P = 0.001 and P <0.001, respectively).
The proportion of patients with intestinal motility d isorders w as more affected by constipation, abdominal pain, swelling, anxiety and depression symptoms as well as by quality of life alterations, as compared to healthy subjects (P < 0.001). The results of the various questionnaires compiled by patients (IBS-QOL, HADS-14 A, HADS-14 D,SF12-PCS and SF12-MCS) show ed a significant imp airment in all health-related domains (P < 0.001) (Table 1). Patients w ith intestinal motility d isord ers had lower vitamin D serum levels, as compared to the control group (P < 0.001). Moreover, the poor results of psychological tests (IBS-QOL, SF12-PCS, SF12-MCS, HADS-14 A andHADS-14 D) significantly correlated with low vitamin D levels (r = - 0.57, P < 0.001; r= 0.21, P = 0.01; r = - 0.48, P < 0.001; r = - 0.57, P < 0.001; r = - 0.29, P < 0.001,respectively). Other parameters, such as the age, sex and marital status did not differ between the two groups (Table 1).
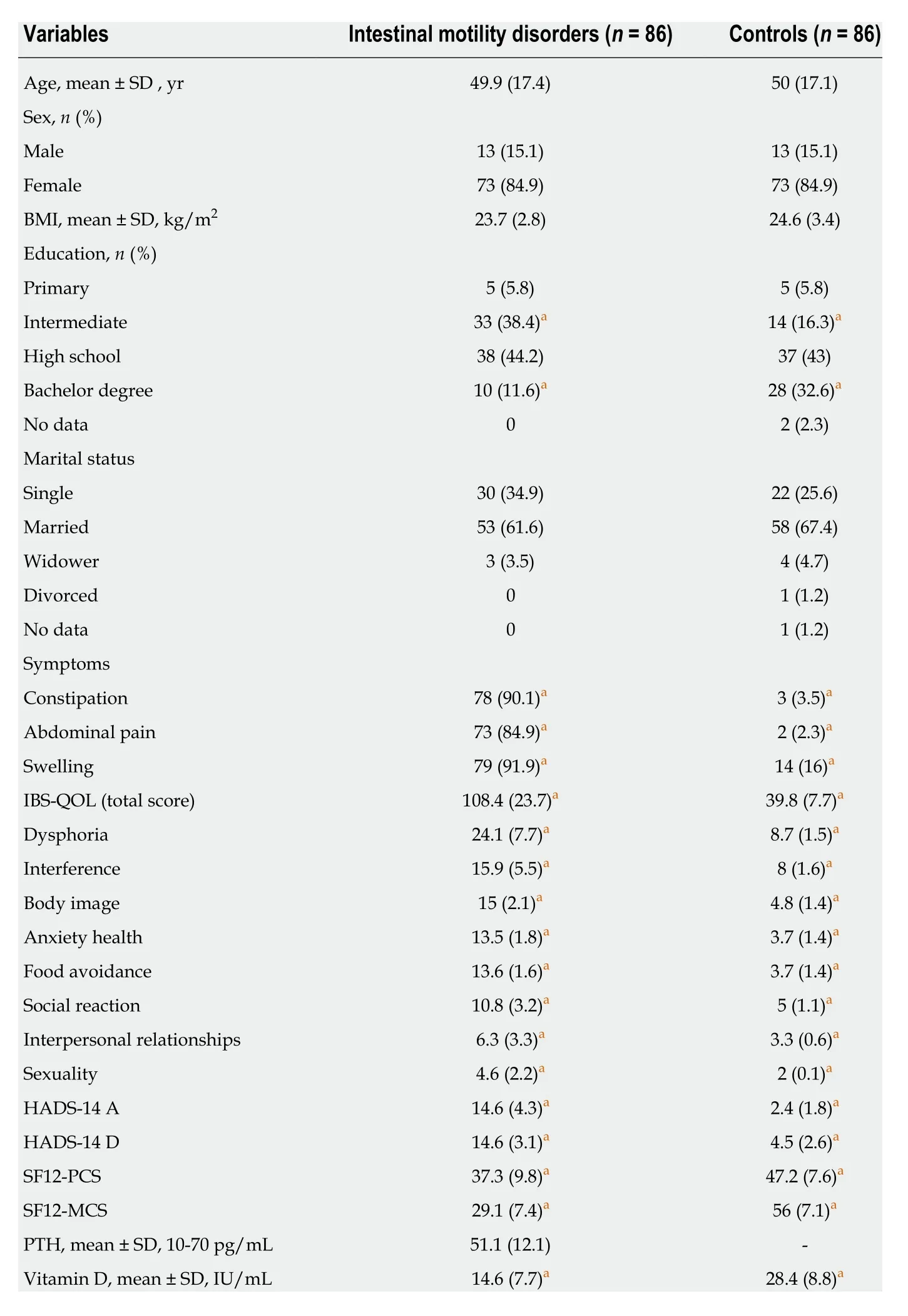
Table 1 Characteristics of patients with functional chronic constipation with intestinal motility disorders and of controls
In the groups with intestinal motility disord ers, 32, 28 and 26 patients, after completing all diagnostic tests, received a diagnosis of delayed oro-cecal transit time(37.2%), STC (32.6%) or delayed oro-cecal transit time with STC (30.2%), respectively.In the group with delayed oro-cecal transit time and with STC, the proportion of patients w ho suffered constipation, sw elling, abd ominal pain and vitamin D deficiency (< 20 ng/mL) was higher than groups with delayed oro-cecal transit time or with STC (P = 0.03, P = 0.02, P = 0.03 and P = 0.04 respectively) (Figure 2). When we considered the three groups: subjects w ith delayed transit time in both intestinal tracts(26), to patients with delayed transit time in only one tract (60) and to controls (86),the quality of life show ed worsening functions. Moreover, vitamin D and BMI were significantly red uced w ith d ecreasing values as follow ing for the variables: delayed oro-cecal transit time with STC group less than delayed oro-cecal transit time or STC group, less than controls (P < 0.001, respectively) (Supplementary material).
Patients with delayed transit time of both intestinal tracts, as compared to patients w ith d elayed transit time involving only one tract, show ed significantly red uced levels of vitamin D and higher PTH levels (for both P < 0.001), and showed worsening quality of life (P < 0.001) (Supplementary material). Patients w ith delayed transit time in both intestinal tracts show ed significantly reduced serum levels of vitamin D and higher PTH serum levels (for both P < 0.001), and show ed w orsening quality of life (P< 0.001) than p atients w ith delayed transit time in only one tract (Sup plementary material).
Risk factors associated to intestinal motility disorders
Results from linear regression analysis are show n in Table 2. At univariate and multivariate analysis ad justed for BMI, vitamin D levels remained a significant independent risk factor for intestinal motility disorders occurrence (OR = 1.19; 95%CI:1.14-1.26, P < 0.001).
DISCUSSION
In this stud y, w e d emonstrated for the first time that serum vitamin D deficiency could be associated to functional chronic constipation ind uced by intestinal motility disorders. Furthermore, patients show ing the latter clinical condition are frequently affected by anxiety and depression symptoms which severely impair their quality of life.
About 1 billion people have vitamin D insufficiency or d eficiency[13]. Now ad ays,this phenomenon is associated w ith significant d isability and healthcare costs[14,15].Several studies show ed that hypovitaminosis D may be a risk factor for many chronic diseases and for mortality[16,33-36]. Notably, vitamin D deficiency has been involved in the pathophysiology of inflammatory bowel disease, IBS and also depression[13-17,19]
Some multicentric studies, reported a higher prevalence of hypovitaminosis D in the southern Europe[37,38]. Interestingly, Italian eld erly subjects show ed the low est levels of vitamin D in Europe in the w inter season[37,38]. In our stud y, w e found low serum levels of vitamin D, mainly checked d uring the summer season, among patients affected by intestinal motility disorders during an interval time when vitamin D values are usually high, due to beta-ultraviolet rays exposition[13,36]. Moreover, our patients were prevalently female (84.9%) and relatively younger, although, vitamin D deficiency has not been limited to the elderly age[35-38]. While low levels of vitamin D have been also observed in w inter in 33% of pre-menopausal w omen, especially if obese[39], in our study the majority of patients w ith intestinal motility disorders had normal BMI.
How vitamin D deficiency and intestinal motility disorders are linked remains an open question. One intriguing hyp othesis may be that STC and/or delayed small intestinal transit time could negatively modify the gut microbiota[36], or conversely altered microbiome could primarily affect mucosal barrier and gut motility d ue to microbial-derived metabolites[40]. In addition, some studies suggested that vitamin D d eficiency could p red isp ose to gastrointestinal infections[16], w hich could be resp onsible of the “leaky gut” alteration and of loss of immune homeostasis[40,41].How ever, in our patients w e also performed LBT and GBT, to exclude SIBO. When the clinical susp icion of the latter cond ition remained, w e treated them “ex juvantibus”, and w e further exclud ed SIBO as the main cause of bow el symptoms,esp ecially w hen they d id not d isappear after a gut-targeted antibiotic therapeutic cycle.
Anyway, the presence of vitamin D receptor on gut epithelial cells, macrophages and lymphocytes surface, has suggested a possible link between vitamin D deficiency,the dysfunction of its receptor and gut microbiota composition, leading to the onset of autoimmune diseases[40,42,43]. Finally, the influence of vitamin D deficiency on human immune system is also supported by its involvement in the development of multiple sclerosis[44]. As concerning this asp ect, an interesting stud y sup p orted a role of autoantibodies against enteric nervous system targets in B cell-d eficient mice w ith exp erimental autoimmune encephalomyelitis mod el of multip le sclerosis, show ing that serum immunoreactivity (id iop athically or second ary to another autoimmune d isease), could be imp licated in the ind uction of autoimmune gastrointestinal dysmotility[45]. In fact, in humans w ith multip le sclerosis, w hose p athogenesis has been linked to vitamin D deficiency, a slow colonic motility in the proximal tract as well as autonomic rectal dysfunction has been observed[44-48].
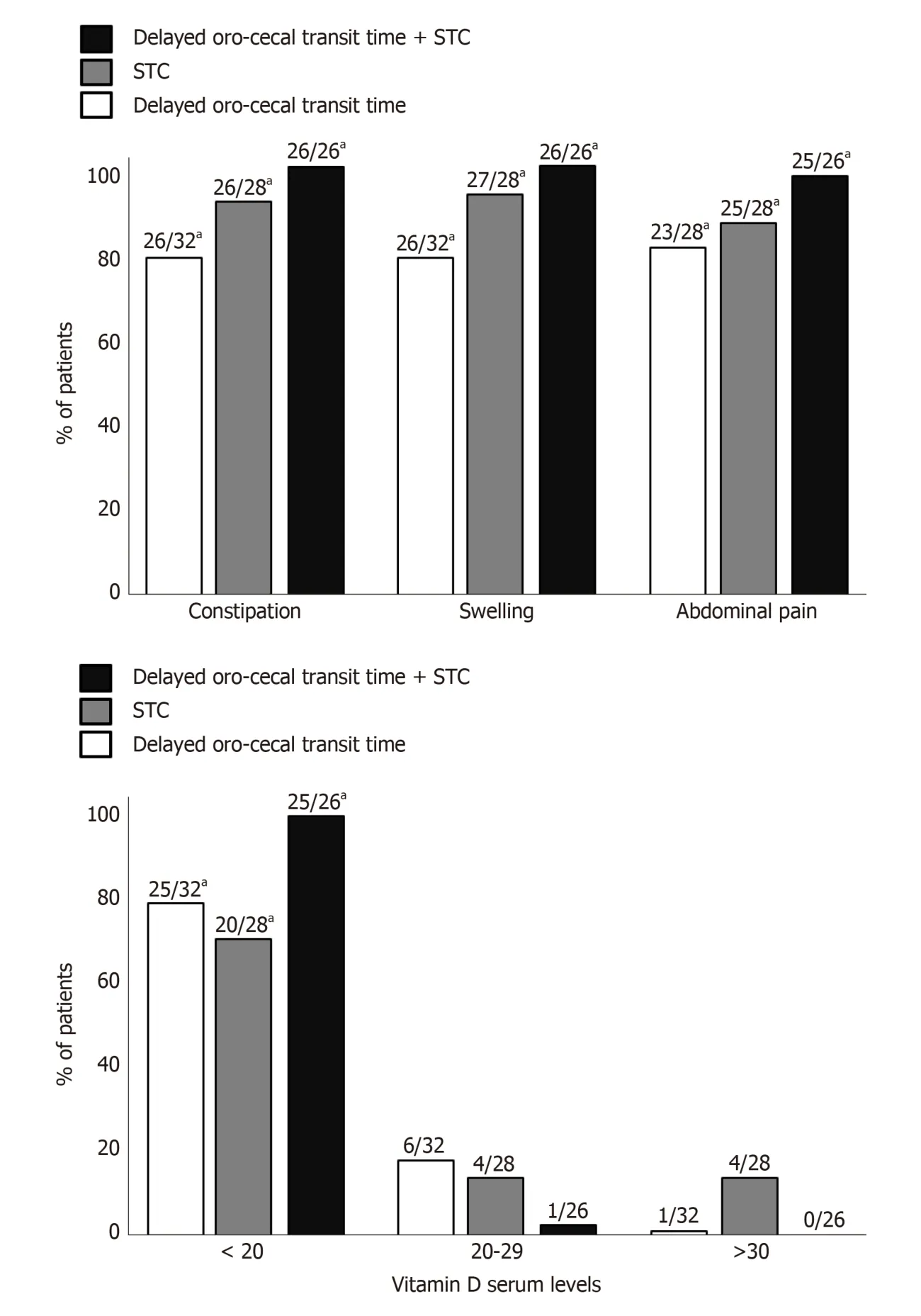
Figure 2 Proportion of patients who suffered constipation, swelling, abdominal pain and vitamin D serum levels, in delayed small intestinal transit time, slow transit constipation, and delayed small intestinal transit time (with) slow transit constipation groups. STC: Slow transit constipation. Significantly different by a P < 0.05.
We may sup p ose that the intestinal motility d isord er could be the “p rimum movens” of an und erlying autoimmune process in a specific genetic background and unmasked by chronic vitamin D d eficiency, w hich could exert metabolic/immunologic damage on ep ithelial and neuromuscular structures of the gut. The latter alterations could include gut hyper-permeability and bacterial translocation, whose d egree of injury and extension could be influenced by the severity of vitamin D deficiency[22,45]. This hypothesis may be supported by our results, which show ed that levels of vitamin D were ind epend ently associated w ith intestinal motility d isorders and by the fact that the prevalence of symptoms associated to functional chronic constip ation grew up in concord ance w ith the w orsening of vitamin D levels,esp ecially in p atients involving more extensively the bow el tract. Furthermore,patients with intestinal motility disorders had high levels of psychological d istress with impaired quality of life, and hypovitaminosis D significantly correlated with the worsening of the psychological functions. In our study, a potential bias could d erive from d isease misclassification, w hich could be a negligible factor since intestinal motility disorder w as diagnosed following standardized criteria, and from the small samp le size of our p op ulation. Moreover, w e d id not check fecal microbiota composition.
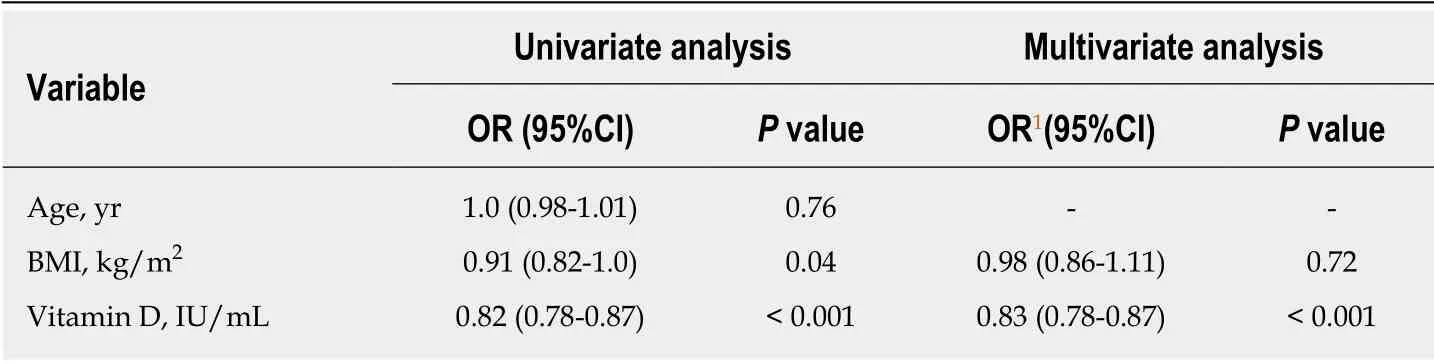
Table 2 Probability of intestinal motility disorder occurrence at the univariate and multivariate analysis
In conclusion, we demonstrated that vitamin D deficiency could be strongly related to intestinal motility disorders. Moreover, patients with intestinal motility disorders are very commonly affected by anxiety and depression symptoms which severely influence their quality of life. If the latter two psychiatric symptoms are caused by intestinal factors, it will be confirmed only through a cross-sectional study. Therefore,we suggest that vitamin D serum levels should be routinely measured and vitamin D supplementation should be considered, to better evaluate its effects on intestinal motility and quality of life of patients with intestinal motility disorders.
ARTICLE HIGHLIGHTS
Research background
Functional chronic constipation is a gastrointestinal disorder that affects more commonly women and older subjects, with a deep impact on global health-care system. Nowadays, only few studies have examined intestinal motility disorders, which are severe clinical conditions associated with chronic functional constipation, whose pathogenesis and prevalence are actually partially known. In this subgroup are inclued patients with slow transit constipation, as well as with slow oro-cecal transit time, whereas their extreme clinical form, could be considered chronic intestinal pseudo-obstruction, which has been related to the structural damage of neural and smooth muscle cells of gut.Research motivation
Research motivation
Although some studies have shown a possible link between vitamin D deficiency and irritable bowel syndrome (IBS), as well as with depression (and with several other diseases), the same link has never been detected before in patients affected by intestinal motility disorders, and the indications to look for vitamin D in these patients relied only of opinions of experts in the field.Therefore we investigated this relationship and the psychological aspects in this subgroup of patients.
Research objectives
To investigate the relationship between serum 25-hydroxyvitamin D levels and functional chronic constipation linked to intestinal motility disorders.
Research methods
Herein, we applied rigorous statistical methods to elucidate this relationship. We performed a prospective case-control study, from May-June to November 2017. We used Glucose/lactulose breath tests, radiopaque markers (multiple capsule techniques) and wireless motility capsule analysis to estimate both oro-cecal and colonic transit time. After receiving a diagnosis of intestinal motility disorders, patients underwent to blood sampling, for checking 25-hydroxyvitamin D levels. Furthermore, we evaluated for these patients the influence on psychological features and on their quality of life, which were estimated by using validated questionnaires, the IBS Quality of life (IBS-QOL), the Short Form Health Survey 12 (SF-12), and the Hospital Anxiety and Depression Scale 14 (HADS-14 A and HADS-14 D).
Research results
Our cohort included 86 patients with chronic functional constipation associated to intestinal motility disorders and 86 age, sex, body mass index (BMI)-matched healthy subjects. Patients with intestinal motility disorders had lower 25-hydroxyvitamin D levels (P < 0.001), and they showed a significant impairment of all health-related quality of life domains and psychological tests (IBS-QOL, SF12-PCS, SF12-MCS, HADS-14 A and HADS-14 D), as compared to the control group (P < 0.001). Moreover, the latter tests significantly correlated with reduced vitamin D
levels (r = - 0.57, P < 0.001; r = 0.21, P = 0.01; r = - 0.48, P < 0.001; r = - 0.57, P < 0.001; r = - 0.29, P< 0.001, respectively). In multivariate analysis, vitamin D low levels remained significantly associated with the occurrence of intestinal motility disorder, after adjusting for BMI (odds ratio= 1.19; 95% confidence interval: 1.14-1.26, P < 0.001).
Research conclusions
We d emonstrated for the first time a strong association betw een vitamin D deficiency and intestinal motility disorders. Moreover, these patients are very commonly affected by anxiety and depression symptoms which deeply impact on their quality of life. These findings suggest that vitamin D serum levels should be routinely measured in this category of patients and consequently vitamin D supplementation could represent a further therapeutic aid for this clinical condition.
Research perspectives
Our findings may confirm how vitamin D deficiency could exert a w ide spectrum of action in many gastrointestinal (or not) diseases, being highly associated with intestinal motility disorders and w ith certain neuropsychiatric symptoms, but remains unclear if it could have a causative role in this process, and for this reason, future cross-sectional stud ies are need ed, also to investigate if anxiety and depression symptoms are caused by intestinal factors.
ACKNOWLEDGEMENTS
We thank to Vanessa Terenzio and Domenico Flavio Terenzio, native English speakers, for the language revision of this manuscript.
杂志排行
World Journal of Gastroenterology的其它文章
- Precision surgical approach with lymph-node dissection in early gastric cancer
- Update on hepatocellular carcinoma: Pathologists' review
- Application of artificial intelligence in gastroenterology
- Clinical significance of programmed death 1/programmed death ligand 1 pathway in gastric neuroendocrine carcinomas
- Functional role of long non-coding RNA CASC19/miR-140-5p/CEMIP axis in colorectal cancer progression in vitro
- Seven-senescence-associated gene signature predicts overall survival for Asian patients with hepatocellular carcinoma
