Triggers of histologically suspected drug-induced colitis
2019-03-09ThorstenBrechmannKatharinantherMatthiasNeidWolffSchmiegelAndreaTannapfel
Thorsten Brechmann, Katharina Günther, Matthias Neid, Wolff Schmiegel, Andrea Tannapfel
Abstract BACKGROUND Drug toxicity is a common and even serious problem in the gastrointestinal tract that is thought to be caused by a broad spectrum of agents. Although withdrawal of the causative agent would cure the disease knowledge is scarce and mostly derives from case reports and series.AIM To investigate potential triggers of drug-induced colitis (DiC).METHODS We conducted a retrospective, observational case control study. Patients were assigned to DiC or one of two age- and gender-matched control groups (noninflammatory controls and inflammatory colitis of another cause) based on histopathological findings. Histopathology was reassessed in a subset of patients(28 DiC with atherosclerosis, DiC without atherosclerosis and ischaemic colitis each) for validation purposes. Medical history was collected from the electronic database and patient records. Statistical analysis included chi-squared test, t-test,logistic and multivariate regression models.RESULTS Drug-induced colitis was detected in 211 endoscopically sampled biopsy specimens of the colon mucosa (7% of all screened colonoscopic biopsy samples);a total of 633 patients were included equally matched throughout the three groups (291 males, mean age: 62.1 ± 16.1 years). In the univariate analysis, DiC was associated with diuretics, dihydropyridines, glycosides, ASS, platelet aggregation inhibitors, nonsteroidal anti-inflammatory drugs (NSAIDs), statins and fibrates, and with atherosclerosis, particularly coronary heart disease, and hyperlipoproteinaemia. Echocardiographic parameters did not show substantial differences. In the multivariate analysis only fibrates [odds ratio (OR) = 9.1],NSAIDs (OR = 6.7) and atherosclerosis (OR = 2.1) proved to be associated with DiC. Both DiC reassessment groups presented milder inflammation than ischaemic colitis. The DiC patients with atherosclerosis exhibited histological features from both DiC without atherosclerosis and ischaemic colitis.CONCLUSION Several drugs indicated for the treatment of cardiovascular and related diseases are associated with DiC. Atherosclerosis and microcirculatory disturbances seem to play an important pathogenetic role.
Key words: Drug toxicity; Drug-induced colitis; Ischaemic colitis; Drug-associated gastrointestinal disease; Atherosclerosis; Colonic ischaemia; Nonsteroidal antiinflammatory drugs; Fibrates
INTRODUCTION
Drug toxicity is a common and even serious problem in the gastrointestinal tract that is thought to be caused by a broad spectrum of drugs. Related symptoms are unspecific and assumed to cover the whole set of complaints known for colitis of any other cause, i.e., bloating, abdominal pain, cramping, diarrhoea, weight loss, mucosal bleeding or anaemia[1,2]. Furthermore, the continued intake of harmful medications can lead to structural bowel damage, i.e., development of strictures[3], perforation[4]or severe colitis with the need for emergency colectomy[5]. Although withdrawal of the respective trigger should cure the disease, data about drug-induced colitis (DiC) are scarce. Deeper insights into the phenotype of DiC, the underlying pathomechanisms and the identification of possible triggers are mandatory particularly since intake of multiple drugs hampers the determination of a single drug as the causative agent.
Various patterns of drug-induced damage at the colonic site have been described.These include nonsteroidal anti-inflammatory drug (NSAID) colonopathy,antraquinone-induced laxative-associated damage (melanosis coli), corticosteroidassociated damage (malakoplakia), gold compound-associated damage and other drug-induced conditions, such as microscopic colitis, antibiotics associated infectious and ischaemic colitis[6]. The main pathologies of drug-induced gastrointestinal disease are ulceration, stricture formation, variable inflammatory processes and ischaemia.Within these overall major patterns, microscopic clues, such as apoptosis, cytoplasmic vacuolation, increased intraepithelial lymphocytes, melanosis coli and eosinophils, are pointers to a drug-induced pathology, though all are far from specific[2].
In 2004, Cappell comprehensively collected and critically reviewed the knowledge about potential triggers and mechanisms of drug-induced colontoxicity and categorised them into well-established and probable associations[7]. Suspected agents having well-established associations with colonic ischaemia include cocaine,ergotamine and estrogens, and probable associations include alosetron, digitalis,dopamine, (nor)epinephrine, methysergide, NSAIDs, vasopressin, barbiturates,diuretics and tricyclic antidepressants. Gold compounds, NSAIDs and potassium chloride are thought to cause allergic, cytotoxic or inflammatory colitis; probable associations comprise alpha-methyldopa, salicylates, selective COX-2 inhibitors,carbamazepine, cimetidine, simvastatine, methodrexate, bisaodyl, penicillamine,isoretinoin[1,7]. Other drugs, such as immune checkpoint inhibitors (i.e., ipilimumab)and neuroleptics, have recently been identified as causing colitis[5,8]. Multiples of the associations mentioned above, such as statin use, rely on a single case report[9], a series of case reports and case series[7]. Up to now, no study has investigated potential triggers in a larger cohort of histologically suspected DiC. Hence, we aimed to analyse DiC in comparison to two different age- and gender-matched control groups.
MATERIALS AND METHODS
Study population
We conducted a single-centre retrospective cohort study of patients undergoing colonoscopy with biopsy between 2006 and 2016, referred by the Department of Gastroenterology and Hepatology of the University Hospital Bergmannsheil gGmbH in Bochum, Germany (Supplementary Table 1 and Table 1). All patients of whom a histopathological report was available were considered eligible for inclusion.Outpatients were excluded from analysis due to insufficient information about medical history.
Patients were assigned to one of three groups based on histopathology: DiC, noninflammatory controls (NiC) and inflammatory colitis of another cause (IC) (Figure 1).Patients of both control groups were age- and gender-matched; DiC patients without matching patients were excluded. Histology of microscopic colitis, pseudomembranous colitis and radiation-induced injury were reasons for exclusion for DiC patients. Non-inflammatory controls consisted of patients with irritable bowel syndrome, functional disorders or colorectal cancer screening. Inflammatory controls included diverticulitis, inflammatory bowel disease and ischaemic colitis.
The primary histopathological assessment was validated in a second approach.From a clinical perspective, patients were divided into three groups: DiC without atherosclerosis, DiC with atherosclerosis, and ischaemic colitis. Patients from the first two groups derived from the DiC group while the latter group was gathered from the IC group. Hereby, 28 age- and gender-matched triplets were assembled.
Objectives
The aim of the study was to reveal associations between different agents and the presence of DiC. Secondary objectives were to describe the symptomatology, to identify cofactors that support the presence of DiC and to evaluate the reliability of the histopathological criteria.
Medical history
The electronic database and patient records have been reviewed to identify all drugs prescribed up to 21 d prior to colonoscopy. The specific agents were assigned to 36 different classes, as displayed in Supplementary Table 2.
Histopathological assessment
The histopathological assessment was performed by an expert pathologist based on international standards using haematoxylin and eosin stain including low- and highpower examination. Diagnosis of DiC was based on mixed, predominantly neutrophilic or lymphocytic inflammatory infiltrates, erosions, absence of granulomas, absence of basal plasmacellular infiltration and absence of crypt architectural distortion. Laxative-, corticosteroid- or gold compound-associated damage and well-defined drug-induced conditions, such as microscopic, infectious(including clostridium-associated colitis) and neutropenic colitis, were not regarded as suitable for inclusion.
Histopathological reassessment
Representative biopsy specimens were re-evaluated using haematoxylin and eosin stain with a magnification of 100-fold and assessed regarding oedema, haemorrhage,lymphocytic, granulocytic or eosinophilic infiltration, erosions, ulcerous lesions,necrosis, fibrin plaques on erosions, and fibrosis. The same team of pathologistsevaluated the slides unaware of the former results and the respective group.
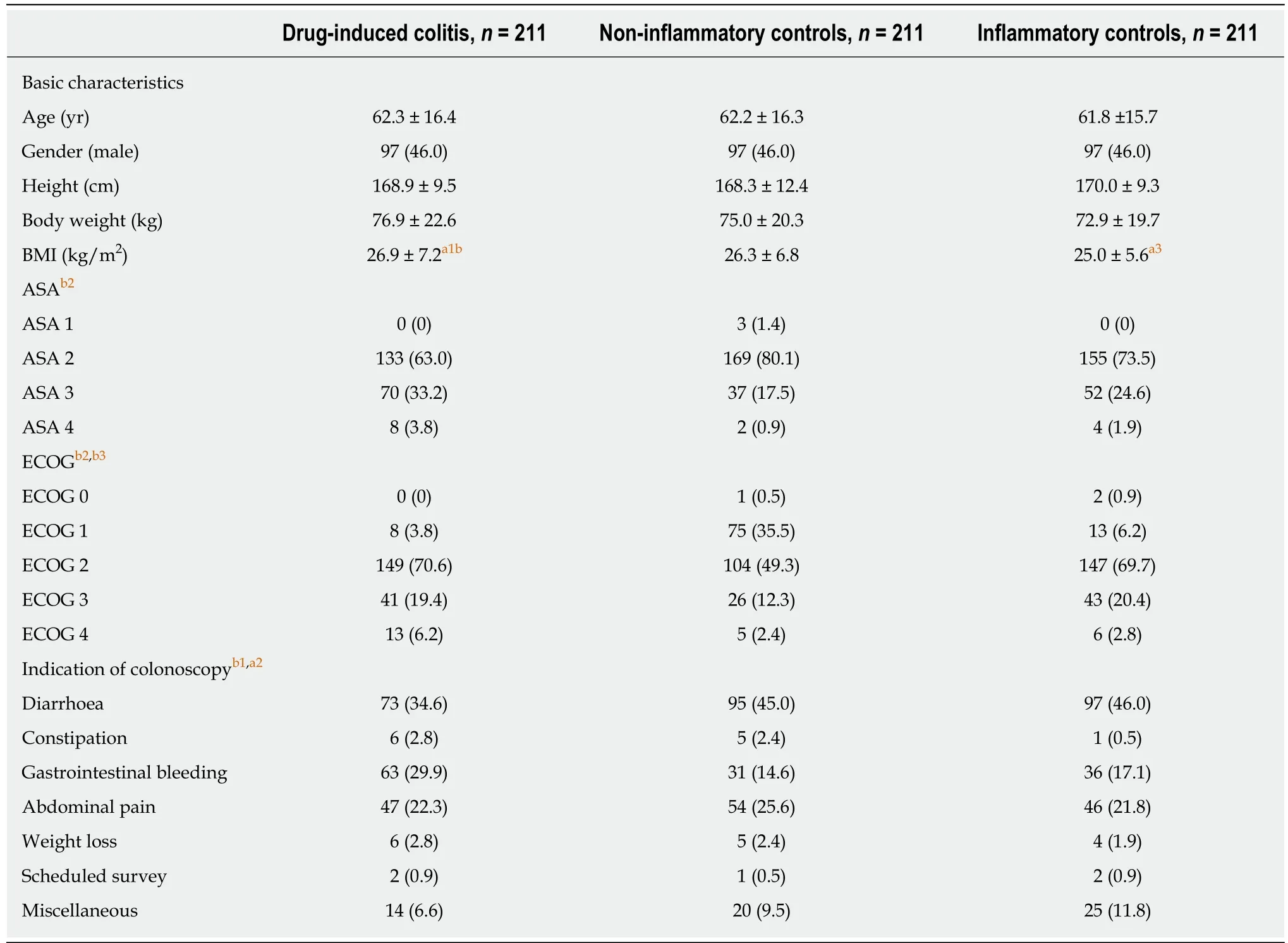
Table 1 Basic demographic characteristics n (%)
Statistical analysis
Statistical analysis was performed with SPSS Version 24 (IBM, Armonk, United States). Arithmetic mean and standard deviation were used for the evaluation of metric variables. Categorial data were stated as absolute and relative frequencies.Nominal variables, such as the dichotomous primary and secondary objectives, were compared using the chi-squared (χ2) test. Metric variables were analysed using the Analysis of Variance (ANOVA) and the two-tailed t-test. The binary logistic regression enter method was used for multivariate analysis. Analysis was considered statistically significant with a P-value ≤ 0.05.
Ethical concerns
The study protocol and amendment have been reviewed and approved by the institutional review board of the Ruhr-University Bochum (registration number 16-5963) based on the ethical guidelines of the Declaration of Helsinki and its later revisions. Written, informed consents were obtained from all patients before specific examinations and procedures such as colonoscopy and biopsy. For this retrospective study informed consent was neither practicable nor necessary and was exempted by the institutional review board of the Ruhr-university.
RESULTS
Basic characteristics
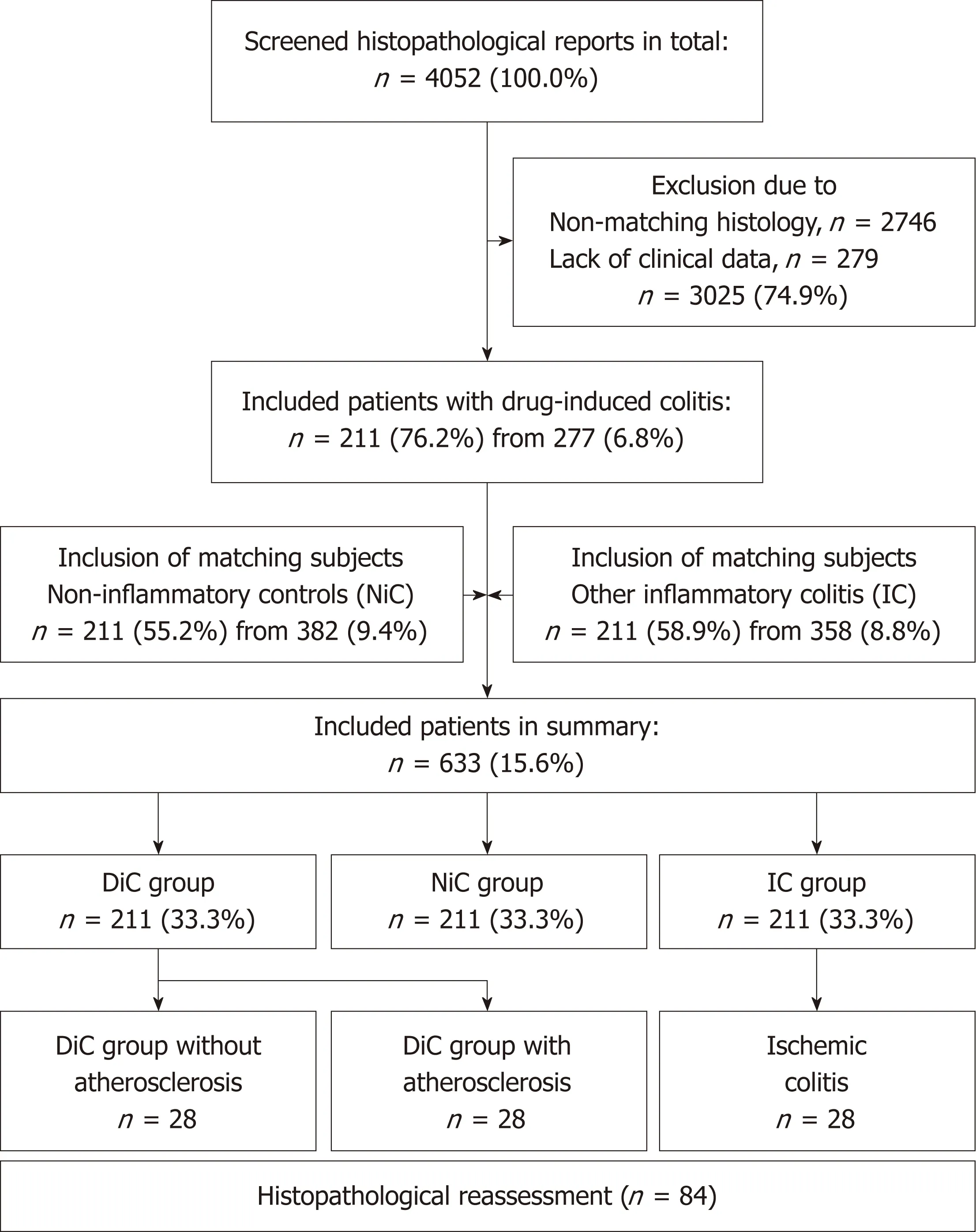
Figure 1 Flow-chart of inclusion. DiC: Drug-induced colitis; NiC: Non-inflammatory controls; IC: Inflammatory controls.
A total of 633 patients (291 male patients, mean age 62.1 ± 16.1 years) were included(Figure 1). Matching referring to gender and age resulted in homogenous groups with 211 subjects in either one (Supplementary Table 3). Medium body mass index (BMI)was 25.9 ± 6.1 kg/m2. Referring to American Society of Anaesthesiologist (ASA)scoring, DiC patients were characterised by higher grades, referring to the Eastern Cooperative Oncology Group (ECOG) scale, both DiC and IC patients were equally distributed, but revealed significantly higher scores than NiC patients. Indications for colonoscopy differed significantly; while diarrhoea predominated among both control groups, the major indication among DiC patients was gastrointestinal bleeding. Other indications, such as abdominal pain and scheduled survey, led to colonoscopy equally often.
Comorbidities
Most comorbidities were equally distributed, but some remarkable differences were found, as displayed in Table 2. Cardiac diseases were most common among the DiC group (52.1% vs 44.1% in NiC, P = 0.098 and 41.2% in IC, P = 0.025, χ2test). Heart failure was less frequent in the NiC group (7.6% vs 16.6% and 14.7%, P = 0.014, χ2test);atrial fibrillation did not differ. Coronary heart disease was most common among DiC patients (22.3% vs 12.3% and 16.6%, P < 0.001, χ2test). While peripheral arterial occlusive disease did not differ, the overall manifestations of atherosclerosis appeared nearly twofold more often among DiC patients (35.1% vs 18.5% and 19.0%, P < 0.001,χ2test). While most cardiovascular risk factors were equally distributed,hyperlipoprotenaemia was more common among DiC patients (10.4% vs 5.2% and 4.3%). Surgery during the same hospital stay was a relatively rare event but was overrepresented among the DiC patients (4.3% vs 0.5% and 1.4%, P = 0.024, χ2test).
Histological assessment
Histopathological patterns are displayed in Supplementary Table 4. Inflammatory features were rarely seen among the NiC group (between 0% and 14.7%), except for lymphoplasmacellular and granulocytic infiltration (40.3%). Oedema, erosions,regeneratory hyperplasia of the crypts and subepithelial haemorrhage occurred equally often among DiC and IC patients (24.2%, 35.5%, 12.3% and 16.4%,respectively). Ischaemia and ulcers were most common among the IC group (5.2% vs 0.5% and 14.7% vs 7.6%, P < 0.001, χ2test), while eosinophilia and mucosal fibrosis were reported most often in the DiC group (24.6% vs 21.8% vs 8.2%, P < 0.001 and 28.0% vs 21.8% vs 14.7%, P = 0.004, respectively).
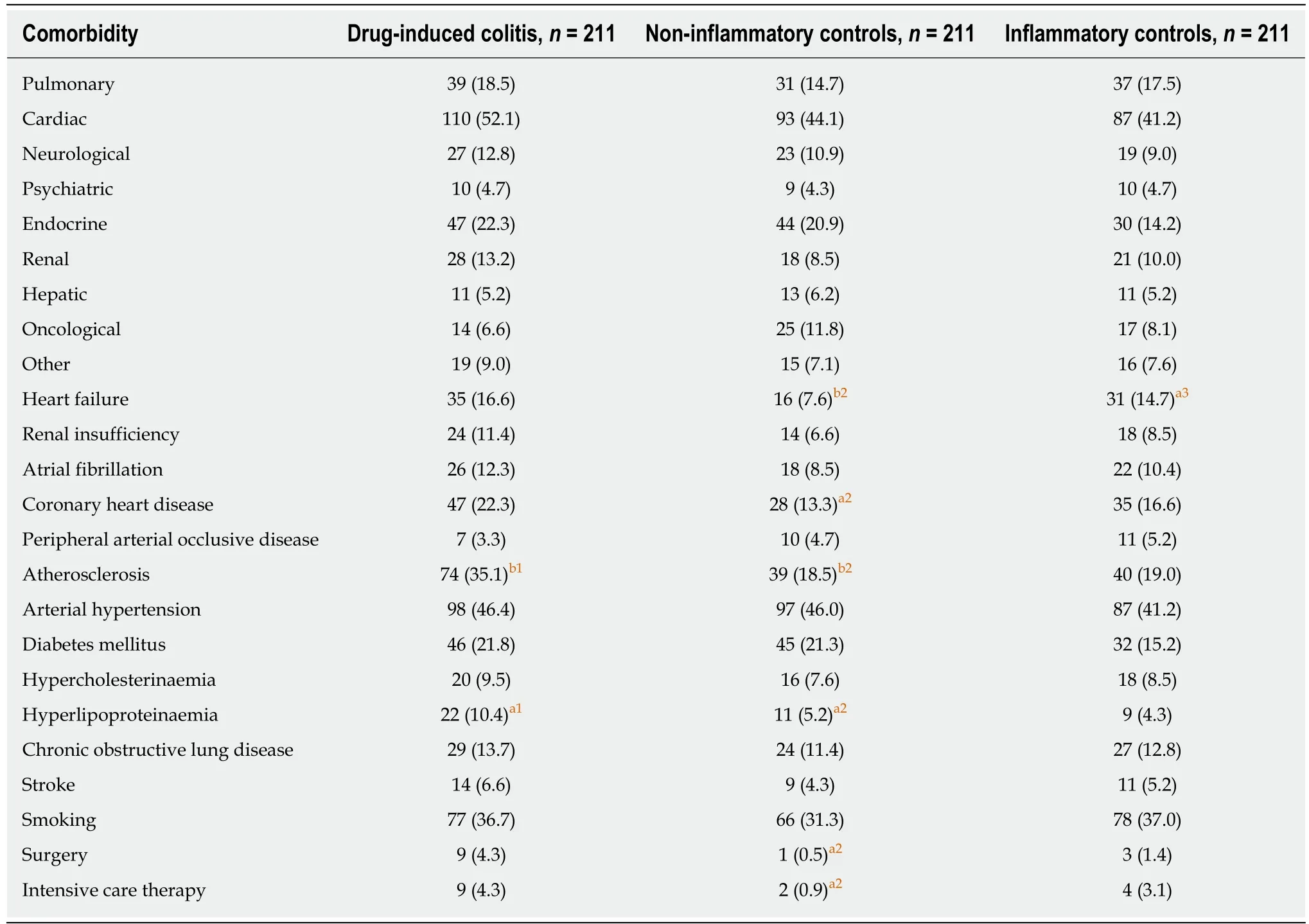
Table 2 Comorbidities n (%)
Histological reassessment
A total of 28 age- and gender-matched triplets (84 patients altogether) were assembled for the reassessment. Among them, two-thirds were female patients (n = 57, 67.9%,mean age 75.6 ± 7.6 years). The inflammatory activity in both DiC groups was predominantly mild (89.3% and 82.1%, respectively), while patients with ischaemic colitis were uniformly distributed between mild, moderate and severe inflammation(Supplementary Table 5). The inflammation in both DiC groups occurred significantly more often in the ascending colon compared to ischaemic colitis (Supplementary Table 6). The same tendency, but less pronounced, was present regarding the coecum.The histopathological reassessment revealed differences between both DiC groups and ischaemic colitis (Table 3 and Figure 2); for instance, eosinophilic infiltration was more common (42.9% and 25.0% vs 3.6%), while ulcers and necrosis occurred less frequently (14.3% and 10.7% vs 57.1% and 3.6% vs 57.1%, respectively). On the other hand, haemorrhage and erosions were equally present between DiC with atherosclerosis and ischaemic colitis but were more common than in the DiC group without atherosclerosis (28.6% and 21.4% vs 3.6% and 32.1% and 35.1% vs 7.1%,respectively). Oedema, lymphocytic and granulocytic infiltration, fibrin plaques and fibrosis were similar in both groups.
Drug assessment
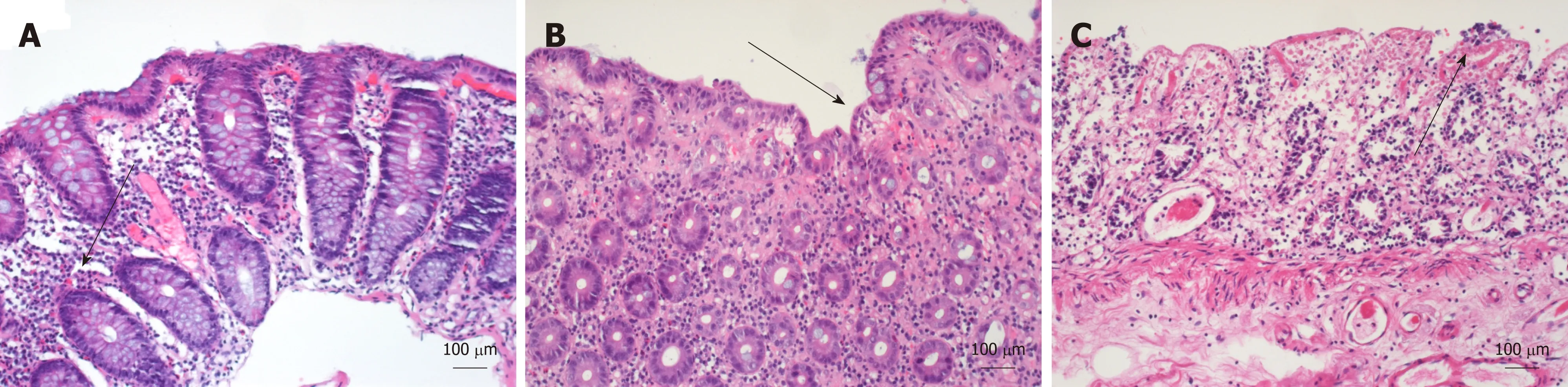
Figure 2 Histological appearance of drug-induced colitis with atherosclerosis, drug-induced colitis without atherosclerosis, and ischaemic colitis in hematoxylin and eosin stain. A: Drug-induced colitis (DiC) with atherosclerosis; B: DiC without atherosclerosis; C: Ischaemic colitis. Three different groups of 28 patients each were collected for histological reassessment. DiC with atherosclerosis (A) is characterised by lymphocytic, granulocytic and eosinophilic infiltration(marked with an arrow) while haemorrhage, necrosis is rarely present. In ischaemic colitis, (C) ulcers, necrosis (marked with an arrow), and erosions predominate, and haemorrhage and fibrosis also occur. Eosinophilic infiltrations are rarely seen. DiC without atherosclerosis (B) shows features of both DiC without atherosclerosis and ischaemic colitis. These include haemorrhage, eosinophilic infiltration and erosions (marked with an arrow).
Patients with DiC took significantly more drugs (mean 4.5 ± 2.8) than NiC (mean 3.9 ±3.0, P = 0.042) and tendentially more than IC patients (3.9 ± 3.2, P = 0.071). The frequencies of specific drug classes are detailed in Table 4. Betablockers, angiotensinconverting enzyme (ACE) inhibitors, benzothiazines, aldosterone antagonists,nitrates, antiarrhythmic drugs, glycosides, metamizole, potassium, vitamin K antagonists, direct thrombin inhibitors, insulin, proton pump inhibitors, thyreostatics,antibiotics, tricyclic antidepressants, neuroleptics and sedatives were equally distributed between all three study groups.
Significant differences with the highest frequencies among DiC vs NiC vs IC patients were found regarding diuretics, dihydropyridines, glycosides, ASS (31.8% vs 22.3% vs 19.0%, P = 0.006), platelet aggregation inhibitors, NSAIDs, statins and fibrates.
The lowest frequencies in DiC vs NiC vs IC patients were found regarding nondihydropyridines. The lowest frequencies in IC vs DiC vs NiC patients were found regarding angiotensin II inhibitors and metformin. The highest frequencies in IC vs DiC vs NiC group were found regarding glucocorticosteroids and other unspecified drugs. The highest frequency among the NiC vs DiC vs IC group was found for levothyroxine and lowest for selective serotonin reuptake inhibitors (SSRIs).
Among the reassessment subgroups (Supplementary Table 7), DiC patients without atherosclerosis took significantly fewer drugs than both other subgroups (4.8 ± 2.5 vs 6.6 ± 2.3, P < 0.01). The use of beta blockers, dihydropyridines, ASS and aldosterone antagonists was lower, though not significantly; statin use was significantly lowest(10.7% vs 60.7% vs 46.4%, P < 0.01). All other drug classes, including fibrates and NSAIDs, were distributed equally; particularly, there were no remarkable differences between DiC patients with atherosclerosis and ischaemic colitis patients.
Echocardiographic parameters
Heart ultrasound was available from 111 patients (17.5%), among them were 54 DiC(25.6%), 34 NiC (16.1%) and 23 IC (11.4%) patients (Table 5). Global left ventricular function was significantly better in NiC patients than in both other groups (P < 0.05)in which normal function was present in 72.2% (DiC) and 73.9% (IC), respectively.There was no moderate or severe decrease among NiC, while DiC patients presented in 9.3% and 11.1% and IC patients in 8.7% and 13.0%, respectively. Additionally,dilation of the left ventricular was reported in none of the NiC patients, but in 14.8%of DiC and even 26.1% of the IC patients (P = 0.036, χ2test). Dilation of the right atrium was reported in 7.4% of DiC patients, 11.4% of NiC and 23.8% of IC patients (P= 0.142, χ2test). No differences occurred regarding hypokinesia or diastolic dysfunction. Limited sample size among the reassessment groups inhibited the subgroup analysis.
Binary logistic regression models
Different models of binary logistic regression analysis were calculated (Table 6). The model comparing DiC patients and NiC that contained the variables chronic heart failure, any manifestation of atherosclerosis, on the one hand, and dihydropyridines,diuretics, digitalis glycosides, low-dose aspirin, any other platelet aggregation inhibitor, NSAIDs, statins and fibrates, on the other hand, revealed a statistically significant model (Omnibus test P < 0.001; Hosmer-Lemeshow test P = 0.598) with low predictive power (Nagelkerke’s R2 = 0.109). In this model, only NSAIDs (P =0.010) and fibrates remained statistically significant, while atherosclerosis (P = 0.087)and diuretics (P = 0.070) showed a persisting tendency. The related odds ratios were 2.2 (CI: 1.2-4.0) and 8.9 (CI: 1.1-74.2), respectively. The resembling models without dihydropyridines or additional ASA or ECOG score showed comparable results (data not shown).
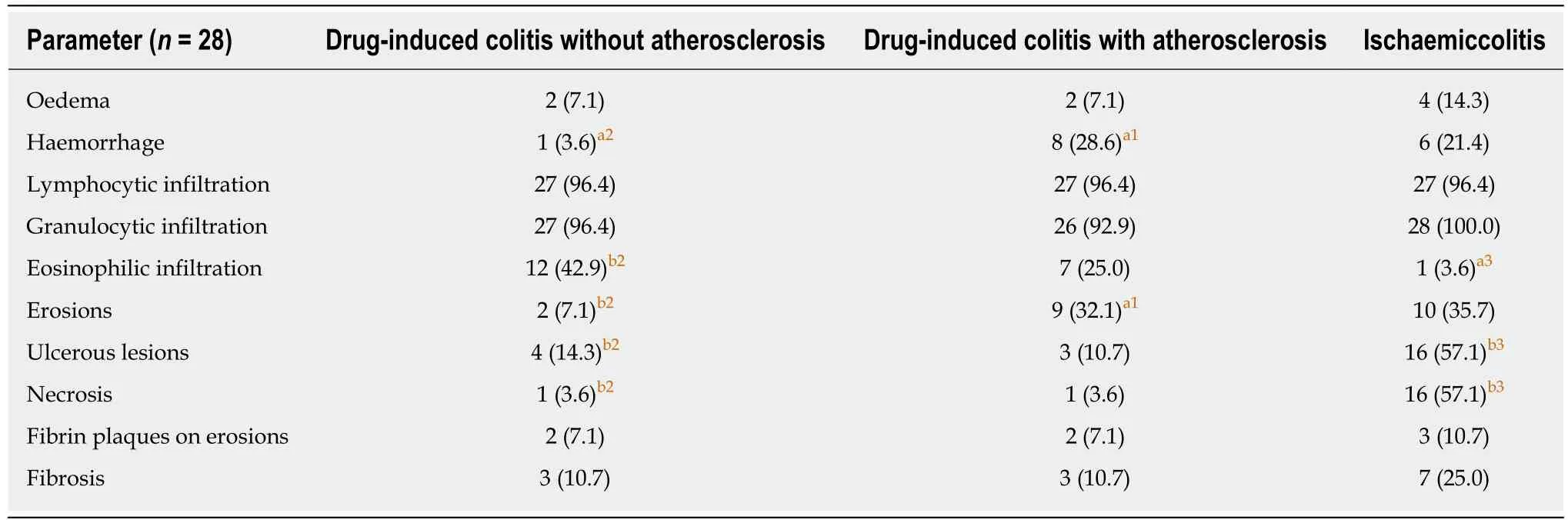
Table 3 Histopathological reassessment n (%)
The same model comparing DiC and IC patients revealed a higher but still low predictive power (Omnibus test P < 0.001; Hosmer-Lemeshow test P = 0.432,Nagelkerke’s R2 = 0.170). Significant variables comprised atherosclerosis (P = 0.009),NSAIDs (P < 0.001) and fibrates (P = 0.043) while aspirin showed only a tendency (P =0.059). The related ORs were 2.1 (CI: 1.2-3.7), 6.7 (CI: 3.0-15.1) and 9.1 (CI: 1.1-76.4).Skipping dihydropyridines or adding the ASA or ECOG score did not change the results substantially (data not shown).
DISCUSSION
In this age- and gender-matched retrospective cohort study, DiC was detected in about 7% of endoscopically sampled biopsy specimens of the colon mucosa. This prevalence coincides well with estimated numbers from a recently published overview[6,10]. Nevertheless, DiC (despite clostridium-associated[11,12]and microscopic colitis[13]) is a rarely reported entity in the literature and most knowledge derives from case reports or case series[7]. Therefore, to the best of our knowledge, this is the first study that systematically investigates a large set of potential triggers of DiC.
Potential triggers of DiC
In univariate analysis, DiC was associated with diuretics, dihydropyridines,glycosides, ASS, platelet aggregation inhibitors, NSAIDs, statins and fibrates. In addition to NSAIDs, that are well established to induce DiC[10,14,15], several drugs that are indicated for the treatment of heart failure, atherosclerosis and related conditions(such as fat-lowering medication) were associated with DiC. Cardiac and vascular comorbidity might, therefore, be a substantial confounding factor or the cause of the disease itself.
Several aspects were undertaken to control confounding factors. Two age- and gender-matched control groups were gathered, one of which consisted of patients with NiC while the other group was assembled from patients with IC. This matching resulted in rather equally distributed comorbidities and only a very few entities differed significantly. While overall cardiac comorbidity and atrial fibrillation were equally distributed between all three groups, atherosclerosis, particularly coronary heart disease, and hyperlipoproteinaemia were more common among DiC patients.Heart failure occurred similarly in the DiC and IC group, but more often than in NiC.Echocardiography was available for only a minority of patients (between 11% and 26%, respectively), but did not show restricted function among DiC patients. In detail,the left ventricular function did not differ between DiC and IC patients, while NiC patients preferentially showed a preserved ejection fraction. Dilation of the leftventricle and right atrium were most common among IC patients, while hypokinesia or diastolic dysfunction were the same among all three groups.
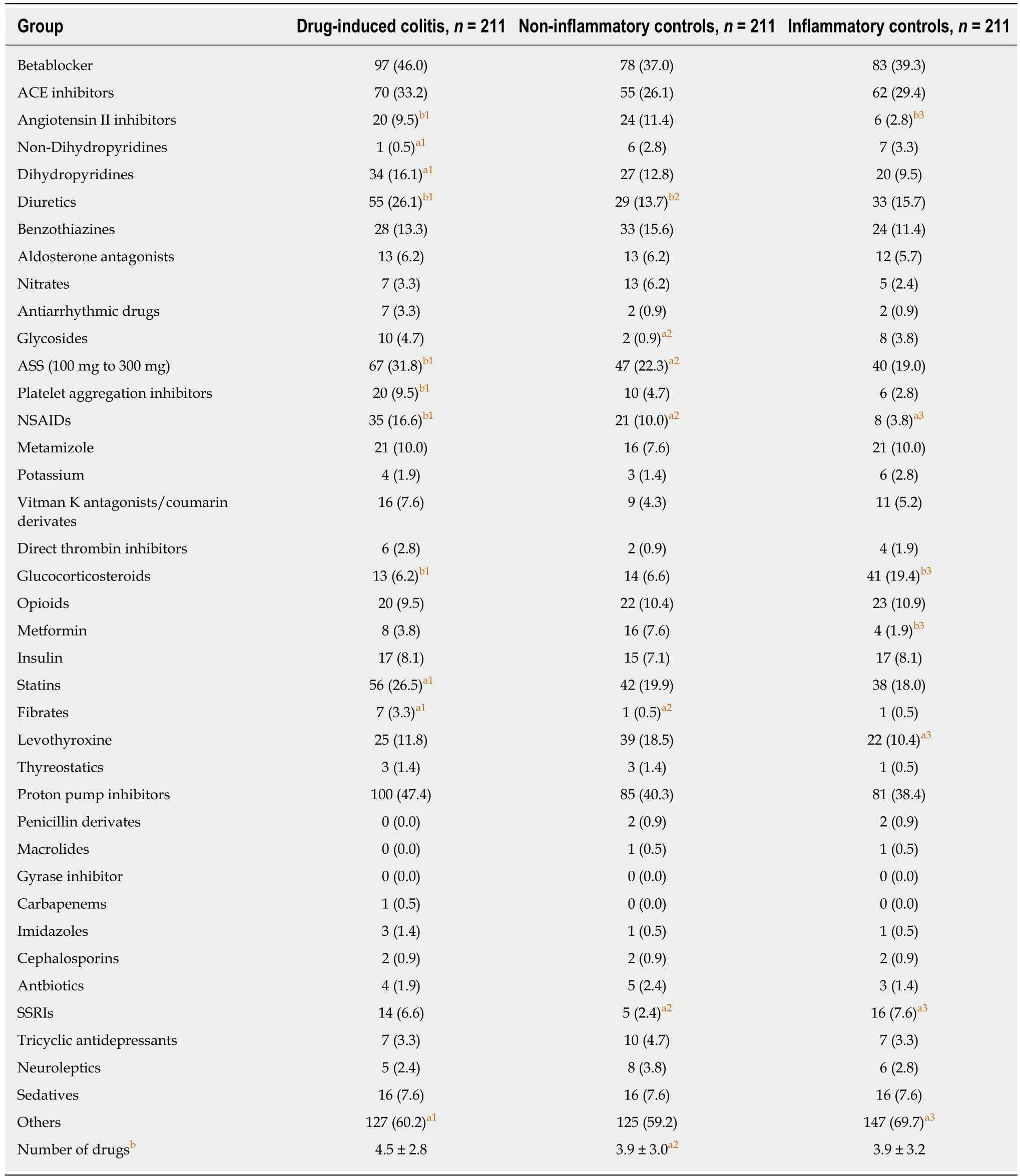
Table 4 Drug assessment n (%)
Only fibrates (OR = 9.1), NSAIDs (OR = 6.7), and atherosclerosis (OR = 2.1) proved to be associated with DiC in the multivariate analysis, while heart failure,dihydropyridines, glycosides, diuretics, low-dose aspirin, platelet aggregationinhibitors and statins lost their relevance. The effects of NSAIDs on the gastrointestinal tract have been extensively investigated, however, the association of fibrates and the role of atherosclerosis are novel findings.
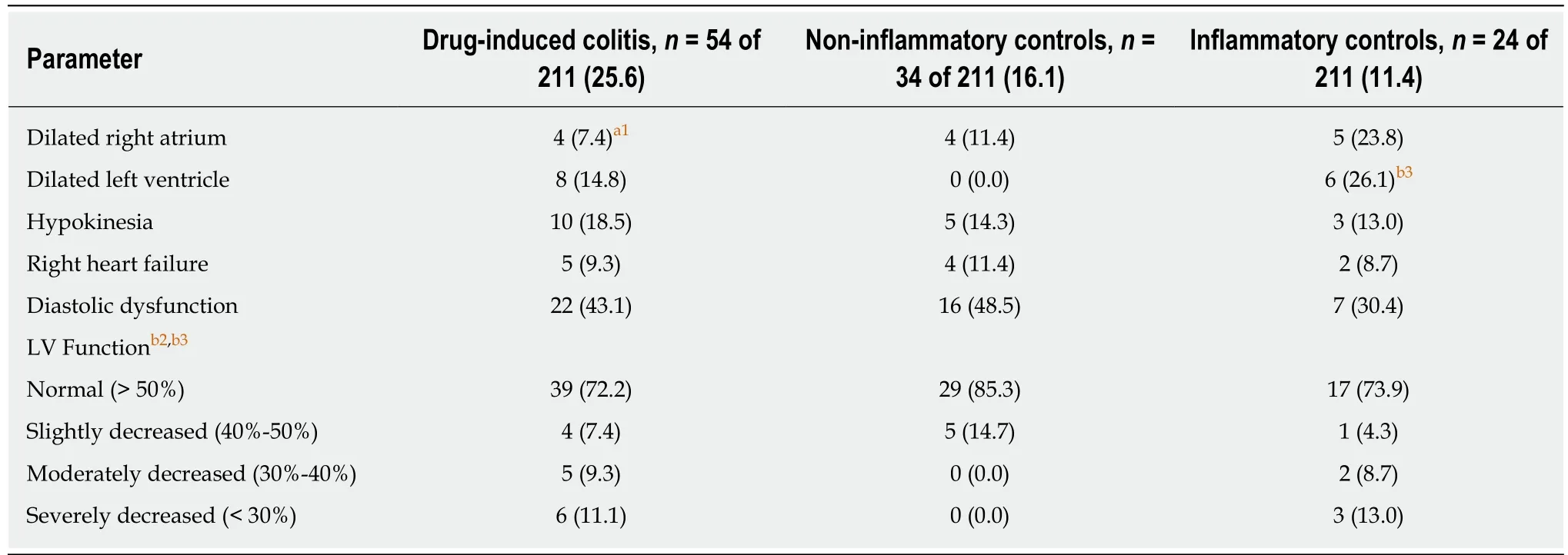
Table 5 Echocardiographic parameters n (%)
Pathogenetic role of ischaemia
It has been proposed that medications can cause colonic ischaemia due to neuronal stimulation (e.g., cocaine), by promoting thrombosis due to hormonal effects (e.g.,estrogen) or by extrinsic compression due to fibrosis (e.g., methysergide). Other drugs may promote colonic ischaemia by shunting blood away from the mesenteric vasculature (e.g., digitalis[16]) by decreasing fluid volume (e.g., diuretics[17]), inducing vasculitis or vascular spasms, or by other, not yet understood mechanisms[2,7,18,19]. It was hypothesised that drugs, such as digitalis and diuretics, may predispose to ischaemic colitis in elderly patients in a state of low blood flow, often due to heart failure[6], but up to now, there has been no proof of this concept. The overall results support the idea of disturbances in microperfusion at least in a subset of patients,maybe those patients with underlying atherosclerosis.
The subgroup analysis of either 28 matched DiC patients without atherosclerosis,with atherosclerosis and patients with ischaemic colitis further strengthens this concept. The DiC patients without atherosclerosis took significantly fewer remedies than both other subgroups and used beta blockers, dihydropyridines, ASS and aldosterone antagonists less often, though not significantly. While statin intake was significantly highest among the DiC subgroup with atherosclerotic manifestations, all other drug classes, including fibrates and NSAIDs, diversified similarly; there were no specific remarkable differences between DiC patients with atherosclerosis and ischaemic colitis patients. Indeed, this distribution does not prove but at least gives a distinct clue that atherosclerosis and focal hypoxia play a substantial role in the aetiopathogenesis of DiC in a subset of patients.
Reliability of histopathological assessment
The presence of DiC in the routine histological assessment was the major inclusion criterion. The pathological changes of neither drug-induced nor ischaemic colitis are specific and significant histological overlap exists between both entities[2,18,20].Nevertheless, acute ischaemic colitis is observed predominantly in elderly (older than 65 years) subjects[21], while the patients of our cohort were distinctly younger (62 years). None of the three different histologic variants of colitis with ischaemic features that Jessurun recently distinguished has been included in the DiC group[20]. Given the common absence of strictly specific histopathological features, the diagnosis of DiC often relies upon thorough clinicopathological correlation, but in clinical practice it is difficult to establish the correlation between a certain medication and a particular pattern of injury. The optimal establishment of a causal relationship that results from improvement with withdrawal and recurrence with rechallenge of the suspected agent is rarely available and was not a common practice in our cohort. This approachis hardly realisable when dealing with a single patient who most commonly takes a multitude of drugs; the mean number in our cohort summed up to 4.5 different agents. Thus, it is the pathologist’s task to offer a strong suspicion concerning possible drug-related pathology[19].
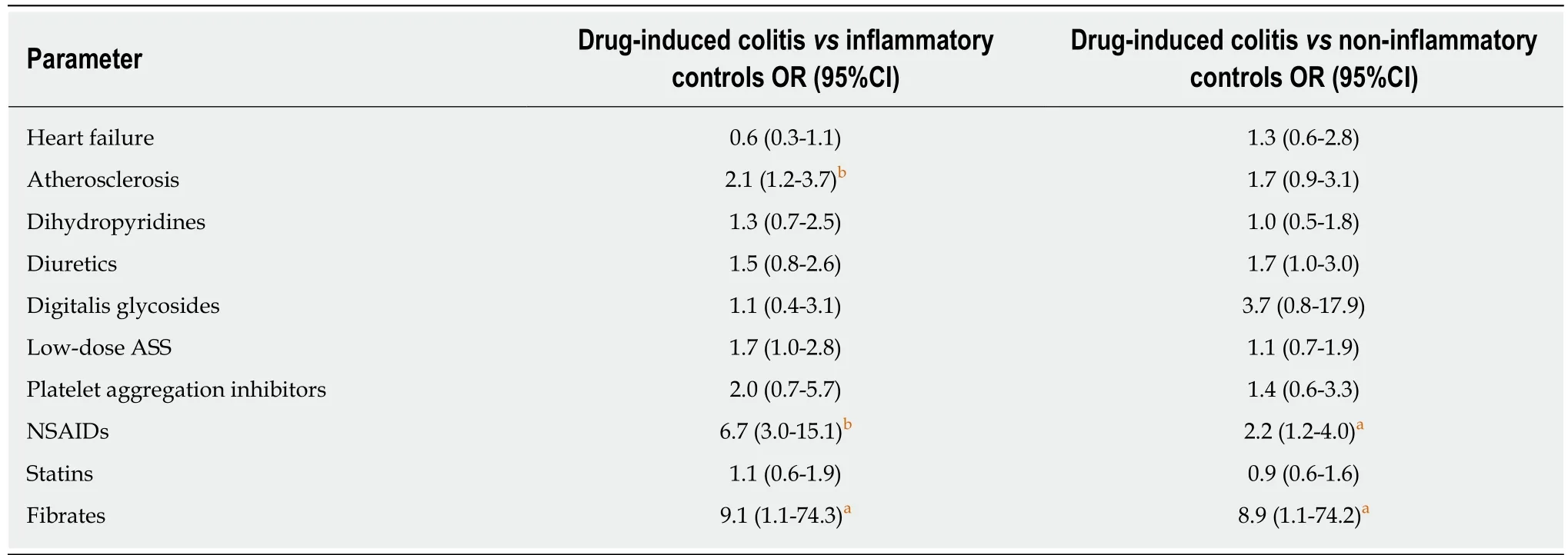
Table 6 Binary logistic regression analysis
The biopsy specimens were reassessed in a subset of patients and compared in three different groups: DiC patients with atherosclerosis, DiC patients without atherosclerosis and patients with ischaemic colitis, to gain deeper insights into the reliability of the histopathological assessment. Patients of both DiC groups presented milder inflammatory activity, suggesting common pathophysiological pathways that can be distinguished from purely ischaemic colitis. Indeed, DiC patients with atherosclerosis exhibited features from both DiC without atherosclerosis and ischaemic colitis: Haemorrhage and erosions were the same among atherosclerotic DiC and ischaemic colitis patients, while the presence of ulcers and necrosis were equal in both DiC groups. Interestingly, infiltration with eosinophils that is characteristic for DiC2were found most often in the DiC group without atherosclerosis, while it rarely appeared among the ischaemic colitis group (42.9% vs 3.6%); atherosclerotic DiC patients ranked in between (25.0%). We, therefore, conclude that focal ischaemia due to disturbances of the microcirculation, probably supported by large vessel atherosclerosis, plays a substantial role particularly in a subset of patients with DiC.
Strengths and limitations
Most patients with acute colitis are diagnosed and treated based on a combination of clinical and laboratory findings without colonoscopy and mucosal biopsy analysis.Endoscopic evaluation is reserved for patients who present with severe or atypical clinical course, do not improve within an expected timeframe or fail to respond to standard treatment[20]. Therefore, the inclusion of histologically suspected DiC bears a potential selection bias. The histopathological approach was limited to colonic manifestations with morphological changes, while functional diarrhoea, alterations on a (sub)cellular level or manifestations of the small intestine were beyond the scope of the study. Despite all potential limitations, this is the largest study that investigates potential triggers of DiC and potential confounders systematically. The fact that NSAID use has clearly been shown to induce DiC[10,14]could have been reproduced in our cohort argues seriously for the reliability of the approach chosen.
CONCLUSION
In conclusion, histopathologically suspected DiC is associated with not only NSAIDs,angiotensin II inhibitors, dihydropyridines, diuretics, ASS and other platelet aggregation inhibitors, as well as statins and fibrates, but also coronary heart disease,hyperlipoproteinaemia and, partially, heart failure. Atherosclerosis (OR = 2.1) and the intake of NSAIDs (OR = 6.7) and fibrates (OR = 9.1) were associated most strongly with DiC in the multivariate analysis. Since a subset of DiC patients with atherosclerosis exhibited histological features of both DiC without atherosclerosis and ischaemia, we propose that focal disturbances of the microcirculation play a substantial role in the pathogenesis of a subgroup of DiC patients. The distribution of drug intake further supports this hypothesis, but the study design is not suitable to prove it. Prospective studies including larger cohorts with clearly defined cardiac function, pattern and severity of atherosclerosis and related comorbidities, such as hyperlipoprotenaemia, are warranted to unravel the underlying aetiology and pathophysiology of this under-recognised entity. Meanwhile, the histological suspicion of DiC might not necessarily reveal a drug-related mechanism but could also reflect focal ischaemia that is supported by macroangiopathy at least in a subset of patients.
ARTICLE HIGHLIGHTS
Research background
Drug-induced colitis is a common and even serious problem, but the knowledge about associated triggers is scarce.
Research motivation
Withdrawal of the respective trigger should cure the disease, so that its identification is crucial.Therefore, deeper insights into the aetiopathogenesis and knowledge about potential triggers is mandatory.
Research objectives
Consequently, the study aimed to identify potential triggers of histologically suspected druginduced colitis.
Research methods
A retrospective case control study of 211 patients with histologically suspected drug-induced colitis and two age- and gender matched control groups was performed. The drug-induced colitis (DiC) patients showed histological changes attributable to drug-induced pathology, i.e.,mixed, predominantly neutrophilic or lymphocytic inflammatory infiltrates, erosions, absence of granulomas, absence of basal plasmacellular infiltration and absence of crypt architectural distortion. The control groups consisted of patients with inflammatory colitis other than DiC and inflammatory bowel disease (i.e., diverticulitis, ischaemic colitis) and of patients without substantial histological changes (i.e., irritable bowel syndrome, cancer screening). Clinical data including drug history was obtained from the electronic data base.
In a second approach, patients were divided into three groups from a clinical perspective: DiC without atherosclerotic comorbidity, DiC with atherosclerotic comorbidity, and ischaemic colitis.Patients from the first two groups derived from the DiC group while the latter group was gathered from the inflammatory controls.
Research results
A total of 633 patients (291 male patients, mean age 62.1 ± 16.1 years) were included. Patients with DiC took more drugs (mean 4.5 ± 2.8) than patients from both other groups (mean 3.9 ± 3.0 and 3.9 ± 3.2, respectively). In univariate analysis, DiC was associated with diuretics,dihydropyridines, glycosides, ASS, platelet aggregation inhibitors, nonsteroidal antiinflammatory drugs (NSAIDs), statins and fibrates. In addition to NSAIDs, that are well established to induce DiC, several drugs that are indicated for the treatment of heart failure,atherosclerosis and related conditions were associated with DiC. Cardiac and vascular comorbidity might, therefore, be a substantial confounding factor or the cause of the disease itself. In fact, atherosclerosis was more common among patients with DiC. In multivariate analysis, atherosclerosis (OR = 2.1) and the intake of NSAIDs (OR = 6.7) and fibrates (OR = 9.1)were associated most strongly with DiC. Since a subset of DiC patients with atherosclerosis exhibited histological features of both DiC without atherosclerosis and ischaemia, we propose that focal disturbances of the microcirculation play a substantial role in the pathogenesis of a subgroup of DiC patients. A total of 28 age- and gender-matched triplets were assembled for the histological reassessment. Some DiC patients with atherosclerosis exhibited histological features of both control groups, DiC without atherosclerosis and ischaemia.
Research conclusions
While most knowledge of drug-induced colitis relies on case reports and case series this is the first study that systematically investigates potential triggers of DiC. This large case control study reveals that patients with the histopathological suspicion of drug-induced colitis take more different drugs than age- and gender-matched control patients. Associated remedies include drugs that are indicated for the treatment of heart failure, atherosclerosis and related conditions.Furthermore, atherosclerosis was more common among DiC patients. We therefore hypothesise that focal disturbances of the microcirculation play a substantial role in the pathogenesis of a subgroup of DiC patients, but the study design is not suitable to prove this hypothesis.
Research perspectives
Prospective studies including larger cohorts with clearly defined cardiac function, pattern and severity of atherosclerosis and related comorbidities, such as hyperlipoprotenaemia, are warranted to unravel the underlying aetiology and pathophysiology of this under-recognised entity. Meanwhile, the histological suspicion of DiC might not necessarily reveal a drug-related mechanism but could also reflect focal ischaemia that is supported by macroangiopathy at least in a subset of patients.
杂志排行
World Journal of Gastroenterology的其它文章
- Current and future pharmacological therapies for managing cirrhosis and its complications
- Outcomes of per oral endoscopic pyloromyotomy in gastroparesis worldwide
- Dbx2 exhibits a tumor-promoting function in hepatocellular carcinoma cell lines via regulating Shh-Gli1 signaling
- Dynamic changes of key metabolites during liver fibrosis in rats
- Procyanidin B2 protects against diet-induced obesity and nonalcoholic fatty liver disease via the modulation of the gut microbiota in rabbits
- Women on the liver transplantation waitlist are at increased risk of hospitalization compared to men