Current and future pharmacological therapies for managing cirrhosis and its complications
2019-03-09DavidKockerlingRooshiNathwaniRobertaForlanoPinelopiManousouBenjaminMullishAmeetDhar
David Kockerling, Rooshi Nathwani, Roberta Forlano, Pinelopi Manousou, Benjamin H Mullish, Ameet Dhar
Abstract Due to the restrictions of liver transplantation, complication-guided pharmacological therapy has become the mainstay of long-term management of cirrhosis. This article aims to provide a complete overview of pharmacotherapy options that may be commenced in the outpatient setting which are available for managing cirrhosis and its complications, together with discussion of current controversies and potential future directions. PubMed/Medline/Cochrane Library were electronically searched up to December 2018 to identify studies evaluating safety, efficacy and therapeutic mechanisms of pharmacological agents in cirrhotic adults and animal models of cirrhosis. Non-selective betablockers effectively reduce variceal re-bleeding risk in cirrhotic patients with moderate/large varices, but appear ineffective for primary prevention of variceal development and may compromise renal function and haemodynamic stability in advanced decompensation. Recent observational studies suggest protective,haemodynamically-independent effects of beta-blockers relating to reduced bacterial translocation. The gut-selective antibiotic rifaximin is effective for secondary prophylaxis of hepatic encephalopathy; recent small trials also indicate its potential superiority to norfloxacin for secondary prevention of spontaneous bacterial peritonitis. Diuretics remain the mainstay of uncomplicated ascites treatment, and early trials suggest alpha-adrenergic receptor agonists may improve diuretic response in refractory ascites. Vaptans have not demonstrated clinical effectiveness in treating refractory ascites and may cause detrimental complications. Despite initial hepatotoxicity concerns, safety of statin administration has been demonstrated in compensated cirrhosis. Furthermore,statins are suggested to have protective effects upon fibrosis progression,decompensation and mortality. Evidence as to whether proton pump inhibitors cause gut-liver-brain axis dysfunction is conflicting. Emerging evidence indicates that anticoagulation therapy reduces incidence and increases recanalisation rates of non-malignant portal vein thrombosis, and may impede hepatic fibrogenesis and decompensation. Pharmacotherapy for cirrhosis should be implemented in accordance with up-to-date guidelines and in conjunction with aetiology management, nutritional optimisation and patient education.
Key words: Cirrhosis; Beta-blockers; Rifaximin; Diuretics; Statins; Proton pump inhibitors; Pharmacology
INTRODUCTION
Decompensation and mortality in cirrhosis are predominantly due to the complications of portal hypertension, and prognosis in cirrhosis progressively deteriorates with the cumulative occurrence of ascites, variceal haemorrhage, hepatic encephalopathy (HE) and spontaneous bacterial peritonitis (SBP)[1]. While both cirrhosis incidence and prevalence have risen in recent decades, uptake of liver transplantation – the only definitive treatment option for cirrhosis - has stagnated at around 5500/year in Europe, primarily due to organ shortages[2]. Consequently,standardised cirrhosis mortality rates globally, and in the United Kingdom particularly, have increased significantly[3]. This development led to the United Kingdom-wide introduction of specialist cirrhosis clinics which integrate multidisciplinary services and aim to optimise supportive cirrhosis management by forestalling decompensation and facilitating recompensation. In the specialist clinic setting, one factor which has gained importance in chronic cirrhosis management is long-term, complication-guided pharmacological therapy. Whilst previous articles have addressed individual pharmacological agents and their role in treating specific complications of cirrhosis, the present article aims to provide an overview of the complete pharmacotherapy currently available for the long-term management of cirrhotic outpatients as well as an insight into emerging and future directions.
METHODS
A search of the existing literature up to December 2018 was conducted using the electronic databases PubMed, Medline and the Cochrane library, as well as relevant guidelines and reference lists. Titles and abstracts were searched for the following key terms: “Cirrhosis” and (“beta-blockers” or “lactulose” or “rifaximin” or “L-ornithine L-aspartate (LOLA)” or “acarbose” or “diuretics” or “midodrine” or “clonidine” or“vaptans” or “human serum albumin” or “anti-coagulation” or “caffeine” or “faecal microbiota transplant”). A separate search was performed for international guidelines to cirrhosis management by the American Association for the Study of Liver Diseases(AASLD) and the European Association for the Study of the Liver (EASL).Additionally, reference lists of included articles were manually screened for further relevant publications. The abstracts of 2031 publications were identified and screened for studies evaluating the safety, efficacy and therapeutic mechanism of pharmacological agents in cirrhotic adults and animal models of cirrhosis. 158 publications were considered relevant to the key question and included in the present review (Figure 1). Only articles published in English were included.
CURRENTLY-USED MEDICATIONS
Beta-blockers
Presently, non-selective beta-blockers (NSBB) are the only drug class endorsed for the long-term treatment of portal hypertension[4,5]. Along with endoscopic band ligation,NSBBs are employed for primary and secondary prophylaxis against variceal haemorrhage, as they combat the hyperkinetic portal-hypertensive syndrome by decreasing cardiac output and portal inflow (β-1 receptor blockade) and by achieving splanchnic vasoconstriction and reducing azygos blood flow (β-2 receptor blockade)[1,6-8]. Thus they efficaciously lower the risk of variceal bleeding and rebleeding as evidenced by several randomized controlled trials (RCT)[9-11].
Recent concerns about beta-blockers:These trials, however, predominantly excluded patients with advanced decompensation, and recent studies have voiced concerns over the safety of beta-blockers in decompensated patients with refractory ascites or SBP and in cirrhotic patients with alcoholic hepatitis[12-14]. In a prospective cohort study of 151 patients with refractory ascites by Sersté et al[12], 1-year survival was significantly lower in patients who received propranolol (19%) compared to patients not on beta-blocker therapy (64%). In another retrospective cohort study by Sersté et al[13]including 139 cirrhotic patients with severe alcoholic hepatitis, cumulative incidence of acute kidney injury (AKI) was significantly higher in the group receiving beta-blockers (89.6%) vs the group not receiving beta-blockers (50.4%). In a retrospective analysis of 607 cirrhotic patients by Mandorfer et al[14], NSBB therapy was associated with increased transplant-free survival in patients without SBP, but with decreased transplant-free survival, increased length of non-elective hospitalisation and increased rates of hepatorenal syndrome (HRS) in patients with SBP. Pathophysiologically, circulating blood volume depletion during large volume paracentesis for refractory ascites and the systemic inflammatory response during SBP may threaten the already limited cardiac reserve of decompensated patients, while beta-blockade further impairs restoration of renal and systemic perfusion pressures[7].Furthermore, patients with advanced stages of decompensation and a more amplified hyperdynamic circulation are likely to receive higher doses of beta-blockers, thus exaggerating detrimental effects on systemic haemodynamics. Accordingly, a retrospective nationwide study of 3719 Danish patients with cirrhosis found a reduction in mortality for propranolol doses < 160 mg/d but an increase in mortality for doses > 160 mg/d[15].
The ‘window hypothesis’:Consequently, the ‘window hypothesis’ by Krag et al[16]proposes the existence of a specific time frame of opportunity during the natural course of cirrhosis, only within the bounds of which NSBB therapy exerts beneficial effects on survival. It is propositioned that the window opens with the development of moderate/large varices and closes during advanced cirrhosis with the advent of refractory ascites, SBP, HRS or with the occurrence of alcoholic hepatitis[6,16]. An elegantly-designed randomized controlled trial by Groszmann et al[17]demonstrated that NSBBs are ineffective in the pre-primary prophylaxis of variceal development and even result in adverse effects in patients without varices, since the absence of a hyperdynamic circulation in patients with subclinical portal hypertension (Hepato-Venous Pressure Gradient (HVPG) < 10 mmHg) attenuates the portal pressure lowering effects of beta-blockers[18,19]. A more recent meta-analysis by Kumar et al[20]also found no difference in incidence of first variceal haemorrhage and development of large varices comparing patients receiving beta-blockers and patients not receiving beta-blockers, yet a significantly higher rate of adverse events [relative risk (RR) 4.66,95% confidence interval (CI) 1.36–15.91] was observed in patients receiving betablockers. With cirrhosis progression, portal pressure heightens while effective circulating volume decreases as a result of splanchnic vasodilatation and raised portal inflow. At this level of disease progression, the drop in effective circulating blood volume is compensated for by enhanced sympathetic stimulation of the cardiocirculatory system in the context of preserved cardiac reserves[4,21]. It is precisely at this stage that NSBBs are proposed to effectively counteract portal hypertension and abrogate the hyperdynamic state, thus improving patient survival[4]. With further advancement of cirrhosis and portal hypertension, however, the cardiac response to stimuli such as volume depletion by variceal haemorrhage becomes limited and betablockade impedes restoration of systemic and renal perfusion pressures, thus negatively impacting patient survival[7,21]. In line with the ‘window hypothesis’, Kim et al[22]conducted a nested case-control study in patients awaiting liver transplantation,matching 205 patients with AKI to 205 patients without AKI. On multivariate analysis, patients with ascites receiving beta-blockers had a 3-fold increased [Hazard ratio (HR) 3.31] risk of developing AKI, while patients without ascites receiving betablockers had a 5-fold reduced (HR 0.19) risk of developing AKI[21,22].
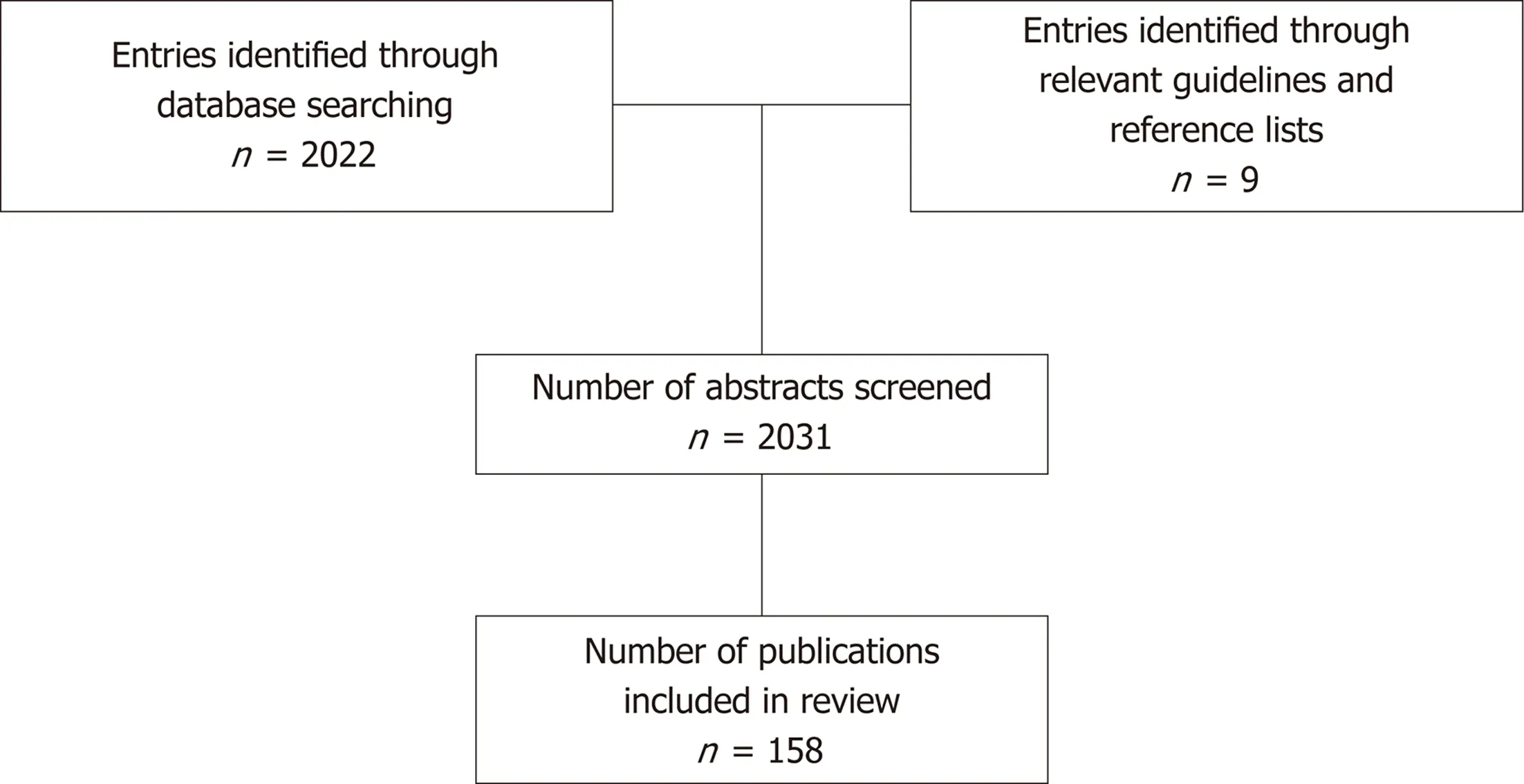
Figure 1 Flow diagram of study inclusion.
As a consequence of these concerns, widespread withholding of NSBB therapy in patients with advanced cirrhosis ensued. Yet, data from additional studies, performed after this initial apprehension had surfaced, provide counteracting evidence. A recent post-hoc analysis of 1188 patients with cirrhotic ascites from three satavaptan RCTs showed no association between NSBB therapy and increased mortality[23]. Similarly, a retrospective study by Leithead et al[24](105 beta-blocker users propensity risk score matched to 105 beta-blocker non-users) correlated NSBB use with improved survival in patients with ascites awaiting orthotopic liver transplantation (HR 0.55, 95% CI 0.32-0.95), and even on subgroup analysis of patients with refractory ascites, betablockers remained independently associated with improved survival (HR 0.35, 95% CI 0.14-0.86). Furthermore, Onali et al[25]evaluated 316 consecutive cirrhotic patients with ascites undergoing assessment for liver transplantation. Beta-blockers were associated with reduced overall mortality (HR 0.55, 95% CI 0.33-0.94) and on sub-group analysis of patients with refractory ascites no difference in mortality was observed (HR 0.43,95% CI 0.20-1.11). The numerous observational studies investigating the risks and benefits of NSBBs in advanced cirrhosis are summarised in Table 1. A recent metaanalysis of three RCTs and 13 observational studies summarising the effect of NSBBs on mortality in cirrhotic patients with ascites found that survival was comparable between NSBB and control groups for both the overall population (HR 0.86, 95% CI 0.71-1.03, P = 0.11) and the refractory ascites subgroup (HR 0.90, 95% CI 0.45-1.79, P =0.76) with significant heterogeneity between included studies[26].
Carvedilol:With the hypothesis that these discrepancies regarding the effect of betablockers in patients with refractory and non-refractory ascites may be related to the type of beta-blocker administered, a meta-analysis of nine observational studies in cirrhotic patients with ascites by Njei et al[27]found that the traditional NSBBs propranolol and nadolol were not associated with increased mortality, but that carvedilol, a NSBB with additional anti-alpha-1-adrenergic receptor activity,demonstrated a statistically significant association with increased all-cause mortality(RR 1.75, 95% CI 1.06-2.90)[27]. Previous studies had shown that carvedilol is more potent in reducing HVPG than traditional NSBBs[28]and is able to achieve a haemodynamic response in a high percentage (56%) of non-responders to propranolol[29]. In rodents, carvedilol administration was shown to modulate inflammatory cytokine generation and augment antioxidant production, resulting in diminished liver fibrogenesis[30,31]. The anti-alpha-1 mediated reduction in intrahepatic resistance brought about by carvedilol may be of benefit to patients with less advanced portal hypertension, where intrahepatic resistance still constitutes a major factor in portal pressure[32]. While traditional beta-blockers were shown to be ineffective in the primary prevention of variceal development, carvedilol achieved a delay in progression of small to large varices from 18.7 to 20.8 mo in a RCT by Bhardwaj et al[33]. However, carvedilol also shows a trend towards a more potent reduction in systemic arterial pressure compared to traditional beta-blockers[19,28]and could thus further destabilise the delicately-balanced haemodynamic state in cirrhotic patients with ascites, as Njei et al[27]hypothesise in view of the detrimental effect of carvedilol on their cohort. In contrast, Sinha et al recently investigated the effects oflong-term, low-dose (12.5 mg) carvedilol treatment in a retrospective, propensity score matched cohort of 264 patients with ascites. After a median follow-up of 2.3 years, carvedilol therapy was associated with a hazard ratio of 0.47 (95% CI 0.29-0.77)in patients with mild ascites and was not associated with increased mortality in patients with moderate to severe ascites[30]. Zacharias et al[34]recently conducted a Cochrane systematic review of 10 RCTs and 810 patients comparing the safety and efficacy of carvedilol versus traditional NSBBs in the primary and secondary prevention of variceal haemorrhage; they identified no differences in the incidence of mortality, variceal haemorrhage and serious adverse events between both groups despite greater reductions in HVPG for the carvedilol group. Due to the low quality of assessed evidence, these findings were associated with substantial uncertainty.
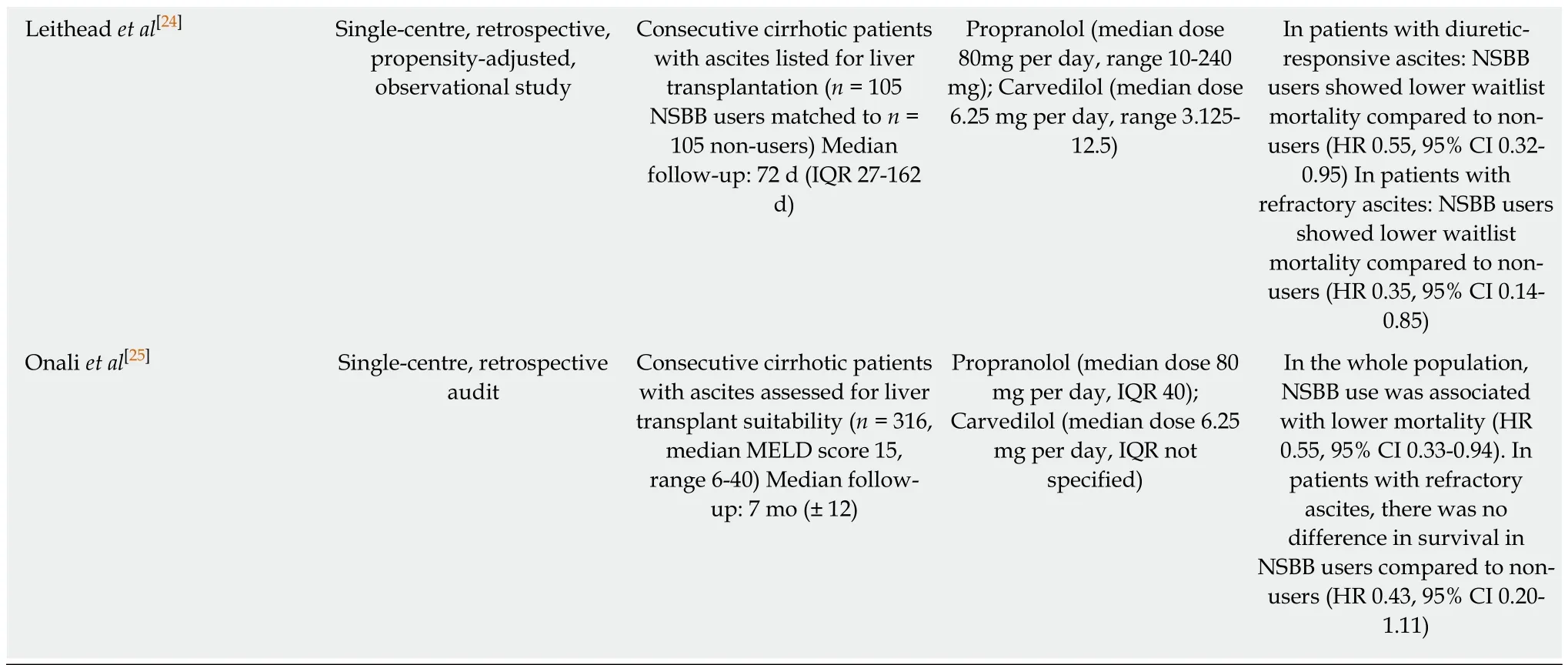
AKI: Acute kidney injury; CI: Confidence interval; HR: Hazard ratio; HRS: Hepatorenal syndrome; IQR: Interquartile range; IV: Intravenous; MELD: Model for end stage liver disease; NSBB: Non-selective beta-blocker; RCT: Randomised controlled trial; SBP: Spontaneous bacterial peritonitis.
Haemodynamically-independent potential of beta-blockers:Additional observational studies have proposed the existence of haemodynamically independent effects of beta-blockers. Senzolo et al[35]and Bang et al[15]observed protective effects of NSBB administration on SBP occurrence in patients with cirrhotic ascites. Similarly, Merli et al[36]prospectively followed 400 cirrhotic inpatients, finding that beta-blockade generally protected against infection and that infected patients showed lower morbidity and mortality when receiving beta-blocker therapy. Mookerjee et al[37]investigated the immunomodulatory effect of beta-blockers in 349 patients with acuteon-chronic liver failure (AoCLF) and observed that beta-blockade favourably affected 28-d mortality (24% vs 34%, P = 0.048). Patients on beta-blockers demonstrated reduced severity of AoCLF, slower progression of AoCLF and lower white blood cell counts on admission[37]. Facciorusso et al[38]analysed 107 cirrhotics admitted to a single centre with sepsis, noting that NSBB users had significantly reduced in-hospital mortality (18.7% vs 42.3%, P = 0.01), hospital stay duration (15.0 vs 18.5 d, P = 0.03),and white blood cell counts (9.2 vs 12.1, P = 0.004) compared to non-users.
A potential pathophysiological mechanism underlying these observations was provided by Reiberger et al[39]who measured reduced serum levels of interleukin 6 and lipopolysaccharide binding protein in cirrhotic patients receiving beta-blockers,indicative of decreased bacterial translocation. Bacterial translocation secondary to intestinal permeability and hypomotility is augmented in liver cirrhosis and appears to play a pivotal role in causing systemic immune dysfunction in these patients[21]. In animal models with ascites, cirrhotic rats were observed to have significantly reduced intestinal permeability as well as faster intestinal transit following propranolol administration[40]. Recently, Gimenez et al[41]observed that monocytes and granulocytes of cirrhotic patients on long-term NSBB therapy displayed significantly raised phagocytic capacity in the presence of bacterial DNA compared to NSBB-naïve patients.
Other potential effects of beta-blockers upon cirrhotic patients:To further investigate the haemodynamically independent effects of beta-blockade in patients with cirrhosis, Thiele et al[42]performed a meta-analysis of 23 RCTs on 2618 patients finding a reduced incidence of hepatocellular carcinoma (HCC) in patients receiving NSBBs [risk difference 0.026, 95% CI 0.052-0.001, number needed to treat (NNT) 38 patients]. Recently, Herrera et al[43]prospectively evaluated 173 patients included in the early HCC detection program for a median follow-up time of 11 years. The cumulative incidence of HCC was significantly lower in NSBB users compared to non-users (6% vs 19% at 10 years, 16% vs 24% at 15 years), with beta-blockade being the only parameter inversely correlated with HCC development on multivariate analysis. Regarding a pathophysiological mechanism underlying this finding, the authors propose that the reduction in bacterial translocation effected by betaadrenergic blockade may diminish the portal load of pathogen-associated molecular patterns and thus hepatic inflammation[44]. Secondly, beta-adrenergic blockade may impede angiogenesis through inhibition of vascular endothelial growth factor production. Both hepatic inflammation and neo-angiogenesis are critical drivers in the pathogenesis of HCC[44].
Clinical guidelines and future directions:Presently, the only effective surrogate marker for assessing response to beta-blocker administration is HVPG. HVPG reduction by 20% or to < 12 mmHg was demonstrated to significantly decrease the risk of variceal bleeding and improve survival[9,45], yet the clinical utility of HVPG testing is limited by its invasiveness and availability[32]. Clinical practitioners predominantly titrate beta-blockers to reach a specific target heart rate (50-55 beats per minute) despite insufficient evidence that reductions in heart rate correlate with reductions in HVPG[32]. It is imperative that future research focuses on the identification of novel, non-invasive biomarkers for the assessment of beta-blocker response, since it is critical to identify the change from benefit to detriment of betablocker treatment during the natural progression of cirrhosis, so that beta-blocker treatment can be individualised and patient benefit maximised.
While beta-blockers continue to occupy a pivotal role in the treatment of portal hypertension, recent evidence has not only outlined additional, haemodynamicallyindependent beneficial effects of beta-blockers in cirrhosis, but also described potentially debilitating effects in advanced cirrhotics. Concerning clinical practice,D’Amico et al[46]recommend that beta-blocker therapy should: (1) Not be used in compensated cirrhotics with no evidence of varices; (2) be used in cirrhotic patients with varices at risk of bleeding or re-bleeding independent of the absence/presence of ascites; and (3) be used with caution in cirrhotic patients with refractory ascites and discontinued if haemodynamic or renal compromise arises. Currently, the Braveno VI consensus and 2017 AASLD guidelines recommend temporarily reducing or withholding beta-blockers in patients with refractory ascites and circulatory dysfunction (serum sodium < 130 mEq/L, systolic BP < 90 mmHg)[5,47,48]. Similarly, the 2018 EASL guidelines recommend discontinuation of beta-blockers in patients who develop hypotension (systolic BP < 90 mmHg), sepsis, bleeding, AKI or SBP, followed by an attempt at re-introduction of beta-blocker therapy after recovery. Presently,EASL does not recommend the use of carvedilol[49].
Overall, the evidence-base for the use of NSBBs in cirrhotic patients remains disputed with the requirement for further assessment of safety and efficacy. A large body of evidence regarding the use of beta-blockers in advanced cirrhosis comes from observational studies which are at risk of indication bias as patients receiving betablockers are likely to have relatively severe liver disease with clinically significant portal hypertension and large varices[4]. This disparity in liver disease severity between patient cohorts is difficult to account for without randomisation[4].
Lactulose and rifaximin
Lactulose:From the 1980s onwards, non-absorbable disaccharides (lactulose and lactitol) have been the mainstay of treatment for HE and have been recommended as first line therapy ever since lactulose was shown to be equally as effective but safer than neomycin[50-52]. The adverse effect profile of non-absorbable disaccharides is wellcharacterised, and is predominantly characterised by non-serious gastrointestinal side effects such as bloating, flatulence and diarrhoea[52]. Lactulose exerts its main effect through reducing production of ammonia. Ammonia has been implicated in the pathogenesis of HE by causing direct neurotoxicity and astrocytic swelling. Lactulose is metabolised to lactic acid by colonic bacteria, resulting in intestinal acidification.The acidic environment both promotes the transfer of ammonia from tissues into the intestinal lumen and impedes the growth of ammoniagenic coliforms. Additionally,the cathartic effects of lactulose aid in decreasing intestinal bacterial load[53].
In 2004 a systematic review of 22 RCTs demonstrated that non-absorbable disaccharides had no significant effect on mortality or HE incidence after exclusion of trials with high risk of bias, and concluded that evidence to support the use of nonabsorbable disaccharides in the treatment of HE was insufficient[51]. As a consequence,further trials assessing the efficacy of lactulose in the management of HE were performed. A RCT of 140 patients by Sharma et al[54]investigating the efficacy of lactulose for secondary prophylaxis of HE found that, after 14-mo follow-up, a significantly lower proportion of patients receiving lactulose (19.6%) redeveloped HE compared to patients receiving placebo (46.8%, P = 0.001). Similarly, Agrawal et al[55]also investigated the efficacy of lactulose for secondary prevention of HE in a RCT (n= 235), finding that lactulose therapy was associated with significantly reduced HE recurrence compared to no intervention (26.2% vs 56.9%, P = 0.001). Another RCT by Sharma et al[56], this time investigating the efficacy of lactulose for primary prophylaxis of HE, found that, after 12-mo follow-up, a significantly lower proportion of patients receiving lactulose (11%) developed overt HE compared to patients receiving placebo(28%, P = 0.02). Furthermore, lactulose therapy was associated with improvement in both cognitive function and health-related quality of life in patients with minimal HE[57]. Mittal et al[58]then assessed the effectiveness of lactulose in the treatment of minimal HE in the RCT setting (n = 322), finding significant improvements in minimal HE in the lactulose group (47.5%) compared to the no intervention group (10%, P =0.006) as well as significant reductions in arterial ammonia levels (- 8.57 vs - 0.52, P =0.0001). Incorporating the new evidence generated after 2004, a recent Cochrane review including 38 RCTs and 1828 patients found moderate quality evidence for beneficial effects of non-absorbable disaccharides on mortality (RR 0.59, 95% CI 0.40-0.87), HE (RR 0.58, 95% CI 0.50-0.69), and other complications of cirrhosis such as liver failure, variceal haemorrhage and HRS (RR 0.47,95% CI 0.36-0.60), when compared to placebo or no intervention[52]. In view of the current evidence-base for non-absorbable disaccharides, EASL and AASLD recommend lactulose as the first-choice agent for the treatment of episodic overt HE and prevention of recurrent HE[59].
Rifaximin:As described above, the cathartic and ammonia-lowering effects of the non-absorbable disaccharide lactulose have been the cornerstone for treating acute,overt HE and maintaining remission in recurrent HE for decades[60,61]. However, its long-term therapeutic value has been limited as a consequence of treatment nonadherence due to its numerous, unpleasant side effects[62]. Lately, the semi-synthetic,non-absorbable antibiotic rifaximin surged in popularity as an alternative or additive to lactulose based on its gut-selective antimicrobial activity favouring non-pathogenic species and its favourable safety and tolerability profile[61]. A randomized, doubleblinded trial in 103 patients found the impact of rifaximin on the portosystemic encephalopathy index to be superior to the effect of lactitol[60,63]. A further placebocontrolled RCT by Bass et al[64]established the safety and efficacy of rifaximin therapy in the maintenance of remission in 299 patients with recurrent HE over a follow-up period of 6 mo, finding that a lower proportion of patients receiving rifaximin experienced an overt episode of HE (22.1%) and were hospitalised with HE (13.6%)compared to patients receiving placebo (45.9% and 22.6%, respectively)[60,64]. As a sequel to this trial, Mullen et al[62]performed an open-label, 24-mo maintenance study in 326 patients to investigate the long-term safety profile and treatment effect durability of rifaximin, finding that long-term rifaximin administration achieves a persistent reduction in HE-related and all-cause hospitalisation without a corresponding increase in infection or antibiotic resistance rates. A meta-analysis of 21 RCTs and 2258 patients demonstrated that rifaximin reduced mortality in overt HE,but not minimal HE, when compared to placebo, and had no effect on mortality when compared to non-absorbable disaccharides. In this study, rifaximin also decreased the risk of serious adverse events and had a potential beneficial effect on quality of life[65].However, the evidence analysed in this meta-analysis was of low-to-moderate quality[65]. Another meta-analysis by Wu et al[66]incorporating 8 RCTs outlined that there was no significant difference in the efficacy of preventing and treating HE between rifaximin and lactulose, but that rifaximin therapy was correlated with less adverse events. A recent retrospective analysis of 1042 patients with HE by Kang et al[67]correlated rifaximin-lactulose combination therapy with significantly improved mortality (HR 0.67, P = 0.024) and reduced risk of recurrent HE (HR 0.45, P < 0.001),variceal haemorrhage (HR 0.43, P = 0.011), and SBP (HR 0.21, P < 0.001), compared to lactulose alone. This was only evident in the non-HCC cohort (n = 421), however.Kabeshova et al[68]evaluated the cost-effectiveness of long-term rifaximin-lactulose combination therapy compared to lactulose monotherapy for recurrent HE in the French healthcare system. This study found that rifaximin-lactulose combination therapy incurs a cost of 18517 EUR (approximately 16000 GBP or 21000 USD) to gain one additional QALY compared to lactulose monotherapy, concluding that rifaximin is a cost-effective treatment in the context of the cost-effectiveness threshold range of 23000-34000 EUR (20000-30000 GBP) adopted by NICE. In view of the current evidence, EASL and AASLD state that rifaximin is effective as an add-on therapy to lactulose for secondary prevention of HE recurrence[59].
The potential uses of rifaximin beyond hepatic encephalopathy:Additionally,recent evidence has indicated that the therapeutic effects of rifaximin may extend beyond its original indication of treating HE. An initial, prospective, observational study conducted by Vlachogiannakos et al[69]observed reduced incidence of variceal haemorrhage, HE, SBP and HRS in 23 patients receiving rifaximin compared to controls. Similarly, Hanouneh et al[70]investigated 404 patients with cirrhotic ascites and demonstrated a 72% reduction in SBP incidence with rifaximin therapy compared to placebo. Norfloxacin is a systemic antibiotic, currently recommended as the first line agent in the prevention of SBP by both AASLD and EASL[71,72]. Recently, Praharaj et al[73]conducted a RCT (n = 117) comparing rifaximin and norfloxacin for both primary and secondary prevention of SBP. Praharaj et al[73]established that patients on norfloxacin had a significantly higher rate of SBP development compared to patients on rifaximin in secondary prophylaxis (39% vs 7%, P = 0.007), while no significant difference (20% vs 14%, P = 0.73) was manifested in primary prophylaxis. A metaanalysis performed by Sidhu et al[74]—incorporating three RCTs and one prospective observational study - compared norfloxacin and rifaximin with the primary outcome of SBP occurrence and secondary outcomes of mortality and adverse events. The included studies, of moderate quality evidence, either demonstrated superior efficacy of rifaximin or no significant difference between rifaximin and norfloxacin in SBP prevention, leading the authors to conclude that rifaximin could be a safe and efficacious alternative to norfloxacin in SBP prophylaxis for patients with hepatitis C virus (HCV) cirrhosis. Furthermore, a small prospective study in 13 patients with advanced cirrhosis suggests improvements in renal function after intestinal decontamination by rifaximin[75]. Baik et al[76]compared propranolol monotherapy to propranolol-rifaximin combination therapy in 65 patients with advanced cirrhosis,finding amplification of mean HVPG reduction with combination therapy. However,a recent RCT investigating the haemodynamic effect of rifaximin in 54 patients with cirrhotic ascites observed no difference in HVPG, cardiac output or glomerular filtration rate compared to placebo[77]. Due to its relative novelty, the evidence-base for the impact of rifaximin on outcomes in cirrhotic patients, particularly regarding its effects outside HE treatment, is lacking in robustness, with the majority of conducted studies featuring very limited sample sizes. A United Kingdom based, multicentre RCT evaluating the role of rifaximin in preventing secondary infections in cirrhotic patients, including both community and hospital acquired infections, is currently being undertaken and its results are awaited[78].
L-ornithine L-aspartate and acarbose:As outlined, ammonia has been identified as the pivotal neurotoxin implicated in the pathogenesis of HE and its reduction is a central objective in the therapeutic approach to HE management. LOLA has demonstrated ammonia-lowering properties by enhancing residual hepatic urea cycle activity and skeletal muscle glutamine synthesis[79,80]. Goh et al[79]performed a recent Cochrane systematic review of 36 RCTs and 2377 patients summarising the evidence of LOLA in the prevention and treatment of HE. The authors found very low quality evidence that LOLA had beneficial effects on mortality, HE and serious adverse events compared to placebo. However, these findings were not upheld when only trials with low risk of bias were considered. On subgroup analysis, there was no difference between intravenous and oral LOLA administration or between minimal and overt HE. In comparison to lactulose and rifaximin, LOLA demonstrated no effect on mortality, HE and serious adverse events. The uncertainty stemming from data quality concerns led the authors to conclude that new, high-quality RCTs are required for the definitive evaluation of evidence[79]. A randomised, placebo-controlled,quadruple blinded, phase IV trial investigating the efficacy of LOLA in treating overt HE is currently in progress and its results are awaited[81].
One randomised, double-blinded, placebo-controlled trial in 107 cirrhotic patients with HE and type 2 diabetes mellitus provided encouraging data for the safety and efficacy of acarbose in treating HE with the intervention group demonstrating lower blood ammonia levels, improved encephalopathy global score and reduced Child-Pugh score[82]. However, the generalisability of these findings is diminished by the highly selective study population of compensated Child-Pugh A cirrhotics with predominantly Grade 2 encephalopathy, as well as the scarcity of further studies investigating the efficacy of acarbose in treating HE[83]. Acarbose is not mentioned in current EASL and AASLD guidelines for HE management.
Diuretics
The most common complication of cirrhosis is ascites[84]. Diuretics are the mainstay of treatment for moderate ascites (Grade 2)[72,85]. Excessive aldosterone generation secondary to splanchnic vasodilatation and systemic hypotension is considered the primary causative factor for increased sodium reabsorption in the kidneys of patients with cirrhotic ascites[86]. Consequently, spironolactone monotherapy was shown superior to loop diuretics for initial ascites management, with furosemide frequently used as an addition to potentiate diuresis in recurrent ascites[72]. Side-effects may result from excessive diuresis causing hypovolaemia and renal dysfunction along with electrolyte disturbances such as hyponatraemia, hypokalaemia and hyperkalaemia[72,87,88]. Furthermore, diuretic therapy may precipitate HE; although the underlying mechanism remains unknown[72,89,90], this is likely related to a combination of electrolyte disturbance and hypovolaemia. To forestall these adverse effects, it is recommended to adjust diuretic dosage so that daily weight loss does not exceed 800 g[91]. In cirrhotic patients who develop ascites, one-year survival ranges from 60 to 85%[92]. Sodium restriction and diuretic therapy enable mobilisation of ascites in approximately 90% of those patients.
α-1 and α-2 adrenergic agonists:One-year survival substantially declines to 25% with the development of refractory ascites (diuretic-resistant or diuretic-intractable), when ascites mobilisation fails due to a lack of effect or advent of complications such as SBP,hyponatraemia and renal impairment[84,93]. First-line management for refractory ascites is serial large-volume paracentesis[49]. However, recent evidence has proposed a role for α1 and α2-adrenergic agonists in managing refractory ascites. A group of heterogenous studies with differing dosing and follow-up regimes demonstrated that midodrine, a peripheral α1-adrenergic agonist acting as a splanchnic vasoconstrictor,increases mean arterial pressure, urine output as well as urine sodium output, and decreases plasma renin and aldosterone activity in patients with refractory ascites[84].Two small randomised pilot studies found that midodrine plus standard medical therapy transiently (3 mo) improves the mobilisation of refractory ascites compared to diuretic therapy alone[94,95]. Guo et al[96]performed a meta-analysis of 10 RCTs (n = 462)finding that midodrine enhances response rates to diuretics, but does not increase survival in patients with refractory ascites. A recent small-scale prospective observational study also suggests that oral midodrine and subcutaneous octreotide combination therapy could ameliorate cirrhosis-induced hyponatraemia (pretreatment serum Na: 124 mmol/L vs post-treatment serum Na: 130 mmol/L, P =0.00001)[97]. AASLD advise to consider the administration of midodrine in patients with refractory ascites, while EASL have not recommended its use in view of limited sample size of existing trials[49,71]. Clonidine, a central α2-adrenergic agonist with sympatholytic activity, is thought to ameliorate sympathetic nervous system overstimulation which leads to renal hypoperfusion and excessive renin-angiotensin system activation in refractory ascites[84,98]. Similar to midodrine, clonidine has been shown to improve urine output and urine sodium output, while lowering plasma aldosterone and renin activity in patients with refractory ascites. Multiple small-scale RCTs with limited follow-up investigated the clinical efficacy of clonidine in such patients, demonstrating that clonidine reduced diuretic requirements and induced earlier diuretic response[94,98]. In animal models of cirrhosis, clonidine improved renal function at low doses, but negatively influenced mean arterial pressure and urine sodium output at high doses[99]. Clonidine is currently not recommended by AASLD or EASL as an adjunct to diuretics in refractory ascites management due to the nonexistence of sufficiently powered, long-term studies[49,71].
Vaptans:To avoid the increased incidence of adverse effects with high-dose conventional diuretic therapy, the so-called vaptans, selective antagonists to the vasopressin V2 receptors in principal cells of collecting ducts, have gained interest in recent decades as they are able to achieve a highly hypotonic diuresis without impacting on the electrolyte balance[100]. Thus vaptans might be valuable in the correction of hyponatraemia, an important predictor of mortality in cirrhotic patients with ascites. However, controversies exist with regards to their expense and their effect on clinically relevant outcomes and prognosis in patients with cirrhosis[100]. In their meta-analysis (16 RCTs, n = 2620) Yan et al[100]found that vaptans showed a significant aquaretic effect and increased serum sodium significantly both when used alone and when used in combination with traditional diuretics, and concluded that vaptans could play a major role in the pharmacological treatment of refractory ascites with insufficient response to traditional diuretics in order to alleviate ascites volume and the need for paracentesis without incurring a higher rate of adverse events. Yet,despite the substantial beneficial impact of vaptans on diuresis and hyponatraemia,vaptan therapy made no significant difference to short-term or long-term survival in these cirrhotic patients. An adverse effect of vaptan treatment observed in the included trials was excessive correction of serum sodium, which may lead to osmotic demyelination, thus necessitating monitoring when administering vaptans[100].Furthermore, the Food and Drug Administration has recommended to avoid the use of vaptans in patients with chronic liver disease, as tolvaptan has the potential to induce serious liver injury[101]. In a phase 3, placebo-controlled, randomized trial (n =1200), satavaptan therapy showed no difference to placebo regarding ascites control,but was superior to placebo in improving serum sodium of hyponatraemic patients.However, in one of the trial groups, satavaptan therapy was associated with increased mortality (HR 1.47; 95% CI 1.01-2.15). No specific causes for this mortality increase were identified, but the majority of deaths were attributed to known complications of cirrhosis. The authors concluded that vaptan therapy is ineffective in controlling ascites, but may have a role in managing hypervolaemic hyponatraemia in cirrhotic patients[102]. Current EASL and AASLD guidelines do not endorse the use of vaptans in cirrhotic patients in light of their costs, risks and lacking efficacy in clinical settings[49,71].
Statins
Although statins are the mainstay for preventing atherosclerosis and have welldefined beneficial effects on cardiovascular health, they are under-prescribed in cirrhotic patients due to concerns over hepatotoxicity[103]. However, recent evidence points towards an unexpected, potentially beneficial impact of statins on cirrhosis resulting from their pleiotropic properties which comprise antioxidant, anti-fibrotic,anti-infective and anti-inflammatory effects[103,104]. Endothelial dysfunction and diminished nitric oxide generation play essential roles in the establishment of the proinflammatory and pro-fibrotic microenvironment of cirrhosis[104]. Numerous preclinical studies in vitro and in vivo have demonstrated that statins upregulate Kruppellike factor 2 and nitric oxide (NO) availability as well as down-regulate hepatic stellate cell activation, thus exerting favourable effects on fibrogenesis, endothelial function and portal hypertension[103]. In addition to findings from pre-clinical studies,simvastatin enhanced hepatosplanchnic NO output and reduced intrahepatic vascular resistance in a study involving 30 cirrhotic patients[105]. A multicentre RCT conducted by Abraldes et al[106]in 59 cirrhotic patients with portal hypertension described that simvastatin significantly decreased HVPG by 8.3% and improved hepatocyte perfusion without discernible harmful effects on the systemic circulation[103,104,106].
In a retrospective study of patients with predominantly Child-Pugh A cirrhosis (81 statin users and 162 controls), statin use was associated with lower mortality (HR 0.56) and decompensation (HR 0.55) risk on multivariate analysis after 36-mo followup[107]. Similarly, another recent retrospective analysis of patients with compensated HCV cirrhosis (685 statin users and 2062 controls) also described statin use to be associated with lower mortality (HR 0.56) and decompensation rates (HR 0.55) at 10-year follow-up after adjusting for age, serum albumin, model for end stage liver disease (MELD) and Child-Pugh scores[108]. Using the Taiwanese National Health Insurance database, Chang et al[109]conducted a nested case-control study with 13-year follow-up, matching 675 statin users with 675 statin non-users. Following a doseresponse relationship, statin use correlated with a significantly decreased risk of decompensation (HR 0.39), HCC development (HR 0.52), and mortality (HR 0.46). The most robust evidence regarding the therapeutic benefit of statins in cirrhosis comes from a multicentre RCT of 158 cirrhotic patients who received either standard therapy(beta-blocker and band ligation) after variceal haemorrhage, or standard therapy plus simvastatin. After 24-mo follow-up, addition of simvastatin had no effect on the rate of re-bleeding but significantly reduced all-cause mortality compared to the control group (9% vs 22%, P = 0.03). However, this survival benefit was only observed in the Child-Pugh A/B cohort, not in Child-Pugh C patients, and no difference was found in the rate of cirrhosis-related complications between the intervention and control groups. Notably, two patients with decompensated cirrhosis developed rhabdomyolysis, thus again raising questions about the safety of statin use in advanced cirrhosis[103,104,110].
Recently, the evidence regarding the impact of statin use on cirrhosis and its complications was summarized by three meta-analyses. Kamal et al[111]performed one meta-analysis of 9 studies (2 RCTs, 7 observational studies) and 166000 patients (40950 statin users) finding moderate-quality evidence that statin use is associated with reduced fibrosis progression (HR 0.55, 95% CI 0.49-0.61) and rate of decompensation(HR 0.54, 95% CI 0.46-0.65) as well as low-quality evidence that statin use is associated with reduced mortality (0.62, 95% CI 0.43-0.91). The second meta-analysis by Kim et al[112]included 121000 patients (46% statin users) and found moderate-quality evidence of an association between statin use and decreased risk of decompensation (RR 0.54,95% CI 0.47-0.61), mortality (RR 0.54, 95% CI 0.47-0.61) and variceal bleeding (RR 0.73,95% CI 0.59-0.91). Thirdly, Singh et al[113]performed a large meta-analysis including 1.4 million patients with 4298 cases of HCC, associating statin use with a 37% risk reduction [odds ratio (OR) 0.63, 95% CI 0.52-0.76] of HCC development. This risk reduction was significantly more pronounced in the Asian population, in which chronic hepatitis B virus infection is the predominant risk factor for HCC development. In this population, the NNT to prevent one case of HCC per year was estimated at 5209. As a consequence of this high NNT in combination with the significant heterogeneity between included studies, the authors conclude that they cannot recommend statins for chemoprevention of HCC[103,113]. In the context of increasingly stretched healthcare budgets, the inexpensiveness of statins and the encouraging evidence presented above calls for the implementation of a phase 3 RCT in patients with Child-Pugh A/B cirrhosis with the primary endpoint of decompensation or death[114].
While the use of statins in cirrhotic patients remains disputed due to safety concerns, multiple studies have demonstrated that statins are safe to use in patients with compensated non-alcoholic fatty liver disease (NAFLD) irrespective of liver enzyme elevations[115,116]. Due to the strong association between NAFLD and cardiovascular morbidity and mortality, both EASL and AASLD guidelines recommend the initiation of cholesterol-lowering therapy with statins in patients with compensated NAFLD[117,118]. However, current AASLD guidelines advise against the use of statins in patients with decompensated cirrhosis in view of the potentially deleterious complications in this population of patients[117]. Since the majority of evidence regarding the pleiotropic effects of statins in chronic liver disease is derived from observational studies and small-scale trials, adequately powered RCTs are required to assess whether the pleiotropic properties of statins can modulate clinical endpoints in cirrhotic patients[119].
Proton pump inhibitors
Despite suboptimal evidence for their efficacy in cirrhosis and growing concerns over their promotion of bacterial overgrowth and translocation, proton pump inhibitors(PPI) are frequently prescribed to patients with cirrhosis receiving multidrug treatment for variceal haemorrhage or portal hypertensive gastropathy in order to forestall peptic complications[120]. In fact, 46%-78% of cirrhotic patients are reported to use PPIs[121]. Initially, concerns about the safety of PPI use in cirrhosis were raised by a variety of low-powered observational studies. A prospective study of 272 patients with overall survival as the primary endpoint demonstrated that PPI treatment was associated with higher MELD scores, ascites and mortality[122]. In addition, a metaanalysis of four studies and 772 patients identified a significant correlation between PPI use and SBP development (OR 2.77)[123]. A prospective cohort study of 400 patients hospitalized with cirrhosis established that PPI use was an independent risk factor for the development of infection (OR 2.0), while beta-blocker use was a protective factor(OR 0.46)[36].
Recently, two large, retrospective analyses fuelled the established fear over the impact of PPI use on SBP and HE development. Dam et al[121]retrospectively analysed data from three large, multicentre RCTs (n = 865) for the use of satavaptan in cirrhotic ascites, describing that current PPI use was associated with an increased risk of HE(HR 1.36, 95% CI 1.01-1.84) and SBP development (HR 1.72, 95% CI 1.10-2.69)compared to non-users. Additionally, the authors described that only 56% of PPI users had a valid indication for PPI prescription[121,124]. Using data from the Taiwan National Health Insurance database, Tsai et al[125]conducted a nested case-control study of 1166 cirrhotic patients with HE matched to 1166 cirrhotic patients without HE, observing a dose-response relationship between PPI use and risk of HE development. The pathophysiological mechanism hypothesized to underlie this observed association between PPI use and SBP/HE development is based on PPIs weakening the stomach acid barrier by increasing gastric pH, thus promoting bacterial dysbiosis, translocation and small intestinal bacterial overgrowth(SIBO)[121,124]. Since the majority of hepatic blood supply is derived from the gut, there is an intimate relationship between the liver and the intestinal microbiome. Gut dysbiosis with consequent translocation of pathogenic bacterial taxa and endotoxins into the portal and systemic circulation promotes immune system dysfunction as well as hepatic inflammation and injury[126]. In line with this hypothesis, Bajaj et al[127]recently conducted a cohort study, observing the readmission rates in 343 cirrhotic inpatients and conducting stool microbiota analyses in 137 cirrhotic outpatients. In the inpatient cohort, PPI use was independently associated with higher readmission rates,while in the outpatient cohort, the microbiota composition of PPI users showed increased oral-origin taxa and decreased beneficial autochthonous taxa. In contrast, a large (n = 1191), retrospective analysis by Ratuapli et al[128]described no significant difference in the frequency of SIBO diagnosis, as established by glucose hydrogen breath testing, between PPI users and non-users. Alternatively, Assaraf et al[129]hypothesise that PPI use and HE development may be linked to a cerebral build-up of toxic metabolites as PPIs act as agonists to ATP-binding cassette efflux transporters found on the blood-brain barrier.
However, this negative trend for PPI use in cirrhosis has recently come under question. Khan and colleagues published two articles highlighting the limitations of the retrospective analyses by Dam et al[121]and Tsai et al[125]. In both studies, the ORs achieved were below 3, an indication that the observed associations may be due to residual confounding rather than causality[124,130]. In the Tsai study, patients receiving PPIs had higher rates of comorbidities, thus representing a potential source of channelling bias[130]. The Dam study analysed data not collected specifically for the purpose of assessing the impact of PPIs on SBP and HE incidence and could thus not account for all potential confounders[121]. Therefore, Khan et al[124,130]concluded that the current evidence-base against PPIs is not of sufficient quality to withhold PPIs from cirrhotic patients with a reasonable indication for PPI treatment. A large (n = 519),prospective, multicentre study by Terg et al[131]observed no significant difference in PPI use between infected and non-infected patients (44.3% vs 42.8%) or between patients with SBP and patients with ascites and no SBP (46% vs 42%). Furthermore, no difference was observed in the causative species or infection origin between PPI users and non-users who developed SBP[131]. The largest meta-analysis (16 studies, 10 casecontrol/6 cohort, n = 8145) on this issue by Yu et al[132]found that the harmful association between PPI use and SBP incidence was present in case-control studies,but not cohort studies, and that there was no association between PPI use and mortality during hospitalisation in both case-control and cohort studies. The authors therefore concluded that causality between PPI administration and increased SBP incidence and mortality could not be established[132]. In view of the conflicting evidence and substantial limitations of the conducted studies outlined above, there is the need for a randomized, placebo-controlled, adequately powered trial investigating the effects of long-term PPI administration in cirrhotic patients with the primary outcomes of HE and SBP occurrence.
Anticoagulation
Historically, cirrhotic patients were viewed as ‘auto-anticoagulated’, since cirrhosis is associated with a global impairment in clotting factor synthesis excluding factor VII and von Willebrand factor. More recently, it has been recognized that the relationship between cirrhosis and the coagulation cascade is more complex and that routine haemostatic tests, such as the international normalized ratio or activated partial thromboplastin time, lack accuracy in predicting coagulation status in these patients.In light of a coexisting reduction in anticoagulant factors (namely antithrombin III,protein S and C), recent studies have highlighted the importance of procoagulant complications in cirrhotic patients, with higher rates of venous thromboembolism(VTE) and splanchnic vein thrombosis being observed. These findings have suggested the potential role for anticoagulation in cirrhosis. Furthermore, there is emerging evidence that coagulation proteins may activate hepatic myofibroblasts to accelerate fibrogenesis. As such, there has been the suggestion that anticoagulant medication may thus have a further role in impeding fibrosis progression[133-135].
Retrospective studies investigating the role of prophylactic anticoagulation in cirrhotic patients at risk of VTE have provided heterogenous results with some studies failing to demonstrate a reduction in VTE incidence with anticoagulative treatment[133,136]. In a single-centre, non-blinded RCT of 70 cirrhotic outpatients, Villa et al[137]investigated the safety and efficacy of low-molecular-weight heparin in preventing portal vein thrombosis (PVT). The major findings were that subcutaneous enoxaparin not only reduced PVT incidence (0% vs 27.7%, P = 0.001) but also protected against hepatic decompensation (11.7% vs 59.4%, P < 0.001) with no apparent increase in haemorrhagic complications. The authors attribute the observed reduction in decompensating events to improvements in hepatic microcirculation with consequent diminution of bacterial translocation and immune dysfunction[134,137].Further prospective and randomised studies are required to delineate the role of prophylactic anticoagulation in cirrhosis.
Regarding patients with established non-malignant PVT, numerous studies have demonstrated a favourable effect of low-molecular weight heparin therapy on portal vein recanalization rates, achieving re-permeation in 40%-90% of treated patients compared to 0% of untreated controls. Early initiation of anticoagulative therapy was the most important factor associated with successful re-permeation. Furthermore,these studies indicate that anticoagulation therapy has an acceptable safety profile in cirrhotic patients with no significant increase in bleeding rates provided that oesophageal varices are adequately screened for and managed[134,138-141]. At present,however, there is a need for detailed guidelines regarding the use of anticoagulation therapy in patients with cirrhosis.
Further treatments
A number of different agents with potentially therapeutic effects upon patients with cirrhosis are currently at different stages of pre-clinical and clinical assessment. These are summarised in Table 2.

Table 2 Summary of further pharmacological agents with potentially therapeutic effects
CONCLUSION
The evidence presented above clearly demonstrates that, while pharmacotherapy plays an important role for the long-term supportive management of the cirrhotic outpatient, its application is also highly complex and controversial. Many questions regarding the effect of the individual agents in the different stages of cirrhosis remain unanswered and require further research, particularly in a randomized, controlled setting with well-defined cohorts of cirrhotic patients. In this article we have provided an update with regards to the latest studies and international consensus on specific treatments. To maximize benefits and minimize drawbacks of chronic pharmacotherapy in cirrhosis, it is essential that these drugs are prescribed and administered only in close accordance with up-to-date guidelines and that patients are reviewed frequently, so that adverse effects can be recognized early. To heighten the effectiveness of pharmacotherapy in cirrhosis, drug administration needs to be individualized with respect to the following criteria: current complications of cirrhosis, stage of cirrhosis, type of drug used (especially for beta-blockers) and dose of drug used. Pharmacotherapy is only one part of the holistic management of the cirrhotic outpatient and will only achieve its full effectiveness if used in conjunction with treatment of the underlying aetiology of liver disease, nutritional management and patient education in a specialist clinic setting.
杂志排行
World Journal of Gastroenterology的其它文章
- Outcomes of per oral endoscopic pyloromyotomy in gastroparesis worldwide
- Dbx2 exhibits a tumor-promoting function in hepatocellular carcinoma cell lines via regulating Shh-Gli1 signaling
- Dynamic changes of key metabolites during liver fibrosis in rats
- Procyanidin B2 protects against diet-induced obesity and nonalcoholic fatty liver disease via the modulation of the gut microbiota in rabbits
- Triggers of histologically suspected drug-induced colitis
- Women on the liver transplantation waitlist are at increased risk of hospitalization compared to men