Clinicaleffectsofphototherapycombinedwithalbuminadministrationonhyperbilirubinemiainnewborns
2018-05-03,,,U,
, , , U,
(DepartmentofNeonatology, AffiliatedHospitalofGuilinMedicalUniversity, Guilin, Guangxi, 541001)
CLC: R 722.17DocumentCode: APaperNumber: 2096-0867(2018)03-0001-05
Introduction
Neonatal hyperbilirubinemia is a universal problem in newborn nurseries. It is mainly caused by excessive accumulation or metabolic disturbance of bilirubin[1]. If neglected or untreated, the unconjugated hyperbilirubinemia carries the risk of neurotoxicity, leading to vital neurodevelopmental consequences for the newborns[2]. This kind neurotoxicity is related to the increased passage of free bilirubin, the fraction of bilirubin that is not bound to plasma proteins, into the brain[3]. The most widely used method of reducing bilirubin level is the phototherapy[4]. However, the combined usage of phototherapy and albumin administration remained controversial. This study showed its originality with taking the newborns’ body weight and the amount of milk intake as observational indicators, exploring more evidences of clinical effects on neonates undergoing phototherapy combined with albumin administration.
Methods
Studydesignandsetting
This study was a prospective randomized controlled clinical trial conducted in a tertiary neonatal intensive care unit in China.
Sampleselection
In total, sixty-eight newborn infants who were hospitalized at affiliated hospital of Guilin medical university were selected as subjects of this study. All subjects aged 1-28 d, average 6.87 d. The ratio of boy to girl is 1.03∶1. Inclusive criterion: (1) Infants with clinically significant hyperbiliribunemia (total serum bilirubin, TSB>12.9 mg/dL) requiring phototherapy. (2) Infants without the administration of immunoglobulin intravenously. (3) Infants without the implementation of exchange transfusion. (4) Infants without neonatal hepatitis or biliary obstruction.
Procedures
Groupandobservationalindicators: All selected infants were randomly divided into the study group and the control group according the order of admission, with 32 cases in each group. Newborns in control group were treated with conventional treatment (phototherapy and fluid replacement). Those in the study group received albumin administration apart from conventional treatment. The differences on TSB, the amount of milk intake and body weight were compared between two groups before and at 1, 2 and 3 days after phototherapy.
Phototherapyandalbuminadministration: All infants were exposed to intermittent phototherapy with the same device (Daiwei Double-sided Blue-ray box, Ningbo).They were unclothed except for their eyes and genital region. The time for phototherapy was 8-10 h per day, 3 days in total. The phototherapy was stopped once the TSB level below 12.9 mg/dL or bronze baby syndrome occurred. Infants were carefully monitored for possible side effects of phototherapy, including dehydration, hypothermia, hyperthermia, skin rash and diarrhea. The administration of albumin was started in the first day of phototherapy. The usage of albumin was based on the body weight about 1g per Kg, dissolving the drug in 5% glucose solution of 20 mL through intravenous drip within 4 hours.
Bloodsamples: Venous blood sampling was performed at 8 am from a peripheral vein (heel)prior to phototherapy and within the first three days after phototherapy. Serum bilirubin levels were measured immediately by trained medical staffs. The bilirubinometer was DH-100 produced by APEL corp. in Shanghai.
Assessmentofmilkintakeandbodyweight: Electronic scale (DY-1, Shizheng Medical instrument co. LTD, Shanghai) was used to weigh newborns at 8 am each day after bathing. The quantities of milk intake for each newborn were recorded in the sheets by nursing staff.
Statisticalanalysis
IBM SPSS Statistics 20.0 (software) was used for statistic analysis in the study. A repetitive measurement and analysis of variance of variance (ANOVA) was performed on the TSB value, body weight and milk intake at different time after intervention.
Results
TSBvalue
There was no significant difference of TSB level between two groups at different time points after phototherapy(F=3.578,P>0.05). In both two groups, the level of TSB was decreased after phototherapy compared with that before phototherapy(F=286.640,P<0.05). Interaction effect was presented between albumin administration and time(F=9.866,P<0.05). Laboratory data are listed in Table 1.

Table 1. ThevariationofTSBvaluebetweentwogroupsbeforeandafterphototherapy (μmol/L)
Bodyweight
There was no significant difference in body weight between two groups before and at different time points after phototherapy (F=1.222,P>0.05). However, the body weight was increased at different time point after phototherapy compared with that before phototherapy (F=5.205,P<0.05). Interaction effect was present between albumin administration and time(F=2.731,P<0.05).Laboratory data are listed in Table 2.
Milkintake
There were significant differences in amount of milk intake between two groups before and at different time points after phototherapy (F=7.808,P<0.05). The amount of milk intake was increased at different time point after phototherapy compared with that before phototherapy(F=83.974,P<0.05). Interaction effect was present between albumin administration and time(F=3.644,P<0.05). Laboratory data are listed in Table 3.

Table 2. Thevariationofbodyweightbetweentwogroupsbeforeandafterphototherapy (Kg)
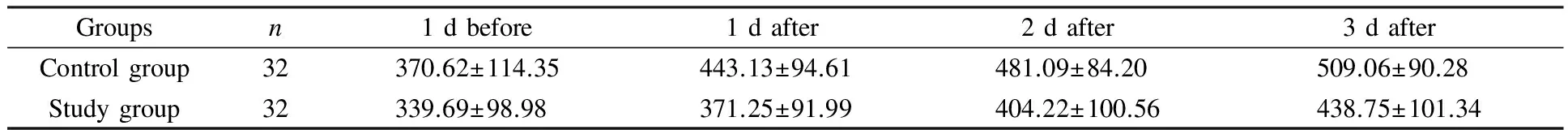
Table 3. Thevariationofmilkintakebetweentwogroupsbeforeandafterphototherapy (mL)
Discussion
The incidence of neonatal hperbilirubinemia has been increasing in recent years[5]. At present, phototherapy for neonatal hyperbilirubinemia was commonly used in clinical practice. The phototherapy uses light energy to change the molecular conformation of bilirubin, therefore, the reaction and excretion of bilirubin photoisomers of was proved to be the main mechanism for the decrease in serum bilirubin during phototherapy for neonatal hyperbilirubinemia[6]. Albumin is a carrier of bilirubin which can combine with the unconjugated bilirubin, therefore promoting its excretion.
A recent study showed that the combined use of albumin and phototherapy could lower the levels of TSB, help the recovery of newborns with neonatal hyperbilirubinemia[7]. Meanwhile, other researches held suspicious opinions to its use in clinical practice. It might cause the redistribution of bilirubin, and affecting the treatment effect of phototherapy by transporting the bilirubin into blood vessels[8]. Some studies also indicated that human serum albumin (HSA) administration was suggested to increase plasma bilirubin-binding capacity. However, its clinical use is infrequent due to difficulties to address its potential preventive and curative benefits, and to the absence of reliable markers to monitor bilirubin neurotoxicity risk[9]
In this study, we showed that the appetite of neonates was greatly improved as the result of the combination application of albumin administration and phototherapy. It may caused by the synergistic effect of albumin to phototherapy. Although there was no obvious evidence about its influences on TSB and the growth of neonates’ body weight, the interaction effects between album administration and time were revealed. It means that the differences may become obvious as time goes on. Longer observation period is needed to provide further description about their combined effect.
[1] BHUTANI V K, ZIPURSKY A, BLENCOWE H, et al. Neonatal hyperbilirubinemia and Rhesus disease of the newborn: incidence and impairment estimates for 2010 at regional and global levels[J]. Pediatr Res, 2013, 74(Suppl 1): 86-100.
[2] GAMALELDIN R, ISKANDER I, SEOUD I, et al. Risk Factors for Neurotoxicity in Newborns With Severe Neonatal Hyperbilirubinemia[J]. Pediatrics, 2011, 128(4): 925-931.
[3] CUPERUS F J C, SCHREUDER A B, IMHOFF D E V, et al. Beyond plasma bilirubin: The effects of phototherapy and albumin on brain bilirubin levels in Gunn rats[J]. J. Hepatol, 2013, 58(1): 134-140.
[4] MREIHIL K, STENSVOLD H J, NAKSTAD B, et al. Phototherapy is commonly used for neonatal jaundice but greater control is needed to avoid toxicity in the most vulnerable infants[J]. Acta Paediatr, 2018: 107(4): 611-619.
[5] GAO Y, XU Y Y, LI L S. Effects of Hyperbilirubinemia newborns undergoing phototherapy by integrated water therapy and touching [J]. J Prac Med, 2012, 28(4): 624-625.
[6] ITOH S, OKADA H, KUBOI T, et al. Phototherapy for neonatal hyperbilirubinemia[J]. Pediatr Int, 2017, 59(9): 959-966.
[7] LI W W, NAI Y, FENG S F, et al Anlysis of combined treatment effects of albumin and phototherapy to neonatal jaundice neonate [J]. J Clin Med Prac, 2017, 21(1): 94-95.
[8] CHEN W C, LIU G S, Effects of simple phototherapy or phototherapy combined with albumin therapy on severe jaundice in full-term neonates[J]. Chinese J Pathophysiol, 2015, 31(5): 943-946.
[9] VODRET S, BORTOLUSSI G, SCHREUDER A B, et al. Albumin administration prevents neurological damage and death in a mouse model of severe neonatal hyperbilirubinemia[J]. Sci Rep, 2015, 5: 16203.