Factitious disorder - A rare cause for unexplained epistaxis
2017-11-29SoumitraDASShabnaMOHAMMEDNimishaDOVALArjunKARTHA
Soumitra DAS*, Shabna MOHAMMED, Nimisha DOVAL, Arjun KARTHA
•Case report•
Factitious disorder - A rare cause for unexplained epistaxis
Soumitra DAS1,*, Shabna MOHAMMED2, Nimisha DOVAL3, Arjun KARTHA1
Psychogenic, epistaxis, factitious, stress
1. Introduction
Factitious disorder is the intentional production of symptoms- physiological or psychological, to simulate an illness.[1]Epistaxis is common enough to be found in 60%of the population and is usually minor and self-limited or may require only local compressive techniques. In rare cases, however, it may be severe enough to cause massive bleeding and even death.[2]Epistaxis can be both anterior and posterior, though anterior is more common, the keisselbach’s plexus being most commonly implicated.It can be caused by both local and systemic processes.Epistaxis not controlled by compression is treated by local vasoconstrictive agents, packing, arterial ligation,and embolization.[3]
Psychogenic recurrent bruising, localised spontaneous ecchymosis, menorrhagia, and haematuria have been mentioned in literature.[4]Factitious disorder is often difficult to distinguish from genuine illnesses and malingering. Malingering is the deliberate production of symptoms for external gain, such as to obtain housing or financial aid or to avoid being drafted[1]. Also noteworthy is the fact that factitious disorder is in itself not a uniform entity. The DSM 5 requires that the symptoms be simulated in order to gain medical attention and partake in the hospital system, whereas the ICD 10 does not insist on this criterion.[1,5]Here, we report a case of factitious disorder which presented with recurrent nasal bleeding where surgical specialists were unable to find any underlying cause.
2. Case Report
An 18 year old girl with no past or family history of psychiatric illness as well as a bleeding disorder,presented to the surgical emergency department with abrupt onset bleeding from the nose. She was admitted to the department of otorhinolaryngology and evaluated for bleeding disorders like factor VIII deficiency and platelet abnormality and underwent neurological imaging and abdominal ultrasonography but investigations were non-contributory.Investigations like total count, differential count, renal function test, liver function test, thyroid function test,and electrolytes were within normal limits. Epilepsy was ruled out in consultation with the department of neurology. In view of non-response to medication, the patient was sent to the psychiatric out patient service for a consultation. Patient’s BMI was 25. Vitals were stable with vesicular breathing sounds and normal S1 S2 heart sounds. There were no organomegaly and tenderness over abdomen. Central nervous system and peripheral nervous system parameters were within normal limits. For genital examination, gynaecological consultation was asked for. A gynaecology consultation revealed that she had multiple cut marks over the unexposed areas of her body. Injury report was prepared that showed 1cm by 5cm cuts marks over her thigh and upper leg mostly in the medial region. All cuts were superficial skin cuts. Most of them were dry and few were recent like near to the upper thigh. She denied any physical or sexual abuse. On instruction from us, the mother kept an eye on the patient unobserved and discovered the patient injuring herself with sharp objects in unexposed areas and mixing it with her nasal secretions to simulate epistaxis.
After a detailed evaluation, the patient revealed that she was undergoing significant ongoing stress due to parental conflict. Since her childhood she has been exposed to severe mental turmoil due to the unhealthy relationship between her parents. Though there was no growth restriction to her social, motor and language milestones, she had developed very poor attachment behavior towards parents and friends. She also mentioned a lack of confidence about decision making and asking validation in everything she had to take part which exposed her dependent personality traits.
Although a high achieving student, her grades had recently been slipping. She claimed to be unable to recall what had happened during the periods of epistaxis. After mental status examination and suggestion, she revealed that she had been having low mood and loss of interest in academics but denied suicidal ideation and vegetative dysfunction. She did not have any intention to obtain medical attention. Her main motive seemed to be to get attention from her parents.
She was started on fluoxetine and cognitive behavioral therapy and then we persuaded the family to attend family therapy to resolve the parental conflict. She was followed up for 1 year with monthly telephonic consultation and three monthly outpatient visits. Since the last consultation, she was doing well with excellent academic achievements. Fluoxetine was tapered and stopped after 9 months of therapy. Positive reappraisal, seeking social support and problem solving strategies were taught and mindfulness techniques were demonstrated to her.
3. Discussion
Factitious disorder is often misdiagnosed leading to unnecessary medications and expensive examinations.Subconscious or unconscious conflicts are played out in the patients behaviour. Circumscribed amnesia and complex acting out of internal conflicts have been mentioned in the literature but are often not diagnosed due to poor knowledge about its varied presentations.Factitious disorder is more common among girls than boys (1.8-3:1).
The factitious disorder can be presented with haematuria, haemoptysis, vomiting and hypoglycaemia.It is differentiated from malingering by the absence of external gain or rejection of treatment or invasive procedures. According to DSM 5, it is characterised by falsification of physical or psychological signs and symptoms with individual presentation such as illness or impairment which could not be explained by any other mental or physical disorders. Also, it gives value to the absence of external rewards rather than internal motivation. Factitious disorder by proxy is another diagnosis where the caregiver is responsible rather than the patient himself or herself.[5,6]
An unconscious motivation comes from childhood trauma or deprivation where the child gradually assumes suffering or illness as the sole meaning of life.When he or she receives attention from a physician it is thought of as a vehicle for relief. Eventually, the sick role gives the patient comfort and relief from trauma.[7]The following flowchart can explain the psychoanalytic underpinnings of the disorder:
In this case, gender and parental conflict impose the patient to take on a sick role. The patient did not have any external motivators neither did she reject anyof the investigations or consultations. Very few cases have been reported where bleeding initiated from the scalp, eye, nostrils, skin, urethral orifice, and anus.But in all such cases organicity should be ruled out,even the rarest one such as hematidrosis where Red Blood Cells (RBC) get mixed up with sweat presenting as bleeding from intact skin. Often medical teams land in a difficult situation as unrestricted investigation may enable indirect ways of abusing the system.Often the doctor patient relationship is at stake when parents are informed about suspected intentional production of symptoms, leading to repeated discharge against medical advice and lawsuits against doctors.Professionals who have little experience in psychiatry are liable to misdiagnose, underdiagnose or overtly diagnose the condition.[8]
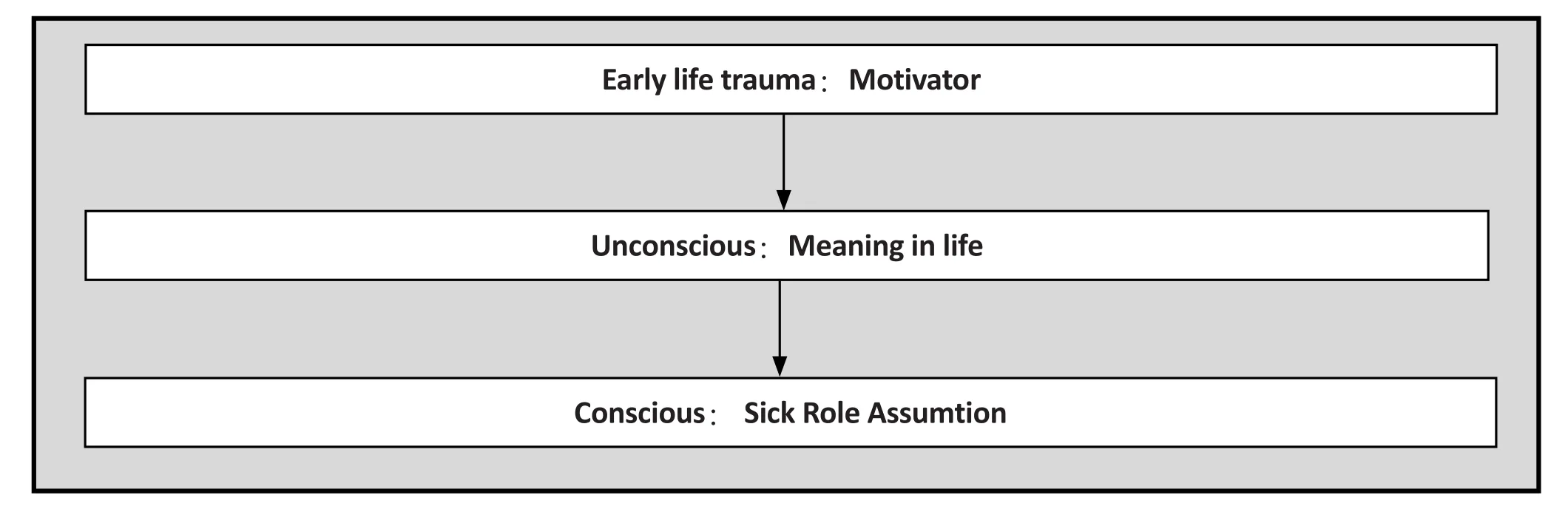
Figure1. The psychoanalytic underpinnings of the disorder
So, a tactful approach where both physical and psychological approaches are given equal importance with the help of interdepartmental liaison could be the ideal choice to prevent the imagined abandonment from the parts of caregivers. After ruling out the proxy phenomena, parents could be instructed to observe for 24 hours and maintain records of behavior. Although it is a legally conflicted procedure, covert video recording could also be helpful.[6]
The aim of reporting such cases is to give equal importance to psychological phenomena in the case of recurrent atypical presentation of bleeding disorder rather than putting it as a diagnosis of exclusion. Also,it describes the need for compulsory undergraduate and postgraduate training in psychiatry irrespective of various specialities. Multiple investigations and treatment options could simply be avoided if mental phenomena are considered in cases of bleeding disorder.
Conflict of interest
The authors declare that they have no conflict of interest related to this manuscript.
Funding
No funding support was obtained for preparing this case report
Informed consent
The patient signed an informed consent form and agreed to the publication of this case report.
Authors’ contributions
Concept of paper: DS, KA; Design: DS, DN, KA; Literature search: DS, MS, DN, KA; Clinical study: DS; Experimental study: DS; Data acquisition and analysis: DS; Statistical analysis: DS, MS, DN, KA; Manuscript preparation: DS, MS,DN, KA; Manuscript editing: DS, MS, DN, KA; Manuscript review: DS, MS, DN, KA; Guarantor: DS
1. World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. Geneva: World Health Organization;1992
2. Giotakis A, Kral F, Riechelmann H, Freund M. Intractable posterior epistaxis due to a spontaneous low-flow carotidcavernous sinus fistula: A case report and a review of the literature. Case Rep Otolaryngol. 2015;2015: 739019. http://doi.org/10.1155/2015/739019
3. Corry J, Kucik LT, Clenney T. Management of Epistaxis. Am Fam Physician. 2005;71(2): 305-311
4. Jafferany M, Bhattacharya G. Psychogenic Purpura (Gardner-Diamond Syndrome). Prim Care Companion CNS Disord. 2015;17(1). doi: http://doi.org/10.4088/PCC.14br01697
5. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Washington, DC; 2013
6. Uzuner S , Bahali K , Kurban S , Erenberk U , Cakir E. A pediatric case of factitious disorder with unexplained bleeding symptoms. Gen Hosp Psychiatry.35(6): 679.e7 - 679.e8. doi: http://doi.org/10.1016/j.genhosppsych.2013.03.003
7. Nadelson T. Munchausen spectrum. Borderline character features. Gen Hosp Psychiatry. 1979;1(1): 11–17
8. Bezner SK, Buchanan GR. Bleeding from the eyes and through intact skin: physiologic, structural, spiritual, or faked? Am J Hematol. 2013;88(8): 713–716. doi: http://doi.org/10.1002/ajh.23485
做作性障碍 —— 一例不明原因的鼻出血的罕见病因
Das S, Mohammed S, Doval N, Kartha A
心因性、鼻衄、人为的、压力
Summary:Epistaxis or nasal bleeding is a common condition which may be severe enough to warrant an urgent medical or surgical treatment. Factitious epistaxis is a rare entity. Due to a lack of exposure in complex behavioral issues during undergraduate training, it is quite natural on the part of a surgeon to miss the underlying emotional phenomena. Here, we present a case of factitious disorder which presented to the surgical causality with nasal bleeding. After proper evaluation and liaison with the department of otorhinolaryngology, we were able to manage the patient with antidepressants and cognitive behavioral therapy.
[Shanghai Arch Psychiatry. 2017;29(2): 120-123.
http://dx.doi.org/10.11919/j.issn.1002-0829.216063]
1Dept. of Psychiatry, Govt. T D Medical College, Alappuzha, Kerala, India.
2Dr. Somervell Memorial CSI Medical College, Karakonam, Kerala, India.
3The University College of Medical Sciences (UCMS) and Guru Teg Bahadur Hospital, Delhi, India.
*correspondence: Dr. Soumitra Das. Mailing address: C/420 PG Hostel, Vandanam Hospital, Alappuzha, India. Postcode: Kerala-688005. E-mail:soumitratdmc@gmail.com
概述:鼻衄或鼻出血是一种常见的疾病,有可能会严重到需要紧急医疗或手术治疗。人为的鼻出血是一种罕见的案例。对患者复杂的行为问题,在大学阶段的培训较少,因此,外科医生常常错过患者一些隐藏的心理问题。在这里,我们给出一例做作性障碍的病例,该案例由于鼻出血而进行手术。经过适当的评估并于耳鼻咽喉科会诊之后,我们采用抗抑郁药物和认知行为治疗成功治愈该患者。

Dr. Soumitra Das graduated and obtained a bachelor degree from the Agartala Govt. Medical College,Tripura, India in 2010, and a doctoral degree in psychiatry from the Govt. T D Medical College, Alappuzha,Kerala, India in 2015. Now he is working as a senior resident at the department of Psychiatry at the National Institute of Mental Health and Neuroscience, Bangalore, India. He is also a member of the Indian Psychiatric Society and IPS, Keraia. His research interests include ECT in clozapine resistant schizophrenia.

OBITUARY
With great sadness we announce the passing of Professor Desen Yang on March 31, 2017.Professor Yang was former vice president of Hunan Medical University, Hunan Medical University, former director of the Institute of mental health and the department of mental health, vice chairman of Psychiatry Branch of the Chinese Medical Association, and chairman of the editorial board of the Association of National Psychiatric Publication. He was 88 years old. Professor Yang will be greatly missed by his family and colleagues.
猜你喜欢
杂志排行
上海精神医学的其它文章
- Efficacy towards negative symptoms and safety of repetitive transcranial magnetic stimulation treatment for patients with schizophrenia: a systematic review
- Factors related to acute anxiety and depression in inpatients with accidental orthopedic injuries
- Placement instability among young people removed from their original family and the likely mental health implications
- A study of the characteristics of alexithymia and emotion regulation in patients with depression
- Efficacy and metabolic influence on blood-glucose and serum lipid of ziprasidone in the treatment of elderly patients with first-episode schizophrenia
- The current situations and needs of mental health in China
