经内耳钆剂MRI造影确诊的儿童梅尼埃病一例并文献复习
2017-11-01赵丹珩林勇生
刘 娅,赵丹珩,林勇生,刘 阳
经内耳钆剂MRI造影确诊的儿童梅尼埃病一例并文献复习
刘 娅,赵丹珩,林勇生,刘 阳
目的提高对儿童梅尼埃病的认识,以早期诊断、治疗。方法回顾性分析1例经内耳钆剂MRI造影确诊的儿童梅尼埃病患者资料,并复习国内外相关文献。结果患儿11岁,因发作性眩晕伴左耳耳鸣6年余就诊,眩晕每年发作约4~5次,左耳听力渐下降。多次就诊外院,行头颅MRI等检查未见异常,药物控制眩晕效果不佳。入我院后,结合病史、听力学检查结果,进一步行内耳钆剂MRI造影示双侧膜迷路积水,确诊梅尼埃病。行内淋巴囊减压术,术后随访3个月眩晕未再发作,听力未再继续减退。结论因儿童梅尼埃病患者内耳积水处于病变初始阶段,尚未引起症状,且患儿对症状的描述欠准确,导致诊断困难。内耳钆剂MRI造影检测到内耳积水可为本病诊断提供相对客观的证据。
梅尼埃病;儿童;眩晕;磁共振成像;误诊
梅尼埃病是以发作性眩晕、波动性听力下降、耳鸣和耳胀满感为特征症状的耳源性疾病,根据英国、美国和日本的流行病学数据,梅尼埃病的发病率为(34~190)/100万,发病年龄集中在40~60岁[1-3],儿童患者极少见,占全部患者数的0.4%~7.0%[4-6]。因为儿童患者对眩晕发作的表述往往欠准确,给诊断和治疗带来一定困难。我科2017年2月经内耳钆剂MRI造影确诊1例儿童梅尼埃病,患儿在长达6年的病程中始终未能明确诊断,现回顾性分析其临床资料,并结合文献探讨儿童梅尼埃病的诊治要点。
1 临床资料
男,11岁。因发作性眩晕伴左耳耳鸣、听力下降6年余入院。患儿6年前出现发作性旋转性眩晕,伴左耳耳鸣及波动性听力下降,眩晕持续3~5 h,眩晕缓解后耳鸣略减轻,每年发作4~5次。病程中多次就诊外院,行头颅MRI等检查未见异常,口服药物(具体不详)控制眩晕效果不佳。既往史:体健,无特殊疾病史。家族史:直系亲属中无类似症状发生。患儿来诊时为发作间期,专科检查:未发现自发及诱发性眼震,双耳鼓膜完整,标志清。纯音测听示:左耳中度感音神经性聋,0.5、1、2 kHz平均听阈约42 dB HL;右耳听力在正常范围。头颅MRI及颞骨CT检查未见异常。畸变产物耳声发射检查示:左耳未引出,右耳正常。左耳短声听性脑干反应阈值为50 dB HL,鼓室导抗示双耳A型曲线。前庭双温试验提示左侧前庭功能重度低下。根据病史和听力学检查结果,高度怀疑梅尼埃病,进一步行内耳钆剂MRI造影。于耳内镜下通过鼓膜穿刺向双耳鼓室内注射顺磁性造影剂钆喷酸葡胺(拜耳医药公司生产),稀释8倍(0.1 ml钆剂+0.7 ml 0.9%氯化钠注射液)约0.6 ml;24 h后行内耳MRI 3D-FLARE序列扫描,结果示:双侧前庭内淋巴间隙增宽(超过1/3),以左侧最为显著(图1);双侧耳蜗不确定。
2 结果
根据病史、听力学检查结果,以及MRI结果提示膜迷路积水影像,符合梅尼埃病诊断标准,确诊梅尼埃病。在全麻下行左侧内淋巴囊减压术。术后第3日出院,术后随访3个月,眩晕未再发作,听力较术前未降低。
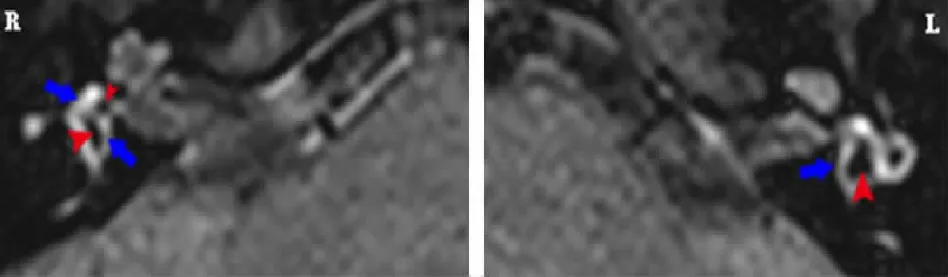
图1儿童梅尼埃病患者内耳钆剂MRI造影(水平位)示
双侧前庭内淋巴间隙增宽,以左侧明显,蓝色长箭头所示高信号区为前庭外淋巴,红色短箭头所示低信号区为内淋巴
3 讨论
3.1导致儿童眩晕的常见疾病 流行病学研究发现,8%~15%的儿童有眩晕病史,引起儿童眩晕的常见疾病为前庭性偏头痛(27.82%)、良性阵发性眩晕(15.68%)、前庭神经炎(9.81%)和梅尼埃病(4.08%)[7-8]。前庭性偏头痛患儿头痛常发生于额部或眶周,持续时间一般≤2 h,头痛和眩晕在发作时间上可能无相关性。儿童良性阵发性位置性眩晕发作时间为数秒至数分钟,发作频率常随着年龄增长而降低。前庭神经炎常有病毒感染或上呼吸道感染病史,发作持续时间为2~3周。此外,中耳炎、外伤和脑肿瘤等亦可导致眩晕发作,但明确病因相对容易。耳科医生需要对上述导致儿童眩晕的常见疾病进行仔细鉴别。
3.2梅尼埃病的病理特点 有学者对已故梅尼埃病患者头颅进行解剖发现,几乎所有患者内耳均表现为膜迷路积水[9]。因此,膜迷路积水成为梅尼埃病较公认的病理基础。然而,并非所有内耳膜迷路积水患者均会出现梅尼埃病的症状[10]。目前尚未明确膜迷路积水与梅尼埃病症状的出现有关系。大量颞骨解剖提示,约17%的儿童有不同程度的膜迷路积水;新生儿出现膜迷路积水的比率约为1.4%[11-12]。故可以认为儿童或青少年期静止性膜迷路积水可发展为中年期梅尼埃病。内淋巴积水导致膜迷路破裂、内外淋巴液离子混合后刺激眩晕感受器出现眩晕,被普遍用来解释梅尼埃病相关症状与内耳病理改变[13]。本例内耳钆剂MRI造影证实双侧膜迷路积水,以左侧为著,且眩晕、耳鸣、耳聋等梅尼埃病的典型症状出现于左耳。而本例造影提示的右耳前庭内淋巴积水,证实儿童期确实存在内淋巴积水这一病理状态,但尚未出现相应的临床症状。
3.3诊断标准 自1972年以来,美国耳鼻咽喉头颈外科学会对梅尼埃病的诊断进行了3次修订。近20余年来,我国对梅尼埃病的诊疗多遵循“1996年贵阳梅尼埃病诊疗指南”,2017年3月中华医学会耳鼻咽喉头颈外科学分会对梅尼埃病的诊疗指南进行了更新[14-15]。根据目前国内外最新指南,确诊梅尼埃病需满足以下4条:①2次或2次以上发作性旋转性眩晕,持续时间20 min~12 h;②听力损失符合低频、中频感音神经性聋,有波动性;③患耳有波动性听力下降、耳鸣和耳胀满感;④排除其他前庭疾病。新指南还将此病的检查手段分为基本检查和可选择的检查[15],但并未对儿童梅尼埃病做出特殊解释或说明。本例是在询问病史和行听力学检查的基础上,经内耳钆剂MRI造影增强扫描而明确诊断。目前公认的膜迷路积水判断标准是:前庭池内低信号的内淋巴区域超过整个前庭截面的1/3。
3.4内耳钆剂MRI造影的诊断意义 Gürkov等[16]认为,内耳钆剂MRI造影可直观地评价膜迷路积水的情况,如果医院MRI检查室具备相应的检查条件,应该对所有疑似梅尼埃病的患者行此项检查。内耳钆剂MRI造影将顺磁性造影剂钆喷酸葡胺从鼓室经圆窗膜和前庭窗环韧带间隙扩散进入外淋巴,但不能进入内淋巴;24 h后患者外淋巴区域在MRI 3D-FLAIR序列下呈高信号,而内淋巴区域呈低信号[17-18]。这一检查是半定量检查,受检查技术、主观判定影响较大[18],特别是耳蜗内积水主观判定较为困难[19-20]。故本例内耳钆剂MRI造影结果判定以前庭池内淋巴积水作为内耳内淋巴积水的依据,得到内耳造影的图像质量较高,能够客观证明膜迷路积水,为明确患耳内淋巴积水提供了相对客观的依据。
3.5延误诊治原因 眩晕的临床表现较为复杂,梅尼埃病的诊断又是“症状性诊断”,而且患儿可能受到年龄的限制对眩晕和听力下降的描述欠准确,从而造成诊断困难,这可能是文献报道儿童梅尼埃病“发病率较低”的原因之一[4-6]。本例年仅11岁,病程6年,多次就医但未能明确诊断,可能与患儿提供的发病信息不足及眩晕相关检查不够全面有关[21]。
综上,因儿童梅尼埃病患者内耳积水处于病变初始阶段,尚未引起症状,且患儿对症状的描述欠准确,导致诊断困难。本例提示,对发作性眩晕伴耳鸣、听力下降的患儿采用内耳钆剂MRI造影检查,在前庭池内检测到内耳积水可为梅尼埃病的诊断提供相对客观的影像证据。
[1] Shojaku H, Watanabe Y, Fujisaka M,etal. Epidemiologic characteristics of definite Ménière's disease in Japan. A long-term survey of Toyama and Niigata prefectures[J].ORL J Otorhinolaryngol Relat Spec, 2005,67(5):305-309.
[2] Alexander T H, Harris J P. Current epidemiology of Meniere's syndrome[J].Otolaryngol Clin North Am, 2010,43(5):965-970.
[3] Tyrrell J S, Whinney D J, Ukoumunne O C,etal. Prevalence, associated factors, and comorbid conditions for Ménière's disease[J].Ear Hear, 2014,35(4):e162-e169.
[4] Mizukoshi K, Shojaku H, Aso S,etal. Meniere's disease and delayed endolymphatic hydrops in children[J].Acta Otolaryngol Suppl, 2001,545:6-9.
[5] Filipo R, Barbara M. Juvenile Menière's disease[J].J Laryngol Otol, 1985,99(2):193-196.
[6] Brantberg K, Duan M, Falahat B. Ménière's disease in children aged 4-7 years[J].Acta Otolaryngol, 2012,132(5):505-509.
[7] Gioacchini F M, Alicandri-Ciufelli M, Kaleci S,etal. Prevalence and diagnosis of vestibular disorders in children: a review[J].Int J Pediatr Otorhinolaryngol, 2014,78(5):718-724.
[8] 沈丽芳,汤建国.儿童眩晕的诊治现状[J].临床耳鼻咽喉头颈外科杂志,2009,23(1):43-47.
[9] Ishiyama G, Lopez I A, Sepahdari A R,etal. Meniere's disease: histopathology, cytochemistry, and imaging[J].Ann N Y Acad Sci, 2015,1343:49-57.
[10] Merchant S N, Adams J C, Nadol J B Jr. Pathophysiology of Meniere's syndrome: are symptoms caused by endolymphatic hydrops?[J].Otol Neurotol, 2005,26(1):74-81.
[11] Bachor E, Karmody C S. Endolymphatichydrops in children[J].Otorhinolaryngol Relat Spec, 1995,57(3):129-134.
[12] Foster C A, Breeze R E. Endolymphatic hydrops in Ménière's disease: cause, consequence, or epiphenomenon?[J].Otol Neurotol, 2013,34(7):1210-1214.
[13] 刁明芳.前庭疾病——基于临床病例的诊断和治疗路径[M].湖北:湖北科技出版社,2017:107-111.
[14] Lopez-Escamez J A, Carey J, Chung W,etal. Diagnostic criteria for Menière's disease[J].J Vestib Res, 2015,25(1):1-7.
[15] 中华耳鼻咽喉头颈外科杂志编辑委员会,中华医学会耳鼻咽喉头颈外科学分会.梅尼埃病诊断和治疗指南(2017)[J].中华耳鼻咽喉头颈外科杂志,2017,52(3):167-172.
[16] Gürkov R, Pyyko I, Zou J,etal. What is Menière's disease? A contemporary reevaluation of endolymphatic hydrops[J].J Neurol, 2016,263(Suppl 1):S71-S81.
[17] Naganawa S, Satake H, Kawamura M,etal. Separate visualization of endolymphatic space, perilymphatic space and bone by a single pulse sequence; 3D-inversion recovery imaging utilizing real reconstruction after intratympanic Gd-DTPA administration at 3 Tesla[J].Eur Radiol, 2008,18(5):920-924.
[18] 杨凤,刘阳,王庆军,等.梅尼埃病内淋巴积水MRI影像诊断评价及影响因素分析[J].中华耳科学杂志,2015,13(3):493-496.
[19] 严进,彭利艳,成红政,等.梅尼埃病的内淋巴积水和积水程度3D FLAIR MRI显影[J].临床耳鼻咽喉头颈外科杂志,2015,29(5):421-424.
[20] Fukuoka H, Tsukada K, Miyagawa M,etal. Semi-quantitative evaluation of endolymphatic hydrops by bilateral intratympanic gadolinium-based contrast agent (GBCA) administration with MRI for Meniere's disease[J].Acta Otolaryngol, 2010,130(1):10-16.
[21] 吴子明,张素珍,苏平,等.儿童梅尼埃病[J].中华耳科学杂志,2008,6(4):424-427.
MeniereDiseaseinChildren(CaseReportandLiteratureReview)
LIU Ya, ZHAO Dan-heng, LIN Yong-sheng, LIU Yang
(Department of Otolaryngology, Head and Neck Surgery, Navy General Hospital, Beijing 100048, China)
ObjectiveTo improve the understanding of Meniere's disease in children and to achieve early diagnosis and treatment of Ménière's disease in children.MethodsThe clinical data of a child diagnosed as Ménière's disease depended on medical history, hearing results and inner ear MRI with Gadolinium enhancement were studied. Literatures about Ménière's disease in children were also reviewed.ResultsAn 11 year old boy presented to our clinic due to episode of vertigo and tinnitus of the left ear for 6 years. Vertigo The vertigo occurred 4-5 times a year and the hearing of the left ear was decreased gradually. The child was treated in other hospital for many times and got no efficacy result. Ménière's disease was confirmed depended on detailed medical history, hearing results and inner ear MRI with Gadolinium enhancement. The inner ear MRI examination demonstrated an enlarged endolymphatic space in vestibule, which was consistent with the pathology of endolymphatic hydrops of Ménière's disease. Endolymphatic sac decompression was performed on this child. During more than 3 months' follow up, there was no recurrence of dizziness and hearing was preserved after surgery.ConclusionEndolymphatic hydrops exists in the early stage in children with Ménière's disease. Children may give inadequate information of the clinical characters of dizziness, which may mislead to the difficult to diagnosis. Inner ear MRI examination with Gadolinium enhancement can detect endolymphatic hydrops, and provide objective evidence for the diagnosis of Ménière's disease.
Meniere disease; Child; Vertigo; Magnetic resonance imaging; Misdiagnosis
军队后勤科研基金资助项目(BWS14J***)
100048 北京,海军总医院全军耳鼻咽喉头颈外科中心
刘阳,E-mail:liuyangdoc@sina.com
R764.33
A
1002-3429(2017)10-0013-04
10.3969/j.issn.1002-3429.2017.10.005
2017-05-24 修回时间:2017-08-03)