Ex Vivo Lung Perfusion:Scientific Research and Clinical Application
2017-09-08XinliangGaoWeiLiuMingyaoLiuLatnerThoracicSurgeryResearch
Xinliang Gao,Wei Liu,Mingyao Liu(. Latner Thoracic Surgery Research
Laboratories, Toronto General Hospital Research Institute, Department of Surgery and Institute of Medical Science, Faculty of Medicine, University of Toronto, Toronto, Ontario, Canada;2. Department of Thoracic Surgery, Bethune First Hospital, Jilin University, Changchun, Jilin 130021, People's Republic of China)
【编者按】刘明耀教授是多伦多大学临床医学研究生院院长、外科教授、资深科学家,主要从事肺移植的临床与科研工作。主持科研课题27项,主要参与课题10项,曾荣获伊丽莎白二世女王钻石禧年奖章。其所在的多伦多大学总医院于1983年和1986年分别完成了世界首例成功的单肺及双肺移植,肺移植的相关临床及科研水平处于世界第一位。近年来成功研发了体外肺灌注装置(ex-vivo lung perfusion,EVLP),200多例经临床鉴定不可使用的肺脏经过此装置修复后已经成功用于移植,效果甚佳,引起全球轰动。EVLP是一种新型的肺脏体外灌注技术,可以在体外为供肺提供通气和血供,并可在灌注期间对供肺进行快速的功能评估和干预治疗。因此,EVLP技术可在移植前有效延长供肺保存时间,提高供肺质量,为受损伤供肺,尤其是边缘性供肺提供了体外修复的可能,可显著增加适合移植的供肺数量,提高边缘供肺的利用率,有效缓解供肺短缺的现状。刘明耀教授团队已协助全球包括我国在内的多家医疗中心开展肺移植的临床及科研工作,其中EVLP装置的深入研发及多中心临床试验也是刘教授团队与天津市第一中心医院沈中阳教授团队合作承担的国家国际科技合作专项项目的主要研究内容之一,无锡人民医院陈静瑜教授团队也参与了研究,将对我国肺移植的发展起到积极的促进作用。
Introduction
Lung transplantation is a standard treatment for patients with end-stage lung diseases. Data from the International Society for Heart and Lung Transplantation (ISHLT) showed that 3 973 adult lung transplantation procedures were performed in 20141. Despite the growing interests on lung transplantation, only about 20% of lungs from donations after brain death (DBD) have been used for transplantation2-3. The worrisome of development of primary graft dysfunction (PGD) makes physicians conservative in donor lung selection. PGD is the major cause of mortality within the first year after transplantation4. It is also a major risk factor for development of chronic lung allograft dysfunction,which is the leading cause of death in lung transplant patients5. The deficit of donor lungs resulted in American waitlist mortality reaching at 16.5 deaths per 100 waitlist years in 20156. In order to increase the suitable donor lungs, donations after cardiac death(DCD) have been included for lung transplantation.According to ISHLT DCD registry, there were 306 DCD donor lung transplantations performed between 2003 and 20137. The lack of objective assessment of donor lungs prevented the use of marginal donor lungs for transplantation.
Normothermic ex-vivo lung perfusion (EVLP) is a novel technology to overcome the shortage of donor lungs. EVLP provides donor lungs with ventilation and perfusion at body temperature8. This technique allows assessment of physiological as well as biological functions of donor lung prior to transplantation, extends the time of donor lung preservation, and facilitates the repairing of lung injury. It has increased the utilization of marginal donor lungs for transplantation. With rapid molecular assessments of donor lung and advanced therapeutic intervention during EVLP, more and more donor lungs will become suitable for transplantation with improved quality. The present review introduces the clinical application, current research status and future development of EVLP.
Rationale
The current gold standard of donor lung preservation is cold static preservation. The donor lungs are flushed with cold low potassium dextran preservation solution,followed by topical cooling and lung ventilation9. Then,the lungs are transported in a static inflated state at 4℃.Hypothermia reduces the metabolism of the donor lungs(5% of metabolic rate at 37℃), which is beneficial to maintain cell viability and slow down cell death processes10. However, the cold static preservation technique is limited in that the static status prevents the removal of harmful substances released from the lung tissue and precludes the assessment and repair of donor lungs.
An advantage of EVLP is that it returns and maintains the donor lungs at body temperature, which allows the pulmonary cells to remain metabolically active and viable11. During this time period, lung edema could be relieved and harmful substances be removed, so that homeostasis of the donor lungs could be maintained.Mechanical ventilation may reduce atelectasis, and perfusion may improve microcirculation. Passenger leukocytes, a primary cause of cellular rejection, could also be removed during EVLP12. In the EVLP circuit,oxygen is removed from and carbon dioxide is supplied to the perfusate via a membrane oxygenator. This allows for the assessment of oxygenation function of the lung.Addition of carbon dioxide helps maintain the pH of the perfusate. EVLP also provides opportunities to repair donor lungs with advanced rehabilitation and immunomodulation.
EVLP Protocols
Three different EVLP protocols have been reported from the University of Toronto, University of Lund,and Organ Care System (OCS), respectively. The differences among these three protocols are shown in Table 1.

Table 1. Comparison between different ex vivo lung perfusion protocols
Toronto protocol is able to maintain lungs in the EVLP system for extended period. Toronto protocol uses an acellular perfusate, lower perfusion flow to avoid hemodynamic stresses13. The EVLP circuit maintains a positive left atrial pressure that can prevent collapse of the microvasculature, decrease edema formation and reduce microcirculation failure14. After the left atrium and pulmonary artery cannula are connected to the EVLP circuit, anterograde flow is initiated at 150 ml/min with the perfusate at room temperature. The temperature of the perfusate is then gradually increased to 37℃ over the next 30 min. When the temperature reaches 32-34℃, mechanical ventilation is started and the perfusate flow rate is gradually increased to the targeted flow (40% of estimated donor cardiac output)within 60 min. Once ventilation is started, mixed gas(86% N2, 6% O2, 8% CO2) is used to deoxygenate the perfusate, and to provide carbon dioxide to the inflow perfusate via a gas exchange membrane, to maintain PaCO2between 35 and 45 mmHg(1 mmHg =0.133 kPa). The steroid, antibiotic, and heparin are added to the perfusate prior to EVLP initiation.Hemodynamics, ventilation and oxygenation capacity parameters are assessed every hour. Bronchoscopic examination and radiographs of the lungs are performed every 2 h. A partial exchange (250 ml) of fresh perfusion solution is performed every 2 h. The Lund and OCS protocols are similar to the Toronto protocol with modifications (Table 1).
Development and Clinical Experience of Toronto EVLP Protocol
Ex vivo organ perfusion was first reported in 1935,when Alexis Carrel and Charles Lindbergh successfully performed ex vivo organ perfusion at body temperature15.In 1970, Jirschet al. described first isolated EVLP to assess and maintain lungs. However, this EVLP attempt was unsuccessful due to severe lung edema and increased pulmonary vascular resistance (PVR)16.The EVLP wasn't successful until the development of STEEN SolutionTM—an extracellular buffer with high concentration of albumin to maintain colloid pressure.Steen et al. performed the first clinical EVLP case in 200317. In that study, the donor lung was perfused only for 60 min, because of the development of lung injuries with increased PVR and airway pressures18.
The broader clinical applications of EVLP for assessment of donor lungs began after the development of Toronto EVLP protocol. The Toronto group has significantly modified the EVLP technique and performed this procedure with swine lungs to maintain stable lung function for up to 12 h8. In 2007, Toronto group designed and registered the first clinical trial on EVLP. The first clinical case using Toronto EVLP protocol succeeded in 200819. Two years later, the clinical trial data were reported in The New England Journal of Medicine20. The incidence of PGD 72 h after transplantation was 15% in 20 EVLP lungs and 30% in 116 standard lungs. There was no significant difference in 30-day mortality, bronchial complications, duration of mechanical ventilation, or length of staying in an intensive care unit (ICU)/hospital between the two groups. No severe adverse events related to EVLP were reported20.
In 2012, the Toronto group updated the clinical data to 50 lungs (22 DCD and 28 DBD lungs) that were transplanted after EVLP. The EVLP treated lungs had similar PGD rates 72 h after transplantation, as well as similar extubation time, ICU/hospital staying lengths, thirty-day mortality rate and 1-year survival rate compared to 267 standard lung transplantations21.This technique was approved by the Ontario Health Technology Advisory Committee (OHTAC) and Canadian Ministry of Health (MOH) in 2012, and by U.S. Food and Drug Administration (FDA) in 2014.
In 2015, long-term data showed that 63 patients receiving lungs assessed by EVLP had a 5-year survival rate of 71% compared to 340 conventional donor lung recipients receiving contemporary transplants in which the 5-year survival rate is 57%. Functional measures such as the absence of chronic lung allograft dysfunction, highest forced expiratory volume in 1 s(FEV1) predicted, six-minute walk distance, and acute cellular rejection episodes were similar between the EVLP and control groups. There is a significant improvement in life quality after lung transplantation in both groups22.
A recent study by the Toronto group investigated the lung transplantation outcomes after DCD with EVLP.The 27 recipients received DCD lungs without EVLP(DCD-no EVLP group) were compared to 28 recipients who received DCD lungs with EVLP (DCD-EVLP group). In addition, 570 date-matched standard DBD lung recipients were also included in this study for comparison. There were no major differences between the DCD recipients and the DBD recipients for multiple measures, including mechanical ventilation duration,ICU stay, 1-, 3-, and 5-year survival rates. However,compared to DCD-no EVLP group, DCD-EVLP recipients had a shorter hospital stay23. Considering the EVLP protocol was used to assess the marginal donor lungs, the equivalent results between the two groups are very impressive and important. The development of EVLP techniques and clinical reports of Toronto EVLP protocol are shown in Table 2.
Research to Advance the EVLP Technique
The EVLP technique has been undergone investigations continuously. These researches have helped to improve the quality of the system and the procedure, and to develop EVLP as a platform for donor lung repair.
Technical development of EVLP
Close vs. Open Left Atrium
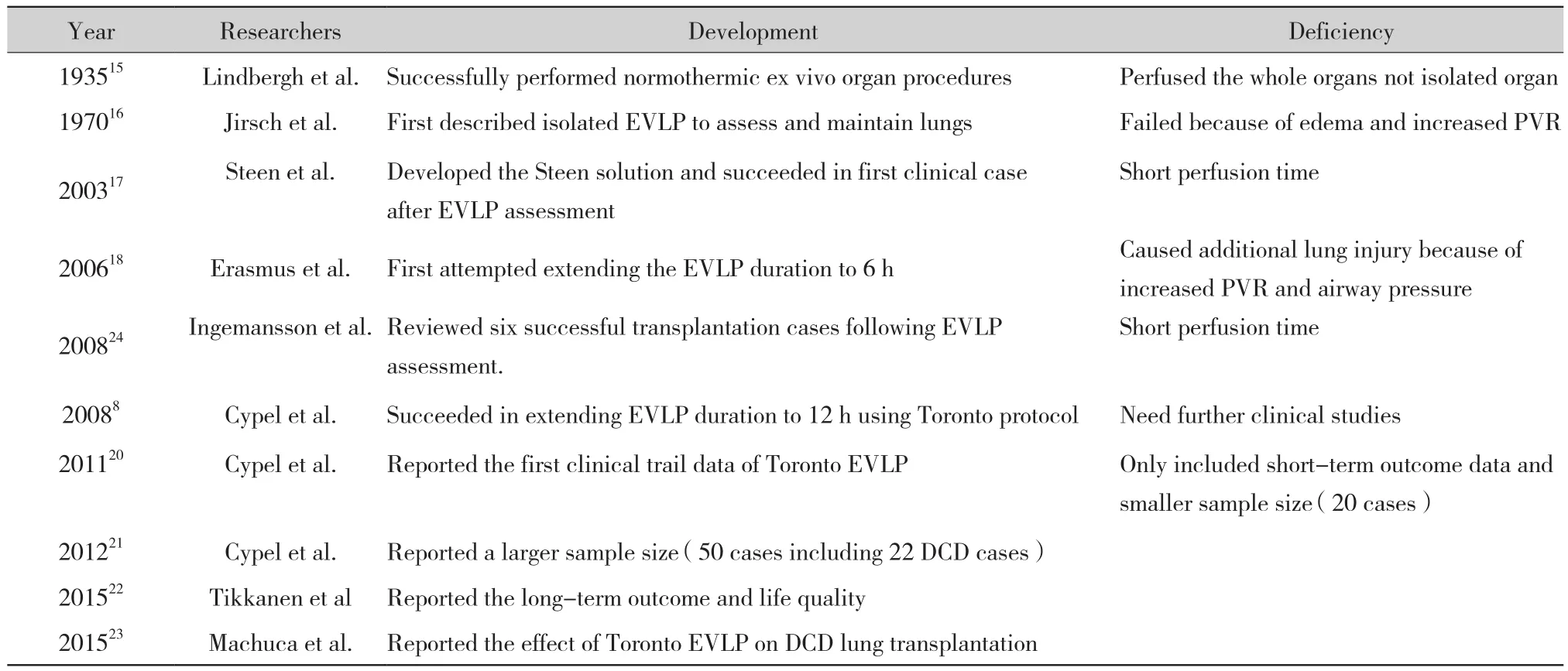
Table 2 Development and Clinical Reports of Toronto EVLP
As shown in Table 1, the closure or opening of the left atrium is one of the differences among the 3 protocols for clinical EVLP. The closure of the left atrium provides a left atrial pressure of 3-5 mmHg. This pressure may expand the pulmonary vessels and capillary bed, and reduce PVR. However, it requires surgical training and takes time;to keep the left atrium open is much easier and less technical demanding. In 2002, Petaket al. and Broccardet al. found that sufficient left atrial pressure improved pulmonary functions in rat and rabbit EVLP models, respectively14,25. In 2016,Linacreet al. compared the effects of the closurevs. opening of the left atrium on the lung mechanics and hemodynamic parameters of porcine donor lungs during EVLP. They found that opening the left atrium considerably increased PVR for prolonged (12 h)EVLP, with decreased oxygenation and compliance.In contrast, with the closure of the left atrium, the lung mechanics and hemodynamic parameters were more stable. Moreover, lung edema in donor lung with opened left atrium was more severe than that with the closed one26. Collectively, these findings demonstrate the benefits of closing the left atrium to maintain normal function in the donor lung during prolonged EVLP. To overcome the technical challenges of closing the left atrium, a specially designed adaptor has been designed and under further testing.
Acellular vs. Cellular Perfusate
Another disputed issue is whether the perfusion should be supplemented with erythrocytes, to better mimic the physiological condition, and to better evaluate oxygenation capacity during EVLP. Two studies compared the effect of EVLP with or without erythrocytes during EVLP. Romanet al. reported that there were no significant differences in PVR,pulmonary compliance, ratio of partial oxygen pressure to fraction of inspired oxygen, dry/wet weight ratio of the lung, number of immunocytes in the lung,and ultrastructure of the lung tissue between the two groups. However, interleukin-8(IL-8) level in the bronchoalveolar lavage was significantly higher when using perfusate without erythrocytes. The EVLP was only lasted for 4 h in that study; therefore, the effect of prolonged EVLP was not elucidated13. In 2016, Beckeret al. investigated the effect of perfusate supplemented with or without erythrocytes in EVLP for 12 h. No significant difference was observed in the oxygenation capacity and ultrastructure of the lung. However,prolonged EVLP with perfusate containing erythrocytes showed significantly higher PVR and pulmonary arterial pressure27. It appears that both protocols are compatible for current clinical applications (less than 6 h EVLP).However, if more injured lungs need to be repaired for prolonged times, this question needs to be considered.Methods of Ventilation and Perfusion
Several studies investigated the effects of different protocols of perfusion and ventilation during EVLP.Ventilation protocols can be divided to volume controlled and pressure controlled models. To ensure tidal volume of the donor lungs during EVLP and to prevent alveolus collapse and atelectasis, the volumecontrolled protocol is commonly used. However,the pressure-controlled protocol may be beneficial for improving lung hemodynamics and preventing pulmonary barotrauma28. Mehaffeyet al. compared the conventional volume-controlled ventilation with an airway pressure release ventilation during EVLP with porcine DCD lungs, followed by single left lung transplantation. The airway pressure release ventilation group showed higher oxygenation capacity and pulmonary compliance during the reperfusion of the lung grafts29.
All three current EVLP protocols use centrifugal pumps or roller pumps to provide continuous pulmonary perfusion. However, pulse-type pulmonary perfusion better resembles pulmonary perfusion under physiological conditions. To determine if pulse-type perfusion is superior to continuous perfusion, Schumeret al. examined the effects of each method on lung physiology. They reported that there was no apparent difference between pulse-type EVLP and continuous EVLP in lung oxygenation capacity, pulmonary edema and peak airway pressure30. Using rat heart-lung blocks, Tanaka perfused both pulmonary and bronchial arteries during EVLP. This dual-EVLP method effectively reduced inflammatory response and improved post-transplantation microcirculation and functions of the lung by triggering mitochondrial respiration31.
The ventilation and perfusion strategies should be further studied, and better techniques should be integrated into the current protocols, to improve the quality of donor lungs.
Evaluation of donor lungs during EVLP with biomarkers
An accurate functional evaluation of donor lungs during EVLP is important for the selection of suitable donor lungs for transplantation. The primary indicators of pulmonary function in vivo are the ratio of arterial oxygen partial pressure and the fraction of inspired oxygen. However, these indicators are insufficient for ex vivo lung perfusion, especially when acellular perfusate is used; measurements related to pulmonary vessels and airways should be considered32. The Toronto group suggested the following criteria prior to transplantation of the donor lungs: the ratio of oxygen partial pressure and the fraction of inspired oxygen from left atrium above 400, stable or decreasing pulmonary arterial pressure and airway pressure, and stable or increasing pulmonary compliance33. In addition to these physiological assessment, biomarkers together with rapid molecular diagnosis techniques are under developing.
The perfusate provides samples for biological assessment to help predicting the development of PGD. Machucaet al. found that the levels of stem cell growth factor-β at 1 h post-EVLP, IL-8 and growthregulated oncogene-α at 4 h post-EVLP correlated with patients' post-transplantation outcome34. Hashimoto et al. reported that soluble adhesion molecules in the EVLP perfusate are associated with incidence of PGD35.Machuca et al. further found high endothelin-1 (ET-1)levels in the EVLP perfusate as a potential biomarker to predict the PGD. Sageet al. developed a nanochip technique that can measure the ET-1 levels in the perfusate within 30 min36-37. The rapid molecular diagnosis technique should be further developed, which may provide objective assessment of the quality of the donor lung, and as an indicator of the effectiveness of donor lung repair.
Repair injured donor lungs during EVLP
EVLP provides a platform for ex vivo treatment of donor lungs. Multiple therapeutic strategies have been explored with EVLP system.
Injury specific treatments
The use of high-dose empirical antibiotics on infected human donor lungs during EVLP reduced bacteria in the lung and improved the lung functions38. The spectrum of bacterial infection and resistance to antibiotics varies from different countries and even different cities and hospitals. To identify site-specific infections may help to chose more effective antibiotics.The EVLP also allows the use of high dose of antibiotics with less concerns of side effects on other organs.Treatment of infection ex vivo may prevent and reduce infection-associated complications during and after lung transplantation.
Aspiration of stomach contents is a common complication in multi-organ donors and may lead to infection and damage of donor lungs. It is also one of the common reasons to decline donor lungs. In a swine lung model,Khalife performed aspiration of the stomach contents by bronchoalveolar lavage using solution containing exogenous surfactant. As a result, the donor lungs exhibited better oxygenation capacity39. Inciet al. also found that aspiration of the gastric acid and intra-airway administration of exogenous surfactant on donor lungs during EVLP, improved the oxygenation capacity, reduced pulmonary arterial pressure and alleviated pulmonary edema40. Nakajimaet al. used acid aspiration to develop severe lung injury in pigs,and then combined bronchoalveolar lavage and surfactant administration during EVLP, followed by lung transplantation. They demonstrated that the lung functions were not only improved during EVLP, but also after lung transplantation41.
Donor lung thrombosis is another major cause of PGD post-transplantation42. Motoyamaet al. reported that following warm ischemia, fibrinolysin administration during EVLP in murine lungs reduced PVR, resulting in alleviation of pulmonary edema and improvement in the oxygenation capacity and pulmonary compliance43-44.Machucaet al.did pulmonary thrombolysis in a human donor lung during EVLP, and then transplanted it successfully45.
When the clinical diagnoses are clear (e.g., infection,acid aspiration or pulmonary thrombosis), these treatments can repair the donor lungs in an injury specific manner. On the other hand, most of donor lungs suffering from inflammation and cell death,broader treatments are required to ameliorate related lung injury.
Drugs as therapeutics
There are two subtypes of adenosine receptor-2,A2A and A2B. Stoneet al. found that supplementing A2A receptor agonist during EVLP reduced proinflammatory mediator expression in murine lungs after DCD. As a consequence, pulmonary edema was reduced and pulmonary function was improved46. According to Wagneret al., after prolonged cold preservation,treatment of DCD donor lungs with an adenosine A2A receptor agonist during EVLP enabled PaO2/FIO2ratios greater than 400 mmHg after transplantation in a pre-clinical porcine model47. By contrast, the A2B receptor antagonists suppress the pro-inflammatory response in typeⅡalveolar epithelial cells48. A2B receptor antagonism during EVLP attenuated ischemiareperfusion induced lung injury and augmented reconditioning of DCD lungs49. β-receptor agonists,as bronchodilators, can relieve airway spasm and reduce airway pressure. It has been demonstrated that inhalation of β-receptor agonists during EVLP alleviates pulmonary damage and improves pulmonary function50-51. Steroids can reduce inflammatory and immune responses. In 2016, Martenset al. reported that administering steroids before cardiac failure and during EVLP enhanced pulmonary compliance, reduced pulmonary edema and production of inflammatory factors in DCD lungs. However, no improvement was observed in PVR or lung oxygenation capacity52.
Therapeutic gases
Therapeutic gases may also provide a new avenue for reducing donor lung damage. According to Donget al.,administration of nitric oxide to DCD donor lungs before and after lung retrieval alleviated lung edema during EVLP. It also reduced PVR and improved oxygenation after transplantation53. Inhalation of carbon monoxide also enhanced the oxygenation capacity of DCD donor lungs and dramatically reduced the transcription or expressions of cytokines related to the ischemiareperfusion injury54. Another gas inhaled to improve lung function is hydrogen. Noda et al. showed that inhaling 2% hydrogen during EVLP significantly alleviated pro-inflammatory response in EVLP and improved mitochondrial oxygen metabolism, and contributed to a better post-transplantation outcome55. It was proved by Haam in 2015 that inhaling 2% hydrogen reduced PVR and pulmonary arterial pressure. This was accompanied by a dramatic reduction in the release of inflammatory mediators, such as IL-1β, IL-6, IL-8 and TNF-α56. Inert gases, such as argon and xenon,have been shown to exert protective properties against cell apoptosis and inflammatory response induced by ischemia-reperfusion injury. However, according to Martenset al., ventilation with argon and xenon during EVLP did not improve graft function57. The clinical application of these gas molecules should be further tested and considered.
Biological treatments
Mesenchymal stromal cells (MSCs) have been used to treat pulmonary damage induced by chemotherapy drugs, endotoxins, mechanical ventilation and bacteria58-61. In 2015, Gennaiet al. showed that supplementing human donor lungs declined from clinical program with micro vesicles derived from human MSCs during EVLP improved lung function and hemodynamic parameters, and alleviated pulmonary edema62. To determine the optimal route and dose of MSCs, Mordant et al. performed EVLP in a swine donor lung model. It was found that intravascular (but not intrabronchial) delivery of 150×106MSCs improved outcome of the lungs perfused ex vivo63.
IL-10 is an anti-inflammatory cytokine. An increase in the production of IL-10 in donor lung may alleviate inflammatory response and improve donor lung function64. EVLP provides a time window for expression of therapeutic genes and gene products before lung transplantation. In 2009, Cypelet al. performed intraairway administration of the adenoviral vector mediated IL-10 gene delivery into donor lungs during EVLP. The results showed that overexpression of IL-10 inhibited inflammation in human lungs, up-regulated the levels of anti-inflammatory mediators, improved oxygenation capacity and decreased PVR65. In 2017, Machucaet al. performed intra-airway administration of the adenoviral vector carrying IL-10 gene into swine lungs during EVLP. These donor lungs were transplanted to recipients and animals were maintained alive for 7 days.It was shown that not only the ex vivo treatment with IL-10 gene was safe but also improved post-transplantation lung functions66. This large animal survival pre-clinical study may lead to a clinical trial.
Establishing Donor Lung Repair Centers
Since EVLP is a complex procedure requiring experienced teams and equipment, it may not be necessary for every lung transplantation center to develop this technique. In 2012, a marginal donor lung was remotely transported to University of Toronto Lung Transplant Program for EVLP, and then to the recipient center,and transplanted successfully67. Using a pig lung transplant model, Hsin et al. demonstrated that after EVLP, the donor lungs preserved for another 10 h at 4℃ before transplantation, had excellent outcome68.Inspired by these studies, it has been recommended to establish regional donor lung assessment and repair centers (ARCs). In this way, donor lungs could be obtained and prepared with the standard procedures in the donor centers, and then transported to the ARC, where the lungs could be assessed and repaired properly. If the donor lungs are deemed to be suitable or made suitable for transplantation, the lungs would then be shipped either nationally or internationally to the recipient centers for most suitable recipients. This will greatly facilitate the quality and quantity of lung transplantation.
With further development of ex vivo perfusion systems to other solid organs, the ARCs could function as a hub for multiple organ procurement, assessment, repair and distribution. This will dramatically change the practices of organ donation, management and utilization worldwide.
Advanced EVLP Devices
The EVLP circuit is composed of multiple individual devices. Several research groups and companies have been developing EVLP as portable medical devices. The next generation of EVLP systems will be a standardized medical equipment that streamlines the EVLP process with less demand on the technical training, to drastically reduce hospital costs, space in the operating room allocated for EVLP. The device may be mobile,making it well suited for donor lung transport.
These medical devices can be further developed to perfuse multiple different organs simultaneously;either separately or in the same circuit. It is possible that organ-organ interaction may maintain organ functions better ex vivo. It may further improve the quality of multiple organ transplantation.
Conclusions
EVLP is a novel technology that extends the donor lung preservation, and enables the assessment and repair of donor lungs prior to transplantation. This method holds significant potential to increase the number of suitable donor lungs and improve transplantation outcomes.Current research investigates how EVLP can be utilized for treatment and repair of damaged lungs, and how the lung grafts can be altered to reduce immune response following transplantation. Future research will focus on standardization and simplification of EVLP system. It is possible to establish donor lung assessment and repair centers for transplantation.
