Clinical efficacy of acupuncture in treatment of chronic urticaria and its effects on the content of IgE and the imbalance of Th1/Th2 cell function
2020-04-21ZhangXin张欣JiJun纪军
Zhang Xin (张欣), Ji Jun (纪军)
Shanghai Research Institute of Acupuncture and Meridian, Shanghai 200030, China
Abstract Objective: To observe the clinical efficacy of acupuncture in treatment of chronic urticaria and the change in the content of serum immunoglobulin E (IgE), and to discuss the effect of acupuncture on the imbalance of T helper(Th)1/Th2 cell function via observing the changes in the contents of interferon-γ (IFN-γ) and interleukin-4 (IL-4).Methods: Ninety patients meeting the inclusion criteria of chronic urticaria were randomized into an acupuncturemedication group, an acupuncture group and a Western medication group by the random number table method. The acupuncture-medication group was intervened by acupuncture, cupping, collateral-pricking bloodletting and oral administration of cetirizine hydrochloride tablets; the acupuncture group was treated with acupuncture, cupping and collateral-pricking bloodletting; the Western medication group only received oral administration of cetirizine hydrochloride tablets. Before treatment and after 6-week treatment, the changes in the symptom scores and the contents of serum IgE, IFN-γ and IL-4 in the three groups were observed.Results: There were no significant differences in the total effective rate among the three groups (all P>0.05), but the cured and markedly effective rate was significantly higher in the acupuncture-medication group than that in the Western medication group (P<0.05). After treatment, the total symptom score decreased in the three groups (P<0.05),and the improvement of total symptom score in the acupuncture-medication group was more significant than that in the Western medication group (P<0.05). The component symptom scores all decreased after treatment in the three groups (all P<0.05); the improvements of the scores of itch intensity, and skin lesion size and number were more significant in the acupuncture-medication group than in the Western medication group (all P<0.05); the improvement of the skin lesion size score was more significant in the acupuncture group than in the Western medication group(P<0.01). The contents of IgE and IL-4 dropped (all P<0.05) and the content of IFN-γ increased (P<0.05) after treatment in the three groups; the post-treatment changes in the serum contents of IgE and IFN-γ were more significant in the acupuncture-medication group than in the Western medication group (both P<0.05). The incidence rate of adverse reactions was significantly lower in the acupuncture-medication group and acupuncture group than in the Western medication group (both P<0.05), and the relapse rate was significantly lower in the acupuncture-medication group than in the Western medication group (P<0.05).Conclusion: Combined acupuncture and medication can enhance the cured and markedly effective rate in treating chronic urticaria. Acupuncture is equivalent to cetirizine hydrochloride tablets comparing the clinical efficacy in treatment of chronic urticaria. Acupuncture plus medication and acupuncture alone both can effectively mitigate the clinical symptoms, with low incidence of adverse reactions. The relapse rate is low when using acupuncture together with medication. Acupuncture plus medication can work better in regulating the contents of IgE and IFN-γ and improving the imbalance of Th1/Th2 cell function.
Keywords: Acupuncture Therapy; Cupping Therapy; Blood-letting Puncturing and Cupping Therapy; Acupuncture Medication Combined; Urticaria; Immunoglobulin E; Interferon-gamma; Interleukin-4
Chronic urticaria is a common dermatological condition, referring to urticaria that repeatedly attacks exceeding 6 weeks. It belongs to the scope of Feng Sao Yin Zhen (itching skin and rashes) in traditional Chinese medicine (TCM). It can happen in any age groups and seasons but is more likely to attack in spring. In Europe and America, 0.1%-0.3% of the population are affected and women are twice as many as men[1]. Over 40% of the patients may suffer for over half a year and half may get a remission within 1 year, but in some cases, it may last for 10 years or even longer[2].
Autoimmune dysfunction is a significant factor in the development of chronic urticaria. Multiple studies have shown that abnormal immunoglobulin E (IgE) level is involved in the pathogenesis of chronic urticaria[3-4].One domestic study[5]found that about 47.37% of chronic urticaria patients presented abnormally high serum IgE level. More and more researchers have now focused on the imbalance of the function of T helper(Th) cell subsets in chronic urticaria patients, especially the imbalance of Th1/Th2 cell function. Interferon-γ(IFN-γ) is mainly produced by Th1, so that increased serum level of IFN-γ usually indicates hyper-function of Th1 cells; interleukin 4 (IL-4) is produced by Th2 cells and when its serum level increases it suggests hyperactive Th2 cells[6]. IFN-γ and IL-4 are antagonistic to each other, working to inhibit the generation of IgE[7].Therefore, detection of the changes in IFN-γ and IL-4 can indirectly observe the balance between Th1 and Th2 cells. Several clinical trials[8-10]have approved the effectiveness of acupuncture-moxibustion in the treatment of chronic urticaria despite the vague action mechanism. This study aimed to discuss the mechanism of acupuncture-moxibustion in treating chronic urticaria through observing the clinical efficacy and the changes in serum levels of IgE, IFN-γ and IL-4.
1 Materials and Methods
1.1 Diagnostic criteria
The diagnostic criteria were made by referring to the Diagnosis and Treatment Guidelines for Urticaria(2007)[11]. Sudden attack of wheals in different shapes and sizes with clear boundary; coupled with recurrent itching skin and rash that occurred randomly and usually left no trace after release; positive dermatographic test.
1.2 Inclusion criteria
Conformed to the diagnostic criteria of chronic urticaria; lasted over 6 weeks; not using corticosteroids within the previous 1 month and not on antihistamines within the previous week; serum IgE ≥100 ug/L; had no contraindication for the medications adopted in this study.
1.3 Exclusion criteria
Acute urticaria; aged <20 or >65 years; severe complications such as liver or kidney dysfunction,gastric ulcer and infections; pregnant or breastfeeding women.
1.4 Reject and dropout criteria
Not in line with the inclusion criteria but enrolled by mistake; missed the treatment or occurred severe systematic symptom during the study or terminated the observation on one’s own; developed other severe diseases that interfered with the observation.
1.5 Statistical methods
The SPSS version 18.0 software was used for statistical analysis. When in normal distribution, the measurement data were expressed as mean ± standard deviation (x ±s) and the numeration data were expressed as rate. Data in abnormal distribution were expressed as median (lower quartile, upper quartile)[M(QL, QU)]. When measurement data met normal distribution andhomogeneity of variance,inter-group comparisons were conducted using multi-sample ANOVA and intra-group comparisons before and after treatment were performed using paired t-test.Measurement data in abnormal distribution were examined using non-parametric rank-sum test. The effective rate was compared by Chi-square test. When dropout data were analyzed, the missing values were directly deleted based on the correlation analysis.P<0.05 indicated statistical significance.
1.6 General data
Between November 2015 and November 2018, a total of 90 eligible chronic urticaria patients were recruited from the Clinic of Shanghai Research Institute of Acupuncture and Meridian, the Acupuncturemoxibustion Outpatient of Shanghai Huangpu District Hospital of Integrated Chinese and Western Medicine,and the Acupuncture-moxibustion Outpatient of Yueyang Hospital of Integrated Chinese and Western Medicine, Shanghai University of Traditional Chinese Medicine. They were divided into an acupuncturemedication group, an acupuncture group and a Western medication group, with 30 cases in each group. There were 4 dropout cases (2 cases from the acupuncturemedication group and 2 cases from the acupuncture group), and finally eighty-six patients completed the study. There were no significant differences comparing the data of gender, age and disease duration among the three groups (all P>0.05), indicating the comparability(Table 1).
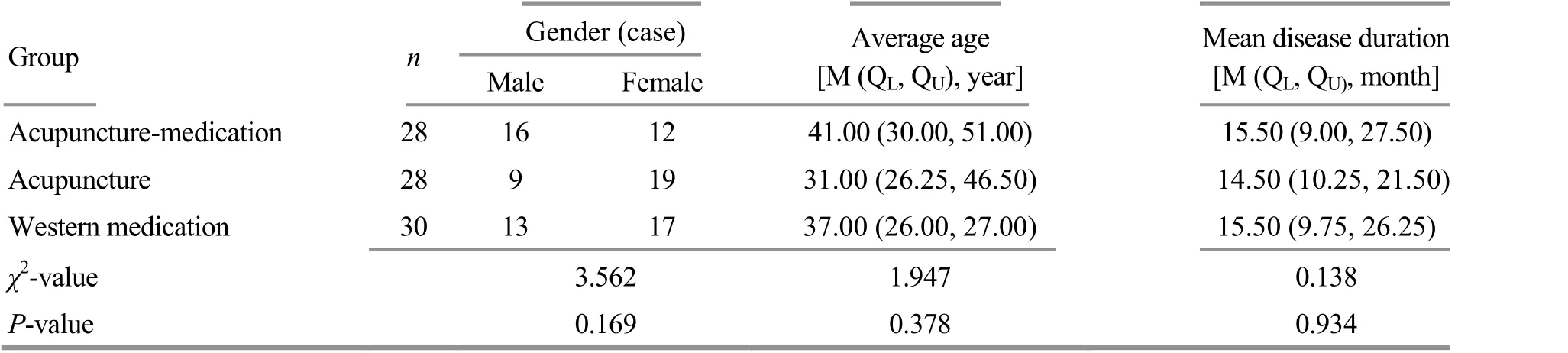
Table 1. Comparison of the general data
2 Treatment Methods
2.1 Acupuncture-medication group
2.1.1 Acupuncture treatment
Acupuncture, cupping therapy and collateral-pricking bloodletting therapy were used in the acupuncturemedication group.
Acupoints: Quchi (LI 11), Waiguan (TE 5), Xuehai(SP 10), Zusanli (ST 36), Sanyinjiao (SP 6), Zhongwan(CV 12), Tianshu (ST 25), Guanyuan (CV 4), Shenque(CV 8) and Geshu (BL 17).
Operation: After standard sterilization, Tony brand filiform acupuncture needles (Hwato Medical Equipment Co., Ltd., China) of 0.25 mm in diameter and 40 mm in length were inserted into Quchi (LI 11),Waiguan (TE 5), Xuehai (SP 10), Zusanli (ST 36),Sanyinjiao (SP 6), Zhongwan (CV 12), Tianshu (ST 25)and Guanyuan(CV4).The insertion directionand depth referred to the Meridian and AcupointScience[12]. The needles were retained for 20 min. Following acupuncture treatment, cupping was performed at Shenque (CV 8) and the cup was retained for 5 min. In the end, bilateral Geshu (BL 17) were treated with plum-blossom needle till there bled slightly, followed by cupping at the local areas with the cups retained for 5 min.
The treatment was performed once every other day,3 times a week, for 6 weeks in total.
2.1.2 Medication
Oral cetirizine hydrochloride tablets (specification No.:H19980014, Suzhou Dawnrays Pharmaceutical Co., Ltd.,China), 10 mg each time, once a day, for 6 weeks in total.
2.2 Acupuncture group
Same acupuncture, cupping therapy and collateralpricking bloodletting therapy as in the acupuncturemedication group were used in the acupuncture group,adopting the same acupoint selection, operation and treatment course.
2.3 Western medication group
The Western medication group only took cetirizine hydrochloride tablets of the same specification as in the acupuncture-medication group, following the same dosage and treatment course.
3 Observation of Therapeutic Efficacy
3.1 Observation items
3.1.1 Clinical symptom scores
The clinical symptom scoring criteria were based on the Guiding Principles for Clinical Study of New Chinese Medicines[13]. The observed symptoms included itching,the size of the biggest wheal, the number of wheals,influence on sleep and daily life, and duration of attack.The clinical symptoms were scored at a 0-3-point scale and recorded before and after 6-week treatment. The total clinical symptom score was the sum of the scores of the above 5 symptoms.
Itching: No symptom, 0 point; mild and not irritating,1 point; moderate but tolerable, 2 points; severe and unendurable, 3 points.
Size of the biggest wheal: No wheal, 0 point; the diameter of wheal ≤1.5 cm, 1 point; the diameter of wheal between 1.5 cm and 2.5 cm, 2 points; the diameter of wheal ≥2.5 cm, 3 points.
Number of wheals: No wheal, 0 point; 1-6 wheals,1 point; 7-12 wheals, 2 points; over 12 wheals, 3 points.
Influence on sleep and daily life: No influence, 0 point;mild and not interfering, sufficient sleep, and not affecting daily life, 1 point; moderate, slightly disturbing sleep, prolonged sleep latency, early awakening and slightly affected daily activities, 2 points; severe,significantly disturbed sleep, poor sleep quality,frequent awakenings, notably affected daily life, or even unable to maintain normal activities, 3 points.
Duration of attack: No attack, 0 point; duration <1 h,1 point; duration ≥1 h, but ≤12 h, 2 points; duration>12 h, 3 points.
3.1.2 Serum indicators
Enzyme-linked immunosorbent assay (ELISA) was used to detect the serum contents of IgE, INF-γ and IL-4.
Before and after 6-week treatment, 5 mL venous blood was collected using the anti-coagulation vacuum blood collection tubes. After standing by at room temperature for 30 min, the blood samples were centrifuged at 3 000 r/min for 10 min. The serum was taken and split charging at one serve and stored at-80 ℃. The detection was conducted within 6 months and repeated freeze-thaw was avoided during storage.The serum indicators were detected by professionals strictly following the instructions.
3.2 Evaluation criteria of clinical efficacy
The clinical efficacy was judged based on the 4-level efficacy evaluation method for chronic urticaria in the China Clinical Dermatology[14]and the symptom score ratio. The symptom score ratio = (Pre-treatment score -Post-treatment score) ÷ Pre-treatment score × 100%.
Cured: The symptom score ratio ≥90%; and the symptoms were basically gone.
Markedly effective: The symptom score ratio ≥60%but <90%, and the symptoms were notably mitigated.
Effective: The symptom score ratio ≥20% but <60%,and the symptoms showed certain improvements.
Invalid: The symptom score ratio <20%, and the symptoms presented insignificant changes.
3.3 Results
3.3.1 Comparison of clinical efficacy
After treatment, the total effective rate was 85.7% in the acupuncture-medication group, 82.1% in the acupuncture group and 83.3% in the Western medication group, and the inter-group differences were statistically insignificant (P>0.05). The cured and markedly-effective rate was significantly higher in the acupuncture-medication group than in the Western medication group (P<0.05), (Table 2)
3.3.2 Comparison of the clinical symptom score
After treatment, the total clinical symptom score declined significantly in all three groups (all P<0.05). The post-treatment change in the total clinical symptom score was more significant in the acupuncturemedication group than that in the Western medication group (P<0.05), (Table 3).
After treatment, the component symptom scores dropped significantly in all three groups (P<0.05). The post-treatment changes in the scores of itching, the size of the biggest wheal and the number of wheals were more significant in the acupuncture-medication group than in the Western medication group (all P<0.05); the post-treatment change in the score of the size of the biggest wheal was more significant in the acupuncture group than that in the Western medication group(P<0.01), (Table 4).
3.3.3 Comparison of the serum indicators
The contents of IgE and IL-4 decreased (all P<0.05)and the content of IFN-γ increased (all P<0.05) after treatment in the three groups. The post-treatment changes in the contents of IgE and IFN-γ were more significant in the acupuncture-medication group than those in the Western medication group (both P<0.05),(Table 5).
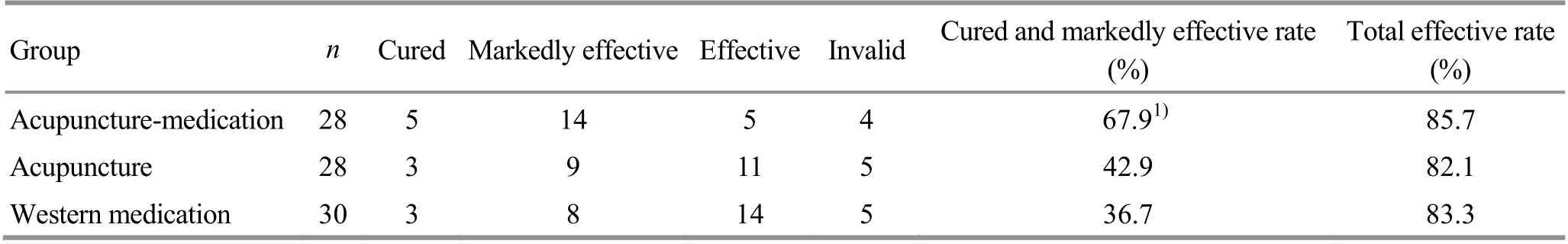
Table 2. Comparison of clinical efficacy (case)
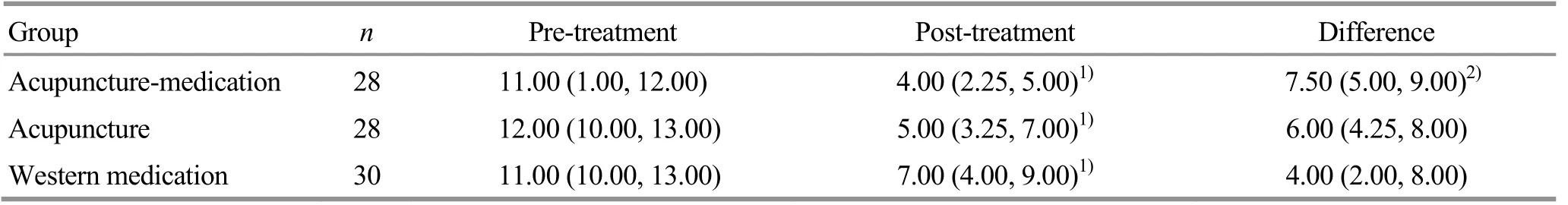
Table 3. Comparison of the total clinical symptom score [M (QL, QU), point]
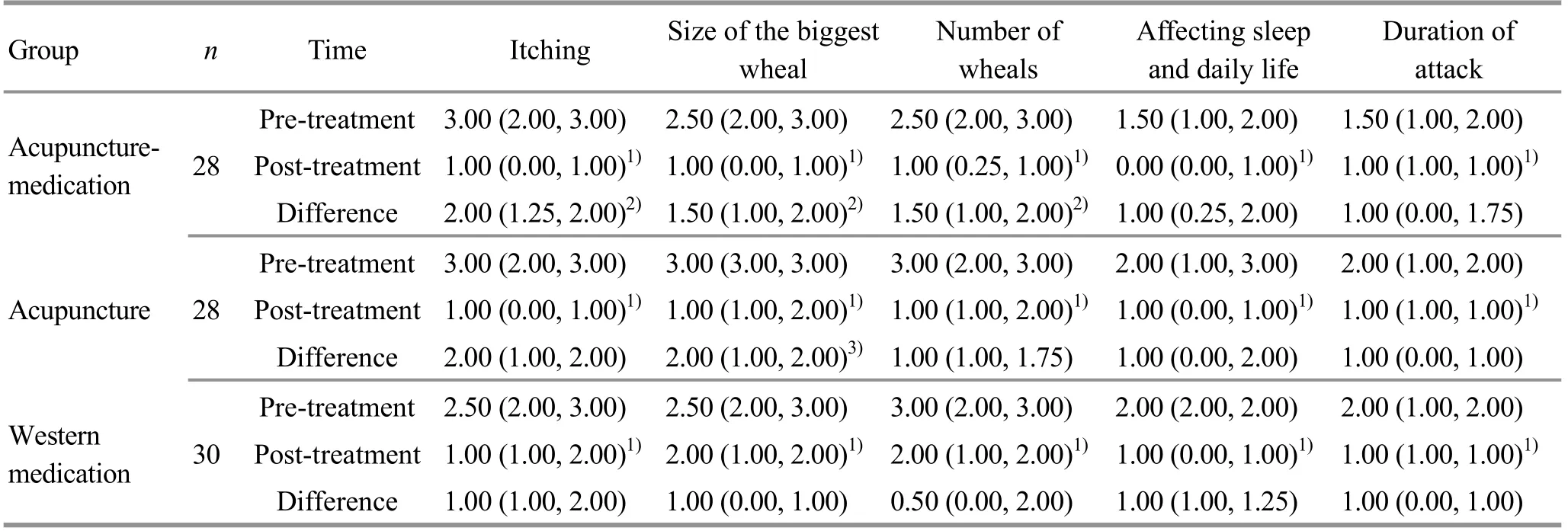
Table 4. Comparison of the component symptom scores [M (QL, QU), point]
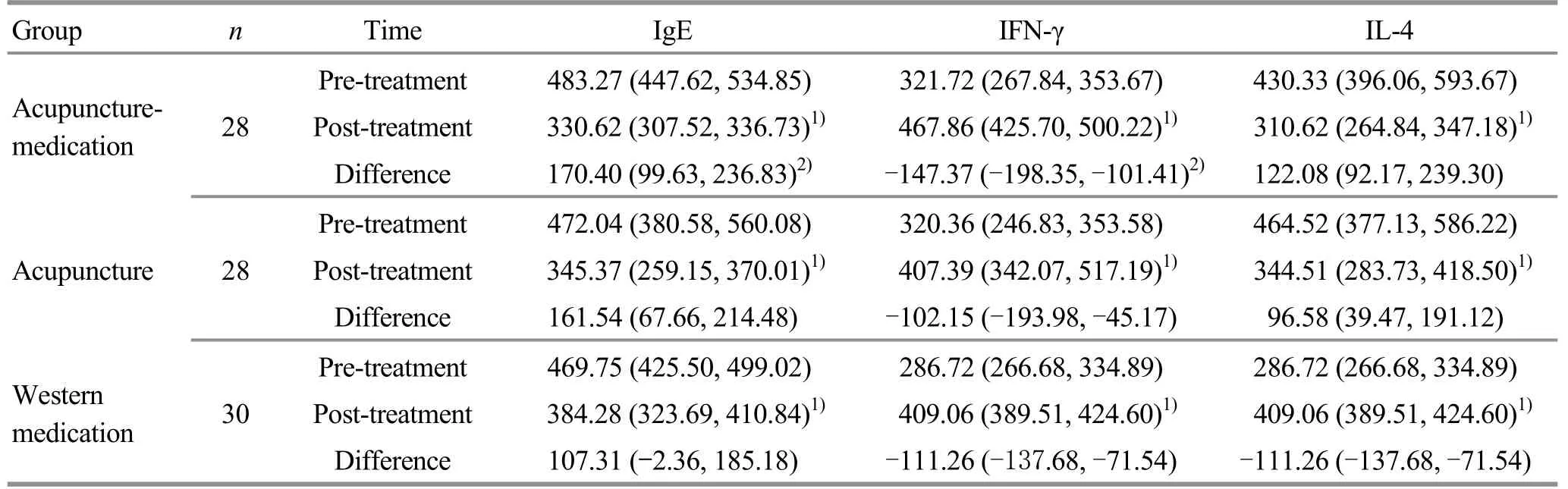
Table 5. Comparison of the serum indicators [M (QL, QU), ug/L]
3.3.4 Comparison of the incidence rates of adverse reactions and relapse rate
There occurred 2 cases of hematioma in the acupuncture group (accounting for 7.1%) during the study, which were mitigated by cold compress. The acupuncture-medication group had 3 cases of adverse reactions (accounting for 10.7%), including 2 cases of hematoma which were mitigated by cold compress and 1 case of digestive dysfunction which improved after 1-day rest. There were 11 cases of adverse reactions in the Western medication group (accounting for 36.7%),including 8 cases of digestive dysfunction which improved after rest and 3 cases of somnolence in the beginning of the study induced by medication which improved after adaption. The incidence rate of adverse reactions was significantly lower in the acupuncture group and the acupuncture-medication group than in the Western medication group (both P<0.05), and the difference between the acupuncture group and the acupuncture-medication group was statistically insignificant (P>0.05).
The 4-week follow-up studied the relapse rate in the cured and markedly effective cases. Of the 12 cases in the acupuncture group, 4 cases showed relapse,accounting for 33.3%; of the 19 cases in the acupuncture-medication group, 1 case had relapse,accounting for 5.3%; of the 11 cases in the Western medication group, 5 cases had relapse, accounting for 45.5%. The relapse rate was significantly lower in the acupuncture-medication group than in the Western medication group (P<0.05).
4 Discussion
TCM holds that in addition to exogenous factors,inborn endowment should be the main internal cause of chronic urticaria, which is like the effect of independent humoral immunity on urticaria in modern medicine. The chapter Wai Ke Xin Fa Yao Jue from Yi Zong Jin Jian (Essential Teachings on External Medicine of Golden Mirror of the Medical Tradition)[15]states that this disease is known as Gui Fan Ge Da (lumps caused by evil spirits) among the people, and usually occurs in people of exterior deficiency when contracting cold or wind, presenting itching skin followed by patches of bean-shaped lumps. It reflects the saying in TCM that‘the body won’t be affected by the external pathogens when there is sufficient healthy qi’. On the contrary, the body won’t be able to fight against external pathogens when the body is weak, and then urticaria will occur.
Western medicine mainly uses antihistamines,glucocorticoids, and epinephrine, etc. to treat chronic urticaria.
Antihistamines are the first-line drugs in the treatment of urticaria and are the most widely used.Cetirizine hydrochloride is the first choice of best-selling anti-allergic drugs[16]among second-generation antihistamines, with a positive effect and strong generalization. It has been widely used in clinical practice. However, some scholars have pointed out that antihistamines may cause different degrees of adverse reactions. Xu T, et al[17]analyzed the adverse reactions of second-generation antihistamines reported during 1986 and 2006. Among them, adverse reactions affecting the cardiovascular system and skin and its accessories, and systemic adverse reactions ranked the top three, accounting for 22.69%, 28.13%, and 15.69%,respectively. Numerous reports also pointed out that antihistamines may cause drug rash[18], anaphylactic shock[19], acute severe drug-induced hepatitis[20], and leukocytopenia[21], etc. In addition, chronic urticaria is a chronic disease that requires long-term medication,which may lead to drug resistance. Due to the existing side effects, long-term medication induces considerable stress in many urticaria patients so that they may not take medications as required. Long XY, et al[22]found that a poor compliance would hinder the clinical efficacy of the drug. Considering all the problems in the treatment of urticaria with Western medicine, it is urgent to find a safer and more effective treatment method. The current study demonstrated that acupuncture-moxibustion produced a positive effect in treating chronic urticaria and the adverse reactions were less common compared with Western medication.
Acupuncture-moxibustion treatment of urticaria can trace back to Zhen Jiu Jia Yi Jing (A-B Classic of Acupuncture and Moxibustion)[23]where it states that Tiantu (CV 22) can be used to treat hives coupled with headache, red hot skin and numb muscles. Bian Que Shen Ying Zhen Jiu Yu Long Jing (Bian Que’s Jade Dragon Classics of Acupuncture and Moxibustion)[24]discusses acupoint selection, recording that wind toxin-caused hives with itching and wounds due to scratching should be treated with Quchi (LI 11, using moxibustion and acupuncture with reducing manipulations), Xuanzhong(GB 39, using moxibustion and acupuncture with reducing manipulations) and Weizhong (BL 40, using bloodletting method). The commonly used acupoints for the treatment of chronic urticaria mainly include Quchi (LI 11), Hegu (LI 4), Fengchi (GB 20), Xuehai(SP 10), Sanyinjiao (SP 6), Zusanli (ST 36), Dazhui (GV 14),Feishu (BL 13), Xinshu (BL 15), Geshu (BL 17), and Pishu(BL 20), etc. Tianshu (ST 25) can be added for heat retained in the stomach and intestine; Neiguan (PC 6)can be added for nausea or vomiting; Shenmen (HT 7)and Yintang (GV 20) can be added for insomnia and restlessness; Qihai (CV 6) and Guanyuan (CV 4) can be added for deficiency of qi and blood. Acupoints can also be selected based on body regions, e.g., Quchi (LI 11),Hegu (LI 4) and Waiguan (TE 5) can be selected when the upper limbs are affected, and Xuehai (SP 10),Zusanli (ST 36) and Sanyinjiao (SP 6) can be used when the lower limbs are affected.
Itching is the most common reason for a patient with chronic urticaria to visit hospital and mitigating itching is the basic requirement for the treatment. The results showed that the three methods observed in this trial all could improve the itching symptom, and acupuncturemedication was superior to Western medication. The release of histamine is the main cause of itching, and the use of antihistamine drugs can directly improve this symptom. The advantage of acupuncture-medication shown in improving itching symptom indicated that acupuncture could down-regulate the content of histamine in treating chronic urticaria. Wheal is the manifestation of urticaria on the skin. It can reflect the severity of urticaria and affect the appearance and emotion of the patients. The clinical analysis demonstrated that all the three treatments can reduce the number and the size of wheals, and the improvements were more significant in the acupuncture-medication group than in the Western medication group. The change in physical symptoms is the basic requirement for treatment, while the improvement in psychosomatic symptoms is the high-level target. O'Donnell BF, et al[25]conducted a questionnaire survey among patients with chronic urticaria and patients with heart diseases, finding that patients with chronic urticaria got similar score in work ability and emotions compared with those with ischemic heart disease, and patients with urticaria got a higher score in sleep disturbance compared with those with heart diseases. It is indicated that chronic urticaria patients are suffering a lot in sleep and daily life,deserving more attention in modern medicine. Our study showed that all the three methods can improve patients’ sleep and daily life, but the inter-group differences comparing the improvement were statistically insignificant, which made it difficult to say which method works better in improving these two aspects.
Serum IgE plays a key role in type Ⅰhypersensitivity[26]. The IgE content is at a very low level in normal human body and usually only increases when stimulated by external allergens. Most chronic urticaria patients do have a higher IgE level, which makes the change of IgE content a biochemical indicator in evaluating the symptoms of urticaria. In this clinical trial,it was found that the serum IgE content decreased after treatment in the three groups, and the improvement was more significant in the acupuncture-medication group than in the Western medication group. Therefore,we should use acupuncture and medication together to down-regulate the serum IgE content in chronic urticaria rather than use Western medication alone.
B cells can secrete IgE under the induction of IL-4 and IFN-γ can inhibit the secretion of IgE, so the imbalance of the ratio of IFN-γ to IL-4 may be an important cause of abnormal IgE level. IFN-γ secreted by Th1 cells can promote the differentiation of Th cells into Th1 cells,meanwhile, IL-4 secreted by Th2 cells can promote the differentiation of Th cells into Th2 cells[27]. It can be found that there exists a cross-regulating effect among these factors. This clinical study showed that the IFN-γ content increased while the content of IL-4 decreased after treatment in all three groups, resulting in a higher ratio of IFN-γ/IL-4, indicating that acupuncture can improve the imbalance of Th1/Th2 cell function in the patients. When the disease onsets, the Th2 response is dominant, and after treatment, it is more inclined to Th1, so that the Th1/Th2 imbalance can be corrected.The improvement of the serum IFN-γ content was more significant in the acupuncture-medication group than in the Western medication group, but the between-group difference comparing the improvement of IL-4 was statistically insignificant. Although it is hard to judge which group works better in improving the IL-4 content,the acupuncture-medication group obtained better result comparing the improvement of the ratio of IFN-γ/IL-4, suggesting that the acupuncture-medication group had advantage in regulating Th1/Th2.
Based on the above conclusions, we can see that the acupuncture-medication group produced better results in improving the clinical symptoms and blood indexes in chronic urticaria compared with the Western medication group. However, the differences between the acupuncture group and the Western medication group were insignificant. This may be due to the differentiation of action pathways between acupuncture and antihistamine drugs. There are many transmitters involved in itching skin. In addition to histamine, there are also serotonin, acetylcholine,bradykinin, substance P, prostaglandin, interleukins,opioid peptides, etc. The pathogenesis of different types of pruritic diseases involves different transmitters.Even for the same disease, there may be differences amongst different subtypes[28]. The current trial did not classify the recruited cases, where may exist differences in the transmitters between the acupuncture group and the acupuncture-medication group or the Western medication group. Furthermore, the small sample size in this study may be a factor leading to bias in the results. These issues should be addressed in the future by expanding the sample size and designing subgroups based on different types of chronic urticaria.
In short, although this study failed to explain the specific effect of acupuncture in treating chronic urticaria, it approved the efficacy of acupuncture in combination with medication. The results also showed that acupuncture-medication can effectively regulate the imbalance of Th1/Th2 and down-regulate the level of serum IgE, better than Western medication alone.Therefore, this integrative method is worth promoting in clinical practice.
Conflict of Interest
The authors declare that there is no potential conflict of interest in this article.
Acknowledgments
This work was supported by Science Project of Shanghai Health Bureau (上海市卫生局科研课题, No. 20124046);Science Project of Shanghai Municipal Health and Family Planning Commission (上海市卫生和计划生育委员会科研课题, No. 201640214).
Statement of Informed Consent
Informed consent was obtained from the patients in this study.
Received: 1 July 2019/Accepted: 15 August 2019
猜你喜欢
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Therapeutic observation of ‘warming-unblocking needling technique’ for knee osteoarthritis due to deficiency of liver and kidney
- Therapeutic observation of arthrolysis under brachial plexus anesthesia for adhesive capsulitis of the shoulder
- Clinical study of thumb-tack needle therapy for cervical radiculopathy based on meridian differentiation
- Clinical observation of acupuncture plus repetitive transcranial magnetic stimulation in the treatment of post-stroke insomnia
- Clinical observation on prevention of chemotherapy infection in gastric cancer by moxa-stick moxibustion plus rhG-CSF and its effect on immune function
- Clinical observation of deep electroacupuncture at Baliao points for female stress urinary incontinence