冠状动脉旁路移植术与药物洗脱支架治疗无保护左主干冠心病疗效比较
2017-09-03周保国王兆东王静王丽君吕洪福李珂
周保国 王兆东 王静 王丽君 吕洪福 李珂
(1.青岛阜外心血管病医院心脏外科,山东青岛 266034;2.山东青岛思达心脏医院心脏外科,山东青岛 266000)
冠状动脉旁路移植术与药物洗脱支架治疗无保护左主干冠心病疗效比较
周保国1王兆东2王静1王丽君1吕洪福1李珂1
(1.青岛阜外心血管病医院心脏外科,山东青岛 266034;2.山东青岛思达心脏医院心脏外科,山东青岛 266000)
目的:探讨无保护左主干病变患者选用冠状动脉旁路移植术与药物洗脱支架治疗的疗效。方法:选择100例在我院行血运重建术的无保护左主干患者,根据患者选择的手术方式不同随机分为两组:A组(药物洗脱支架组,n=48例)、B组(冠状动脉旁路移植术组,n=52例)。统计两组患者一般情况、心功能指标、冠状动脉病变特点、住院期间疗效及术后3年不良心脑血管事件的发生率。结果:两组患者左主干病变的主要位置位于开口部和体部,A组患者左主干+多支血管病变的发生率及Syntax积分明显低于B组,差异有统计学意义;A组患者术后平均住院天数明显低于B组患者,差异有统计学意义,血运完全重建人数低于B组患者,差异有统计学意义,两组患者住院期间总死亡人数相比差异无统计学意义;术后3年两组患者心脑血管事件总人数、总死亡人数、脑卒中、非致死性心肌梗死的发生情况相比差异无统计学意义,A组患者靶血管再次血运重建的发生率明显高于B组患者,差异有统计学意义。结论:无保护左主干病变患者采用药物洗脱支架治疗方法可减少患者围术期的住院时间且不增加患者心脑血管事件的发生及死亡率,但与冠状动脉旁路移植术相比会增加患者远期靶血管再次血运重建。
冠心病;无保护左主干;药物洗脱支架;冠状动脉旁路移植术
心脏左主干主要供应左心室的血液[1-2],因而左主干病变患者是冠状动脉粥样硬化性心脏病中的高危人群。无保护的左主干病变患者由于缺少侧支循环,死亡风险更高[3-4],一旦血流改变可能立刻引起患者心源性休克甚至死亡[5]。冠状动脉旁路移植术是治疗无保护左主干病变的主要方法,可以明显改善患者的生存率[6-7]。随着冠状动脉介入手术的成熟和药物洗脱支架的研发,药物洗脱支架植入成为左主干病变血运重建的新方法[8]。因而本研究将探讨无保护左主干病变患者选用冠状动脉旁路移植术与药物洗脱支架治疗的近远期疗效。
1 资料与方法
1.1 一般资料
选择于我院行血运重建术的无保护左主干患者100例,排除急性心肌梗死、其它原因所致左主干病变者,再次血运重建患者、既往有冠状动脉旁路移植术手术史、术后不能长期耐受抗血小板药物治疗等患者。所有患者术前均行冠状动脉造影确诊为左主干病变(狭窄程度≥50%且左前降支或回旋支无侧支循环及血管桥),随机并根据患者意愿选择手术方式。两组分别为:A组(药物洗脱支架组,n=48例)、B组(冠状动脉旁路移植术组,n=52例)。本研究经我院伦理委员会批准且所有患者均签署知情同意书。
1.2 方法
A组患者术前一周开始采用阿司匹林肠溶片300mg/天、氯吡格雷75mg/天口服,术中根据患者情况选择桡动脉或股动脉穿刺行药物洗脱支架置入术,对于左主干远端分叉无病变的患者采用单支架置入术,合并远端分叉病变的患者采用双支架置入术,术后阿司匹林肠溶片改为100mg/天长期服用,氯吡格雷75mg/天服用一年。B组患者术前一周停用阿司匹林肠溶片、氯吡格雷等药物,改为低分子肝素40~60mg/次,2次/天,皮下注射,术中据情况采用体外循环或非体外循环下冠状动脉旁路移植术,术后长期口服阿司匹林肠溶片100mg/天。两组患者术后据情况加用调脂(阿托伐他汀钙片或瑞舒伐他汀钙)、改善循环(硝酸酯类)、降压药物。
1.3 观察指标
统计两组患者一般情况、心功能指标、冠状动脉病变特点、住院期间疗效及术后3年不良心脑血管事件(总死亡人数、脑卒中、非致死性心肌梗死、靶血管再次血运重建)的发生率。Syntax评分指标具体如下:syntax评分系统将冠状动脉分为16段,对直径≥1.5mm,狭窄程度≥50%的冠脉血管进行评分主要包括冠状动脉优势分布类型、病变血管数目、病变节段及特征等,所得的总分即为Syntax总分。采用SPSS19.0统计学软件进行统计学分析,P<0.05为差异有统计学意义。
2 结果
两组患者年龄、性别比、高血压病史、糖尿病病史、高脂血症病史、吸烟史、心功能指标相比差异无统计学意义。
患者左主干病变的主要位置位于开口部和体部,A组患者左主干+多支血管病变的发生率及Syntax积分明显低于B组,差异有统计学意义,见表1。
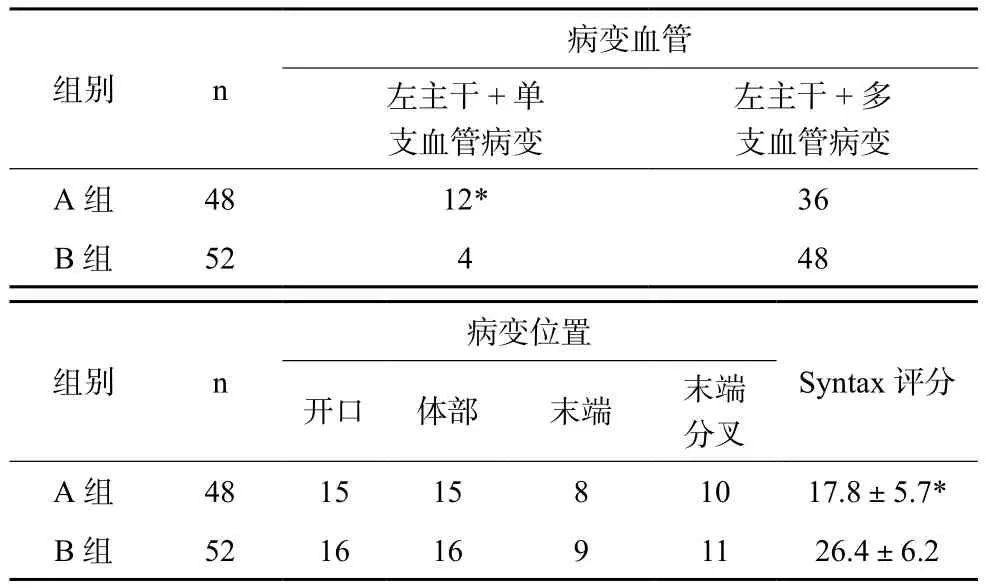
表1 两组患者冠状动脉病变特点比较
A组患者术后平均住院天数(4.5±1.9)天,明显低于B组的(15.8±6.7)天,差异有统计学意义,P<0.05,两组血运完全重建人数38vs49,死亡人数0vs3,A组完全重建人数低于B组,差异有统计学意义,P<0.05;死亡率比较差异无统计学意义。
术后随访3年不良心脑血管事件的发生情况,两组心脑血管事件总人数相比差异无统计学意义,其中总死亡人数、脑卒中、非致死性心肌梗死的发生情况相比差异无统计学意义,P>0.05,A组患者靶血管再次血运重建的发生率18.75%明显高于B组患者的3.85%,差异有统计学意义,P<0.05。
3 讨论
左冠状动脉是供应左心血供的主要动脉,病变率约为5%,患者极易出现心律失常、心肌梗死、心源性休克等危及生命的并发症,早期诊断治疗无保护左主干病变可以明显改善患者预后[9-11]。有研究表明冠状动脉旁路移植术可明显改善无保护左主干患者的生存率[12],且患者无主要心血管事件生存率明显高于冠状动脉支架置入术,因而冠脉旁路移植术是无保护左主干患者首选治疗方案。但冠状动脉粥样硬化的患者多为中老年患者,且多合并糖尿病、心功能不全、外周血管疾病等,外科手术创伤及术后并发症也成为患者中远期生存率的影响因素[13-14]。也有研究表明无保护左主干患者采用介入手术治疗也可获得较高的生存率[15],但合并多血管病变的PCI手术难度较大,因而对于左主干多血管病变的处理策略选择更应慎重。
本研究中, A组患者多为左主干+单支血管病变,因而其Syntax评分低于B组。A组患者术后平均住院天数明显低于B组患者,差异有统计学意义,表明药物洗脱支架置入术创伤小,术后患者恢复快。两组患者住院期间总死亡人数相比差异无统计学意义,表明药物洗脱支架置入术安全性高,并不增加患者围术期的死亡率。A组患者血运完全重建人数低于B组患者,这可能和术中操作有关,由于药物洗脱支架置入术要求冠脉造影清楚显示病变血管、支架能够尽可能伸展、贴合覆盖病变血管,但术中支架置入和释放均在透视下进行,因而可能存在操作上的误差[16]。术后3年随访结果表明术后血管再狭窄是影响药物洗脱支架疗效的重要因素,其可能的机制和血管重塑、血管弹性回缩、血管内血栓及新生内膜增生形成有关,同时糖尿病、高脂血症、急性心肌梗死等也可导致介入手术数周后支架内再狭窄。再次血运重建的血管不仅包括既往的病变血管也包括新狭窄的病变血管,因而病变的新进展和新发病变是限制药物洗脱支架治疗远期效果的重要原因,控制冠状动脉粥样硬化的危险因素,调整患者的血糖、血压、血脂可能有效降低远期血管再次血运重建的发生率[17-18]。以上研究结果可以看出药物洗脱支架治疗具有创伤小、患者住院时间短、术后恢复快等优点,降低其再狭窄率可显著提高其远期疗效。冠状动脉旁路移植术虽然完全血运重建率高,但创伤大、患者围术期并发症、死亡率高。因而对于无保护左主干病变患者的手术方式应具体化、个体化。
[1] QARAWANI D, MENACHEM N, GANEM D, et al. Unprotected left main stenting, short and long-term outcomes[J]. Acute Care Care, 2010,12(4):124-129.
[2] SANJAY P, YOUNG HK, SHERIDAN M. Drug-eluting versus baremetal stents in unprotected left main coronary artery stenosis[J]. JACC, 2010,3(6):602-611.
[3] ALDEA GS, MOKADAM NA, MELFORD R, et al. Changing volumes, risk profiles, and outcomes of coronary interventions[J]. Ann Thorac Surg, 2009,87(6):1828-1838.
[4] ZHENG S, ZHENG Z, HOU J, et al. Comparison between drug-eluting stents and coronary artery bypass grafting unprotected left main coronary artery disease: a meta-analysis of two randomized trials and thirteen boservational studies[J]. Cardiology, 2011,118(8):22-32.
[5] PARK DW, KIM YH, YUN SC, et al. Long-term outcomes after stenting versus coronary artery bypass grafting for unprotected left main coronary artery disease:10-year results of bare-metal stents and 5-year results of drug-eluting stents from the ASANMAIN Registry[J]. J Am Coll Cardiol, 2010,56(5):1366-1357.
[6] BIRIM O, GAMERON M, BOGERS AJ, et al. Complexity of coronary vasculature predicts outcome of surgery for left main disease[J]. Am Thorac Surg, 2009,87(7):1097-1104.
[7] SERRUYS PW, MORICE MC, KAPPETEIN AP, et al. Percutaneous coronary intervention versus coronary artery bypass grafting for severe coronary artery disease[J].N Engl J Med, 2009,360(12):961-972.
[8] LEMESLE G, BONENOL L, LABRONE A, et al. Prognostic value of the SYNTAX score in patients undergoing coronary artery bypass grafting for three-vessel coronary artery disease[J]. Catheter Cardiovasc Interv, 2009,73(9):612-617.
[9] DAWKINS KD, MOREL MA, SERRUYS PW. Counting the score: the SYNTAX score and coronary risk[K]. Euro Intervention, 2009,5(2):33-35.
[10] PALMERINI T, BARLOCCO F, SANTARELLI A, et al. A comparision between coronary artery bypass grafting surgery and drug eluting stent for the treatment of unprotected left main coronary artery disease in elderly patients(aged>or=75years). Eur Heart J, 2007,28(5):2714-2719.
[11] LEE SW, KIM SH, KIM SO, et al. Comparative long-term efficacy and safety of drug-eluting stent versus coronary artery bypass grafting in ostial left main coronary artery disease: analysis of the main compare registry[J].Catheter Cardiovasc Interv, 2012, 80(2):206-212.
[12] MORICE M, SERRUYS PW, KAPPETEIN P, et al. Outcomes in patients with de novo left main disease treated with either percutaneous coronary intervention using paclitaxel-eluting stents or coronary intervention with TAXUS and cardiac surgery trial[J]. Circulation, 2010,121(24):2645-2653.
[13] BRENNAN JM, DAI D, PATEL MR, et al. Characteristics and long-term outcomes of percutaneous revascularization of unprotected left main coronary artery stenosis in the United States: a report from the national cardiovascular data registry, 2004 to 2008[J]. J Am Coll Cardiol, 2012,59(7):648-454.
[14] JIANG WB, ZHAO W, HUANG H, et al. Meta-analysis of effectiveness of first-generation drug-eluting stents versus coronary artery bypass grafting for unprotected left main coronary disease[J].Am J Cardil, 2012,110(12):1764-1772.
[15] WANG QS, TAN Q, LIU DT, et al. Clinical outcomes of trasradial unprotected left main coronary artery stenting in the elderly[J]. Saudi Med J, 2014,35(8):580-584.
[16] PARK DW, KIM YH, YUN SC, et al. Complexity of atherosclerotic coronary artery disease and long-term outcomes in patients with unprotected left main disease treated with drug eluting stents or coronary artery bypass grafting[J]. J Am Coll Cardiol, 2011,57(21):2152-2159.
[17] CHIEFFO A, MELIGA E, LATIB A, et al. Drug-eluting stent for left main coronary artery disease. The DELTA registry:a multicenter registry evaluating percutaneous coronary intervention versus coronary artery bypass grafting for left main treatment[J]. JACC Cardiovasc Interv, 2012,5(7):718-727.
[18] MIN SY, PARK DW, YUN SC, et al. Major predictors of longterm clinical outcomes after coronary revascularization in patients with unprotected left main coronary disease: analysis from the MAIN COMPARE study[J]. Circ Cardiovasc Interv, 2010,3(2):127-133.
The effect comparison between coronary artery bypass grafting and drug eluting stent on the treatment of unprotected left main coronary artery disease
ZHOU Baoguo1, WANG Zhaodong2, WANG Jing1, WANG Lijun1, LYU Hongfu1, LI Ke1.
(1. Department of Cardiac surgery,Qingdao Fuwai Cardiovascular Disease Hospital,Qingdao 266034 china;2. Department of Cardiac surgery,Qingdao starr heart hospital,Qingdao 266000,china)
Objective: The objective of this study was to compare the effect of coronary artery bypass grafting and drug eluting stent on the treatment of unprotected left main coronary artery disease. Methods: A total of 100 cases of patients with unprotected left main coronary artery disease applying revascularization treated in our hospital were randomly divided into group A ( drug eluting stent, n=48) and group B (coronary artery bypass grafting, n=52). The general conditions, cardiac parameters, coronary artery lesion characteristics, curative effect during hospitalization and the incidence of adverse cardiovascular and cerebrovascular events after 3 years of surgery were recorded. Results: The main sites of left main coronary artery disease of two groups were found in ostial and body. The incidence of left main coronary artery plus multi-vessel disease and Syntax score were remarkable lower than that of B group and the difference was statistically signif i cant; the average length of stay of A group was shorter than B group while the number of revascularization of group A was less than group B and the difference was statistically signif i cant. The difference of total death toll during hospitalization between two groups was not statistically signif i cant; the difference of the total number of cardiovascular and cerebrovascular events, total death toll, stroke and the incidence of non-lethal myocardial infarction between two groups after 3 years of treatment was of no statistical signif i cance. The incidence of target vessel revascularization of group A was higher than group B and the difference was statistically significant. Conclusions: The therapy of drug eluting stent on unprotected left main coronary artery disease can decrease the perioperative hospitalization time without adding the morality rate of cardiovascular and cerebrovascular events, however, it will increase the target vessel revascularization comparing with the coronary artery bypass grafting.
coronary heart disease; unprotected left main coronary artery; drug eluting stent; coronary artery bypass grafting
R654.3
A
2095-5200(2017)04-028-03
10.11876/mimt201704013
周保国,本科,主治医师,研究方向:心外疾病临床,Email:guobaozhou231@163.com。
