蛛网膜下腔出血患者头痛发作时经颅多普勒超声监测指标变化的临床研究
2017-08-26康志新
康志新
[摘要] 目的 鑒别蛛网膜下腔出血(SAH)患者头痛发作的病因,为患者提供及时有效的治疗指导方案。 方法 回顾性分析2010年5月~2013年12月入住中国石油天然气中心医院神经内科SAH患者61例临床资料。利用颅多普勒超声(TCD)监测SAH患者入院和头痛发作时大脑中动脉(MCA)、大脑后动脉(PCA)、椎基底动脉系统(BA)血流速度的变化,其中,符合脑血管痉挛(CVS)者为A组,不符合CVS为B组,比较两组TCD监测指标及治疗效果。 结果 A组患者78例次(53.8%),与入院时相比患者头痛发作时MCA、PCA、BA平均血流速度均增加,差异有统计学意义(P < 0.05),考虑为CVS所致,且给予及时有效的治疗方案,病情均得到缓解。B组患者67例次(46.2%),头痛发作时MCA、PCA、BA平均血流速度与入院时相比差异无统计学意义(P > 0.05),其中50例次(75%)患者给予减轻脑水肿治疗病情得到有效缓解。 结论 SAH患者TCD监测数据的变化为CVS诊断提供可靠依据。TCD实时监测对发现和鉴别CVS、脑水肿有重要的临床价值。
[关键词] 蛛网膜下腔出血;脑血管痉挛;脑水肿;经颅多普勒超声;尼莫通;甘露醇
[中图分类号] R743.35 [文献标识码] A [文章编号] 1673-7210(2017)07(b)-0094-04
A clinical study on changes of transcranial Doppler in patients with subarachnoid hemorrhage during headache attack
KANG Zhixin
Department of Internal Medicine, China Aviation Hospital, Beijing 100012, China
[Abstract] Objective To identify the etiology of headache in patients with subarachnoid hemorrhage, in order to provide timely and effective treatment guidelines for patients. Methods The clinical data of 61 patients with subarachnoid hemorrhage treated in Neurology Department of CNPC Central Hospital from May 2010 to December 2013 were analyzed retrospectively. TCD was used to monitor the changes of MCA, PCA and BA blood flow velocity in patients with subarachnoid hemorrhage during hospitalization and headache attack. According to the results of TCD, patients were divided into two groups. Patients in group A were corresponded to cerebral vasospasm, patients in group B were not corresponded to cerebral vasospasm. The TCD indexes and treatment effect of the two groups were compared. Results There were 78 case-times (53.8%) in group A. The MCA, PCA and BA blood flow velocity of patients at headache attack were increased than at hospitalization in group A, the differences were statistically significant (P < 0.05), and it was considered to be caused by cerebral vasospasm. All patients had remission after given timely and effective treatment. There were 67 case-times (46.2%) in group B. The differences of MCA, PCA and BA blood flow velocity between patients at hospitalization and headache attack in group B had no statistically significant (P > 0.05), and it was unrelated to cerebral vasospasm. 50 case-times (75%) of patients had remission after given alleviate cerebral edema treatment. Conclusion The changes of TCD monitoring data of SAH patients provide reliable evidences for cerebral vasopasm diagnosis. TCD real-time monitoring has important clinical value for finding and identifying cerebral vasopasm and cerebral edmema.
[Key words] Subarachnoid hemorrhage; Cerebral vasospasm; Brain edema; Transcranial Doppler; Nim; Mannitol
蛛网膜下腔出血(subarachnoid hemorrhage,SAH)通常指脑底部或脑表面的血管破裂后血液进入蛛网膜下腔所导致的一种临床综合征,是神经科常见的危重症之一,病死率高。头痛是SAH最常见的临床症状,发生率达85%~95%[1-3]。脑血管痉挛(cerebral vasopasm,CVS)、脑水肿是SAH后早期的最严重并发症,是SAH后残废和死亡的主要原因之一[4]。CVS和脑水肿常见的临床症状为难以忍受的剧烈头痛,而目前对于SAH患者头痛发作时的真正病因,尚无积极、有效、无创的判定手段。本研究采用经颅多普勒超声(transcranial doppler,TCD)实时监测SAH患者头痛发作时颅内大动脉血流速度,从而间接判断导致头痛的真正原因,为制订有效的治疗方案提供更多实验数据。
1 对象与方法
1.1 对象
回顾性分析2010年5月~2013年12月入住中国石油天然气中心医院神经内科的SAH患者61例,其中,男38例,女23例,平均年龄(60.7±10.14)岁。所有患者均具有典型的临床症状与体征,且均经颅脑CT检查确诊,符合1994年第4届全国脑血管学术会议制订的SAH诊断标准[5]。排除TCD检查无颞窗患者、昏迷患者、不能配合TCD检查患者。
1.2 方法
所有患者均于入院24 h内行首次TCD(第二代经颅多普勒仪,美国MEDASONICS公司)检查,头痛发作时随时行TCD检查。采用2 MHz脉冲波探头,主要经颞窗、眶窗、枕窗分别测定颅内动脉瘤好发部位Willis环附近大脑中动脉(MCA)、大脑后动脉(PCA)、基底动脉(BA)平均血流速度,探测深度为36~60 mm,由专门的医师进行TCD监测。
1.3 脑血管痉挛诊断标准
CVS诊断首先依靠临床症状,可出现头痛、血压升高、嗜睡、昏睡、昏迷、偏瘫等症状体征。TCD检查MCA可以评价脑血管痉挛的严重程度[6],也是最适合行TCD检查的动脉。TCD检查显示MCA平均血流速度>120 cm/s,PCA平均血流速度>90 cm/s,BA平均血流速度>60 cm/s可诊断为CVS。
1.4 统计学方法
采用SPSS 10.0统计学软件进行数据分析,计量资料数据用均数±标准差(x±s)表示,两组间比较采用t检验;以P < 0.05为差异有统计学意义。
2 结果
2.1 TCD监测数据分析
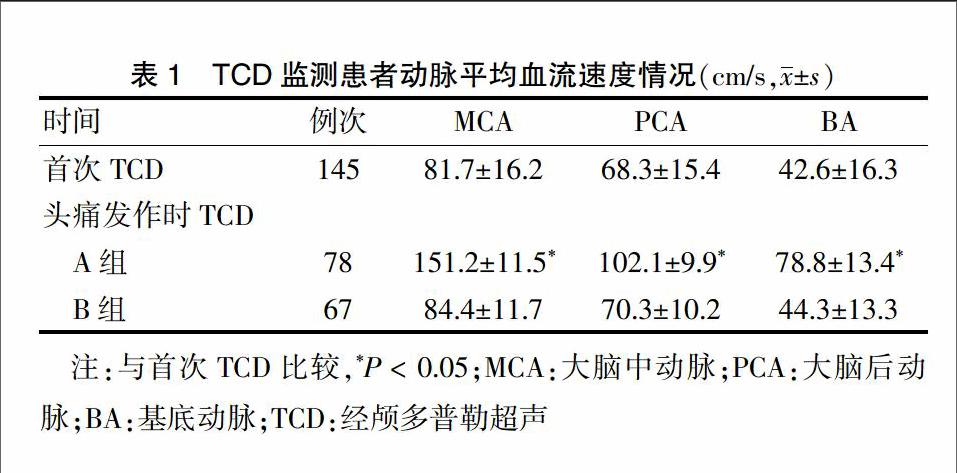
将头痛发作时TCD监测显示符合CVS者78例次(1例次为床旁TCD监测1次)设为A组,不符合CVS者67例次设为B组。与患者入院24 h内首次TCD检查的各指标数据比较,A组头痛发作时MCA、PCA、BA平均血流速度均升高,差异有统计学意义(P < 0.05);B组头痛发作时MCA、PCA、BA平均血流速度与入院时相比差异无统计学意义(P > 0.05)。见表1。
2.2 治疗效果
按照TCD监测结果,SAH患者头痛发作时符合CVS诊断标准者,给予增加尼莫地平静脉泵入速度[平均增加0.2 μg/(kg·min)],头痛可得到缓解。不符合CVS诊断标准者,50例次(75%)给予20%甘露醇250 mL于40 min内静脉滴注,降颅压后头痛得以缓解;余17例次(25%)需要联合加巴喷丁后,头痛方可缓解。未见药物不良反应。
3 讨论
SAH是急性出血性腦血管病,其常见病因为颅内动脉瘤、脑动脉畸形、高血压动脉硬化症、血液疾病等。SAH占急性脑卒中的10%左右,占急性出血性脑卒中的20%,多于情绪激动或过度用力时出现剧烈头痛,此症状是SAH患者的主要痛苦,而难以忍受的剧烈头痛常使患者烦躁不安,加重高颅压甚至诱发再出血,导致患者病死率和致残率增加。SAH时引起剧烈头痛的原因[7-8]可能有以下几点:①颅压的增高;②血液进入脑脊液直接刺激硬脑膜、蛛网膜等;③红细胞破裂释放出5-羟色胺、儿茶酚胺、花生四烯酸、游离激肽等活性物质刺激硬脑膜、蛛网膜等;④红细胞分解的产物或释放的物质刺激所接触血管而引起脑血管痉挛。以上导致头痛的病因中,脑血管痉挛、颅内压增高、脑水肿所致的脑组织损害是SAH患者致死、致残的主要原因之一。能够准确及时判定SAH患者头痛发作的确切原因,并予以及时有效的治疗,是目前临床上亟待解决的问题。
TCD是一种无创性的监测方法,可根据其所监测血管的血流速度、相关指数及血流频谱的变化对SAH患者脑血管痉挛、脑水肿进行动态监测与评估,从而达到床旁实时监测颅内压、颅内动脉血流、CVS等改变的目的,实现实时调整治疗方案,有效缓解病情及降低SAH患者的致残、致死率。美国心脏协会(AHA)/美国卒中协会(ASA)指南[9]及欧洲指南[10]中,已经将TCD作为SAH后发生血管痉挛的常规监测工具。无创性的TCD监测不仅能反映颅内血流动力学变化,也可反映颅内压(ICP)的变化,还能通过TCD所监测的PI值预测脑出血6个月后的预后恢复情况[11]。
临床上,SAH后导致的头痛病因中,可控可治且危及患者生命的为CVS和脑水肿。其中,SAH后CVS是一种复杂的临床综合征,其发生已严重威胁到患者的生命,以往的实验均证实CVS是SAH严重的并发症之一,常引发缺血性脑损害,甚至导致脑梗死,发生率达到30%以上[12],成为SAH患者致残致死的关键因素。数字减影血管造影(DSA)一直作为判断SAH后CVS的“金标准”[13],其最大优点是能准确识别痉挛的血管,并阐明神经功能状况的恶化原因,有确诊价值。但DSA是有创的,且不能在床边即刻实时展开,而TCD弥补了这一缺陷,作为一种无创检查,TCD可以在床边施行,用来随时监测患者颅内血流速度,尤其对大脑中动脉血流速度非常敏感,对血管痉挛有一定的提示作用[14-16]。
本研究采用床旁TCD實时为SAH患者头痛发作时监测颅内动脉的血流速度,与CVS患者入院时比较,差异有统计学意义(P < 0.05);对脑血流的监测使患者得到个性化治疗,避免所有的SAH患者头痛发作时都加量尼莫地平,也避免了CVS引起局部脑组织缺血性而导致的严重后果。SAH后高达17%~40%的患者因脑血管痉挛出现了迟发性缺血性的神经功能障碍[17],本组SAH头痛患者中出现CVS者占53.8%。目前认为,CVS发病机制为当细胞内钙离子浓度升高到一定水平时,平滑肌即刻发生收缩,导致其支配的血管痉挛[18]。
SAH后出现的脑水肿可分为血管源性脑水肿和细胞毒性脑水肿,在临床患者和动物实验中均已得以证实[19-20],两者同时存在,加重临床症状,严重的可致脑疝、脑死亡。经相关研究证实,前者是血脑屏障受损、破坏后的直接结果。由于出现血管内皮细胞和周围胶质细胞凋亡等一系列病理生理变化,致使毛细血管通透性增加,血管内水分渗出的增多,积存于血管周围及细胞间质,形成了脑水肿[21-23]。本研究中,患者头痛发作时,TCD监测未达到CVS诊断标准,但患者有明显颅高压,恶心、呕吐,给予甘露醇脱水降颅压后,75%患者头痛可及时缓解,但仍有25%患者需要联合增加止痛药物,头痛方可缓解。
综上所述,对于目前SAH所致的头痛病因诊断及下一步积极有效治疗方面尚无统一的标准及指南,本研究有望在SAH规范化治疗的基础上,通过实时TCD监测数据,及时有效减轻CVS和脑水肿带来的脑损伤,为将来制订个体化治疗积累临床资料。
[参考文献]
[1] Oeinck M,Neunhoeffer F,Buttler KJ,et al.Dynamic cerebral autoregulation in acute intracerebral hemorrhage [J]. Stroke,2013,44(10):2722-2728.
[2] Manawadu D,Jeerakathil T,Roy A,et al.Blood pressure management in acute intracerebal hemorrhage guidelines are poorly implemented in clinical practice [J]. Clin Neurol Neuosurg,2010,112(10): 858-864.
[3] Manno EM.Update on intracerebral hemorrhage [J]. Continuum(Minneap Minn),2012,18(3):598-610.
[4] 赵君,李兴强,苗素云.TCD动态监测尼莫地平防治蛛网膜下腔出血后脑血管痉挛中的临床观察[J].社区医学杂志,2007,5(13):22-23.
[5] 蒋雨平.临床神经疾病学[M].上海:上海医科大学出版社,1999:77.
[6] 赵冬,许晖,刘祺,等.持续腰大池引流对蛛网膜下腔出血脑血管痉挛的防治研究[J].实用心脑肺血管病杂志,2011,19(6):900-901.
[7] Wallace MS,Irving G,Cowles VE. Gabapentin extended-release tablets for the treatment of patients with postherpetic neuralgia:a randomized,double -blind,placebo-controlled,ulticentre study [J]. Clin Drug Investig,2010,30(11):765-776.
[8] Sun JL,Chiou JF,Lin CC. Validation of the Taiwanese version of the Athens Insomnia Scale and assessment of insomnia in Taiwanese cancer patients [J]. J Pain Symptom Management,2011,41(5):904-914.
[9] Connolly ES Jr,Rabinstein AA,Carhuapoma JR,et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage:A guideline for healthcare professionals from the american heart association/american stroke association[J]. Stroke,2012,43(6):1711-1737.
[10] Steiner T,Juvela S,Unterberg A,et al. European stroke organization guidelines for the management of intracranial aneurysms and subarachnoid haemorrhage [J]. Cerebrovasc Dis,2013,35(2):93-112.
[11] Kiphuth IC,Huttner HB,Drfler A,et al. Doppler pulsatility index in spontaneous intracerebral hemorrhage [J]. Eur Neurol,2013,70(3/4):133-138.
[12] Chen J,Chen G,Li J,et al. Melatonin attenuates inflammatory response-induced brain edema in early brain injury following a subarachnoid hemorrhage: a possible role for the regulation of pro-inflammatory cytokines [J]. J Pineal Res,2014,57(3):340-347.
[13] Rajendran JG,Lewis DH,Newell DW,et al. Brain SPECT used to evaluate vasospasm after subarachnoid hemorrhage:correlation with angiography and transcranial Doppler [J]. Clin Nucl Med,2001,26(2):125.
[14] Alexandrov AV,Sloan MA,Tegeler CH,et al. Practice standards for transcranial doppler (tcd) ultrasound. Part ii. Clinical indications and expected outcomes [J]. J Neuroimaging,2012,22:215-224.
[15] Marshall SA,Nyquist P,Ziai WC. The role of transcranial doppler ultrasonography in the diagnosis and management of vasospasm after aneurysmal subarachnoid hemorrhage [J]. Neurosurg Clin N Am,2010,21(2):291-303.
[16] Alexandrov AV,Sloan MA,Wong LK,et al. Practice standards for transcranial doppler ultrasound:Part Ⅰ-test performance [J]. J Neuroimaging,2007,17(1):11-18.
[17] 王嘉煒,高觉民.蛛网膜下腔出血后脑血管痉挛的发生机制及治疗新进展[J].医学研究杂志,2010,39(3):7-11.
[18] 夏燕.TCD对蛛网膜下腔出血后脑血管痉挛的诊断价值[J].湖北科技学院学报:医学版:,2012,26(5):438-439.
[19] Jayakumar AR,Ruiz CR,Tong XY,et al. Brain edemain acute liver failure:Role of neurosteroids [J]. Archbiochem Biophys,2013,536(2):171-175.
[20] 佟建洲,潘勤,佟中豪,等.β-七叶皂甙钠与丹参联用治疗胶质瘤术后脑水肿的疗效观察[J].现代仪器与医疗,2014,20(1):47-50.
[21] 左涛生,许开喜,王金,等.动脉瘤性蛛网膜下腔出血的CT分布规律及MSCTA动脉瘤分布对照分析[J].中国医药科学,2015,5(21):14-18.
[22] Chen J,Chen G,Li J,et al. Melatonin attenuates inflammatory response-induced brain edema in early brain injury following a subarachnoid hemorrhage:a possible role for the regulation of pro-inflammatory cytokines [J]. J Pineal Res,2014,57(3):340-347.
[23] 黄校权,杨清荣,龚裕兴,等.创伤性蛛网膜下腔出血后症状性脑血管痉挛的危险因素分析[J].中国医药科学,2015,(16):153-155.
(收稿日期:2017-03-11 本文编辑:程 铭)