急性ST段抬高型心肌梗死患者经抽吸导管冠脉内局部推注替罗非班的疗效研究
2017-07-24朱红涛刘学庆丁晓军唐剑峰赵剑锋欧阳巍立龚军辉吴明海邱林林
朱红涛,刘学庆,丁晓军,唐剑峰,赵剑锋,欧阳巍立,龚军辉,吴明海,邱林林
急性ST段抬高型心肌梗死患者经抽吸导管冠脉内局部推注替罗非班的疗效研究
朱红涛1,刘学庆1,丁晓军1,唐剑峰1,赵剑锋1,欧阳巍立1,龚军辉1,吴明海1,邱林林1
目的 比较急性心肌梗死患者在行急诊经皮冠状动脉介入治疗(PCI)时,通过抽吸导管冠状动脉病变处给予替罗非班与经指引导管冠状动脉内给予替罗非班的疗效差别。方法 选取2013年1月~2016年1月于江苏省丹阳市人民医院行急诊PCI的急性ST段抬高型心肌梗死的患者共81例,其中40例经抽吸导管在罪犯血管堵塞处局部缓慢推注替罗非班,41例经指引导管冠状动脉内缓慢推注替罗非班。主要终点为各种原因的30 d死亡;次要终点包括PCI术后即刻心肌梗死溶栓治疗(TIMI)血流、心肌呈色分级(MBG)、住院期间再次心肌梗死、靶血管重建、不稳定型心绞痛及心力衰竭。结果 两组患者年龄、性别、心血管疾病危险因素、血压、心率比较差异无统计学意义。经抽吸导管冠状动脉内局部给药组MBG3级患者明显多于经指引导管给药组(68% vs. 36%,P=0.002),非致死性心力衰竭则明显减少(12.5% vs. 25.6%,P=0.0027)。两组患者各种原因30 d死亡(2.5% vs. 2.4%,P=0.943)、TIMI血流3级(92.5% vs. 87.8%,P=0.848)、住院期间再次心肌梗死(0% vs. 1.2%,P=0.764)、靶血管重建(2.5% vs. 4.9%,P=0.931)及不稳定性心绞痛(15% vs. 19.5%,P=0.840)的发生情况差异无统计学意义。结论直接PCI术中经抽吸导管冠状动脉内局部缓慢给药能改善心肌灌注,减少住院期间非致死性心力衰竭发生率,但是对于30 d内不良事件的发生与对照组相比无明显改善。
急性ST段抬高型心肌梗死;经皮冠状动脉介入治疗;替罗非班;心肌灌注
经皮冠状动脉介入治疗(PCI)是急性ST抬高型心肌梗死(STEMI)最有效的治疗方法,在指南要求的时间内,只要能及时实现冠状动脉再灌注,均能明显改善患者预后[1]。然而,尽管PCI术能使心外膜的血流量迅速和有效的恢复,但是很大比例的STEMI患者有发生死亡等并发症的风险。经过PCI术后,心外膜血管再通,但是心肌微血管仍处于堵塞状况,会导致心肌梗死面积增大,左心室功能受损,并增加死亡率[2]。由于急诊PCI后出现的一些潜在的不良预后,为了尽可能实现微血管的再灌注,通过药物和导管相结合的方法,增加罪犯血管局部药物的浓度,诸如血小板糖蛋白Ⅱb/Ⅲa受体拮抗剂,延缓药物的驻留时间,成为急性冠状动脉综合症血管成形术后,改善预后的一个非常有希望的方法[3]。本研究通过回顾性分析本院81例直接PCI的STEMI患者,比较经血栓抽吸导管局部缓慢给药及经指引导管给药的疗效区别,为临床治疗提供更多思路。
1 方法
1.1 研究对象 江苏省丹阳市人民医院近6年内共有208例STEMI患者行急诊PCI术,随机选取2013年1月~2016年1月住院的81例患者,均行梗死相关动脉血栓抽吸术,所有入选患者临床资料保存完整,均满足本研究需要。入选标准:持续胸痛≥30 min,发病时间<12 h,心电图相邻两个导联ST段抬高≥0.1 mV,冠状动脉造影提示血管完全或次全闭塞,有明显的血栓负荷。排除标准:15 d内使用过纤溶药物、怀疑活动性出血、2年内有脑血管事件、血小板<105/μl、有肿瘤病史、严重肝肾功能障碍、感染及患有血液系统疾病。
1.2 分组和治疗方法 将入组患者分为引导管给药组(n=41)和抽吸导管局部给药组(n=40),引导管给药组:指引导管到位后经冠脉开口注射替罗非班13~15ml(远大医药(中国)有限公司,5 mg/100 ml),术后静脉维持12 h(0.1 μg/ kg/min)。抽吸导管局部给药组,指经抽吸导管在罪犯血管堵塞处局部缓慢注射替罗非班(剂量同上),给药时间持续5 min,术后静脉维持12 h(剂量同上)。两组患者无论给药后闭塞血管是否有血流通过,均以抽吸导管抽吸,根据血栓负荷情况决定抽吸次数。两组均植入药物涂层支架,术前口服阿司匹林300 mg,氯吡格雷600 mg。急诊冠状动脉造影时静脉推注普通肝素2000 IU,行PCI时肝素补足到70 IU/kg。常规给予他汀类药物,根据血压及心率情况给予ACEI或ARB类药物及β受体阻滞剂。
1.3 观测指标 入院患者均检查血脂、血糖、肝肾功能、心肌酶、肌钙蛋白及C反应蛋白等,所有入选患者术后一周左右Simpson法测定左室射血分数(LVEF)值,术后1 h心电图ST下落的百分比(术前ST段抬高的幅度(mm)-术后1 h ST段抬高的幅度(mm)/术前ST段抬高的幅度(mm)×100%)。两位冠心病介入专科医生仔细评估冠状动脉造影结果,目测法估计TIMI血流分级及心肌呈色分级(MBG)。血流TIMI 0~1级为冠状动脉造影未再通,TIMI 2~3级为冠状动脉造影再通,TIMI3级为冠状动脉造影完全再通。MBG 0级:无心肌显影或对比密度;MBG I级:有少许心肌显影或造影剂密度;MBG 2级:有中度心肌显影或造影剂密度,但不及同侧或对侧非梗死相关动脉造影时的心肌显影或造影剂密度,心肌部分灌注;MBG 3级:正常心肌显影或造影剂密度,与同侧或对侧非梗死相关动脉造影时的心肌显影或造影剂密度相当,心肌完全再灌注。MBG 0~1级为心肌无再灌注,MBG2~3级为心肌再灌注,MBG 3级为心肌完全再灌注。
1.4 终点指标 观察替罗非班治疗后冠脉TIMI血流分级[4]、心肌呈色分级[5],住院期间非致死性再次心肌梗死、缺血性靶器官重建、不稳定心绞痛及非致死性心功能衰竭及出院30 d各种原因死亡。
1.5 统计学分析 采用SPSS 19.0软件进行统计学分析,计量资料以均数±标准差(±s)表示,组间比较采用t检验;计数资料用百分比表示,率的比较采用卡方检验,P<0.05为差异有统计学意义。
2 结果
2.1 两组患者一般临床资料比较 所有患者入院后均记录年龄、性别、心血管疾病危险因素、血压、心率等。两组一般情况组间比较差异无统计学意义(P>0.05)(表1)。
2.2 两组患者冠状动脉造影造影及临床情况 胸痛时间,病变血管及罪犯血管,术中血流通过时间,支架植入情况,出院前心脏超声均无统计学意义,术后抽吸导管局部给药组心电图ST段回落较指引导管给药组更明显(P=0.004)(表2)。
2.3 两组患者心肌再灌注情况比较 抽吸导管局部给药组治疗后MBG 3级患者比例明显高于指引导管给药组(P<0.05)。TIMI血流分级治疗前后两组0~3级比例均无统计学意义(P>0.05)(表3)。
2.4 出院30 d随访及住院期间心脏事件 住院期间两组在不稳定性心绞痛,非致死性再次心肌梗死,缺血性靶器官重建的发生情况比较均无统计学差异(P>0.05),而指引导管给药组非致死性心功能衰竭发生率显著升高(P<0.05)。出院30 d各种原因死亡发生率上无差异,抽吸导管局部给药组1例死亡,死因为冠状动脉三支血管病变,心力衰竭反复发作,泵衰竭;经指引导管给药组1例死亡,死因为心室颤动(表4)。
3 讨论
2013年ACC/AHA急性STEMI指南更新中,根据两个随机临床试验[6,7]和一个荟萃分析[8]的结果,推荐STEMI患者急诊PCI时,行血栓抽吸术(Ⅱa类推荐,B级证据)。尽管如此,INFUSE-AMI试验[9]并不支持上述观点,该试验入选了来自37家医院的452例发病4 h内的急性心肌梗死(AMI)患者,均为前降支近端或中段闭塞,术中使用比伐卢定抗凝,随机分为三组,阿昔单抗梗死部位注射组、血栓抽吸组及无血栓抽吸组。术后30 d,通过心脏磁共振评估梗死面积,结果发现血栓抽吸组及无血栓抽吸组无显著差别。但是,该实验中,冠脉内注射阿昔单抗组则明显减少梗死面积,改善预后。ICE试验[10]及Soon等[11]的研究结果也支持上述结论,冠脉内注射Ⅱb/Ⅲa受体剂能改善心外膜血管的灌注及心肌灌注,降低住院期间主要心血管不良事件。近年来TASTE[12,13]及TOTAL[14]实验结果,也提示血栓抽吸并不能减少STEMI患者30 d及1年死亡率,因此中国经皮冠状动脉介入治疗指南(2016)[15]不推荐直接PCI前常规血栓抽吸(ⅢC)。
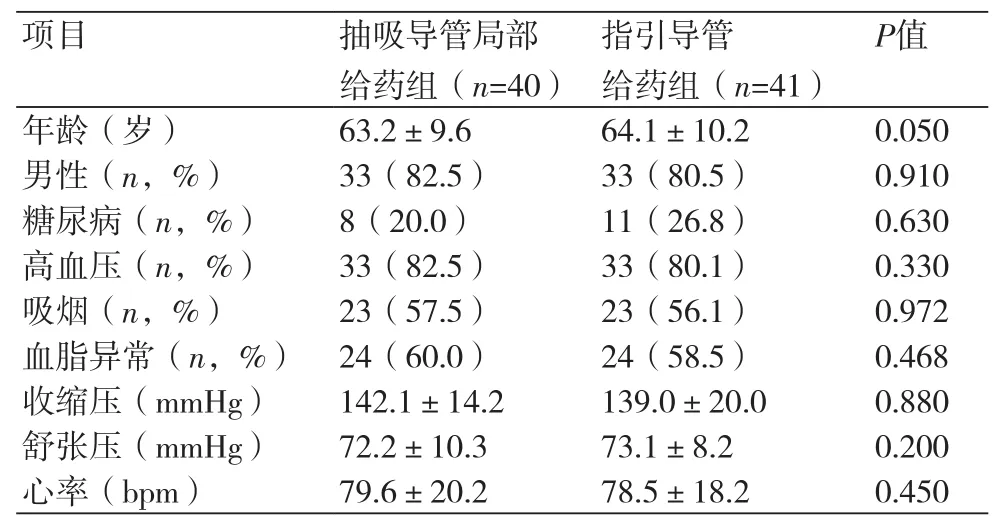
表1 两组患者一般临床资料描述及比较

表2 冠状动脉造影及临床情况比较
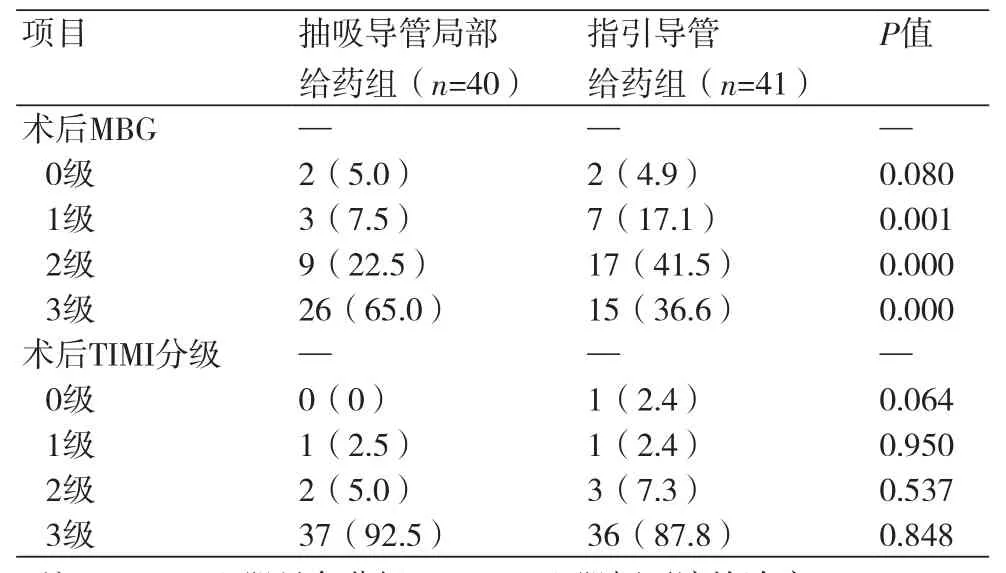
表3 两组患者替罗非班治疗后MBG及TIMI血流比较
目前认为,AMI患者直接PCI过程中,只有达到心肌水平再灌注,才能改善预后,减少并发症,血栓抽吸虽使心外膜灌注达到TIMI3级血流患者增加,但是仍有部分患者存在微血管障碍,导致心肌灌注水平不良。PCI术后发生远段栓塞、无复流或慢血流是预后不良的独立预测因子[16]。血小板糖蛋白Ⅱb/Ⅲa拮抗剂通过阻断血小板聚集的最后通路,从而发挥抗血小板聚集的作用,已经被证实是目前最强效的抗血小板药物,能改善无复流或慢血流的发生率。因此,根据血栓负荷情况,PCI术中静脉或经指引导管冠状动脉内给予Ⅱb/Ⅲa拮抗剂,以期待减少远端血栓栓塞及慢血流的发生。但对于静脉内及经冠状动脉给以Ⅱb/Ⅲa拮抗剂,结果不同,两项荟萃分析显示[17,18]多数研究认为,冠状动脉内注射Ⅱb/Ⅲa拮抗剂能提高LVEF、减少心力衰竭的发生,增加TIMI3级血流,两者住院期间死亡率、靶血管重建、再次心肌梗死、大出血及支架内血栓的发生无明显差别,所有研究多无更长时间的随访结果。虽然经冠状动脉给予Ⅱb/Ⅲa受体拮抗剂取得一些积极的效果,但是指引导管给药无法到达冠状动脉的远端分支,不能直接作用于病变部位,对远端微血管的作用有限,另外,注射的药物由于血栓堵塞,可能反流进入主动脉,从而进入全身循环。Francesco Prati等[19]使用ClearWay RX灌注球囊,在冠状动脉病变局部,经球囊缓慢推注Ⅱb/Ⅲa受体拮抗剂,给药前后使用光学相干断层成像监测血栓负荷,结果无论经灌注导管局部给药(IL组)及经冠状动脉给药(IC组),或者抽吸与否,都不能减少术后支架内血栓负荷。但是,和IC组相比,IL组能提高造影指标,改善心肌灌注。李世英等[20]在STEMI患者行急诊PCI术时,经抽吸导管在梗死相关动脉内注射替罗非班并行血栓抽吸,同单纯血栓抽吸组相比,能明显改善心肌灌注,不良心血管事件有降低趋势。孙宇琚等[21]比较经靶向灌注导管和经指引导管冠状动脉内给予替罗非班,对急性冠状动脉综合征患者PCI术后的影响。结果与经指引导管冠状动脉内给予替罗非班相比,经靶向灌注导管在靶病变远段给药显著改善急性冠状动脉综合征患者心肌组织灌水平,两者院内心血管事件及出血事件发生率相当。

表4 两组住院期间心脏事件比较及出院30 d死亡情况比较
本研究回顾性的分析我院81例AMI患者发现,通过评估MBG达到3级的比例(65% vs. 36.6%),经抽吸导管局部给予替罗非班能显著改善心肌灌注,同时能降低住院期间心功能衰竭的发生率,这和上述部分研究结果相似。虽然和灌注导管相比,局部浓度稍低,但通过增加注射时间,也能起到相似的效果,简单实用,节约手术费用,减少手术时间,在基层医院非常实用。由于本研究是回顾性分析,部分资料不全,无法统计出院更长时间的心血管事件发生率,所以对于改善冠状动脉血流,能否转化为改善患者的长期预后尚不明确,仍需大样本前瞻性随机试验进一步证实。
[1] O'gara PT,Kushner FG,Ascheim DD,et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines[J]. J Am Coll Cardiol, 2013,61(4):485-510.
[2] Van de werf F,Bax J,Betriu A,et al. Management of acute myocardial infarction in patients presenting with persistent ST-segment elevation: the Task Force on the Management of ST-Segment Elevation Acute Myocardial Infarction of the European Society of Cardiology[J]. Eur Heart J,2008,29(23):2909-45.
[3] Keeley EC,Hillis LD. Primary PCI for myocardial infarction with ST-segment elevation[J]. N Engl J Med,2007,356(1):47-54.
[4] Chesebro JH,Knatterud G,Roberts R,et al. Thrombolysis in Myocardial Infarction (TIMI) Trial, Phase I: A comparison between intravenous tissue plasminogen activator and intravenous streptokinase. Clinical findings through hospital discharge[J]. Circulation,1987,76(1):142-54.
[5] Van't Hof AW,Liem A,Suryapranata H,et al. Angiographic assessment of myocardial reperfusion in patients treated with primary angioplasty for acute myocardial infarction: myocardial blush grade. Zwolle Myocardial Infarction Study Group[J]. Circulation,1998,97(23):2302-6.
[6] Sardella G,Mancone M,Bucciarelli-Ducci C,et al. Thrombus aspiration during primary percutaneous coronary intervention improves myocardial reperfusion and reduces infarct size: the EXPIRA (thrombectomy with export catheter in infarct-related artery during primary percutaneous coronary intervention) prospective, randomized trial[J]. J Am Coll Cardiol,2009,53(4):309-15.
[7] Vlaar PJ,Svilaas T,van der Horst IC,et al. Cardiac death and reinfarction after 1 year in the Thrombus Aspiration during Percutaneous coronary intervention in Acute myocardial infarction Study (TAPAS): a 1-year follow-up study[J]. Lancet,2008,371(9628):1915-20.
[8] Bavry AA,Kumbhani DJ,Bhatt DL. Role of adjunctive thrombectomy and embolic protection devices in acute myocardial infarction: a comprehensive meta-analysis of randomized trials[J]. Eur Heart J,2008,29(24):2989-3001.
[9] Stone GW,Maehara A,Witzenbichler B,et al. Intracoronary abciximab and aspiration thrombectomy in patients with large anterior myocardial infarction: the INFUSE-AMI randomized trial[J]. JAMA,2012,307(17): 1817-26.
[10] Deibele AJ,Jennings LK,Tcheng JE,et al. Intracoronary eptifibatide bolus administration during percutaneous coronary revascularization for acute coronary syndromes with evaluation of platelet glycoproteinⅡb/Ⅲa receptor occupancy and platelet function: the Intracoronary Eptifibatide (ICE) Trial[J]. Circulation,2010,121(6):784-91.
[11] Soon D,Ho HH,Loh KK,et al. Clinical outcomes of intracoronary eptifibatide bolus only versus intracoronary bolus and intravenous infusion of eptifibatide in primary percutaneous coronary intervention[J]. Acute Card Care,2012,14(1):42-4.
[12] Lagerqvist B,Fröbert O,Olivecrona GK,et al. Outcomes 1 year after thrombus aspiration for myocardial infarction[J]. N Engl J Med,2014, 371(12):1111-20.
[13] Fröbert O,Lagerqvist B,Olivecrona GK,et al. Thrombus aspiration during ST-segment elevation myocardial infarction[J]. N Engl J Med, 2013,369(17):1587-97.
[14] Jolly SS,Cairns JA,Yusuf S,et al. Outcomes after thrombus aspiration for ST elevation myocardial infarction: 1-year follow-up of the prospective randomised TOTAL trial[J]. Lancet,2016,387(10014):127-35.
[15] 中华医学会心血管病学分会介入心脏病学组,中国医师协会心血管内科医师分会血栓防治专业委员会,中华心血管病杂志编辑委员会. 中国经皮冠状动脉介入治疗指南(2016)[J]. 中华心血管病杂志,2016,44(5):382-400.
[16] Pu J,Mintz GS,Biro S,et al. Insights into echo-attenuated plaques, echolucent plaques, and plaques with spotty calcification: novel findings from comparisons among intravascular ultrasound, nearinfrared spectroscopy, and pathological histology in 2,294 human coronary artery segments[J]. J Am Coll Cardiol,2014,63(21):2220-33.
[17] Ali-Hassan-Sayegh S,Mirhosseini SJ,Shahidzadeh A,et al. Appropriate bolus administration of glycoprotein Ⅱb/Ⅲa inhibitors for patients with acute coronary syndromes undergoing percutaneous coronary intervention: intracoronary or intravenous? A comprehensive and updated meta-analysis and systematic review[J]. Kardiol Pol,2016,74(2):104-18.
[18] Wang JN,Diao S,Tang YJ,et al. Intracoronary versus intravenous administration of abciximab in patients with acute coronary syndrome: a meta-analysis[J]. Plos One,2013,8(2):e58077.
[19] Prati F,Romagnoli E,Limbruno U,et al. Randomized evaluation of intralesion versus intracoronary abciximab and aspiration thrombectomy in patients with ST-elevation myocardial infarction: The COCTAIL Ⅱ trial[J]. Am Heart J,2015,170(6):1116-23.
[20] 李世英,颜红兵,王健,等. 直接经皮冠状动脉介入治疗中血栓抽吸联合梗死相关动脉内应用替罗非班的有效性和安全性[J]. 中华心血管病杂志,2010,38(10):880-5.
[21] 孙宇珺,周雯,丁嵩,等. 经靶向灌注导管在冠状动脉靶病变远段给予替罗非班对急性冠状动脉综合征患者心肌灌注的影响[J]. 中国介入心脏病学杂志,2015,23(1):5-10.
本文编辑:阮燕萍
Efficiency of intracoronary administration of tirofiban through aspiration catheter in patients with acute ST-elevation myocardial infarction undergoing percutaneous coronary intervention
ZHU hong-tao*, LIU xue-qing, DING xiao-jun, TANG jian-feng, ZHAO jian-feng, OUYANG wei-li, GONG jun-hui, WU ming-hai, QIU lin-lin.*Department of Cardiology, People's hospital of Danyang, The Affiliated Hospital of Nantong University, Zhenjiang 212300, China.
QIU lin-lin,E-mail:13952912866@163.com
Objectives In patients with acute ST-segment elevation myocardial infarction (STEMI) who underwent percutaneous coronary intervention (PCI), the efficacy of tirofiban administrated through aspiration catheter and guided catheter was compared. Methods 81 patients with acute STEMI undergoing primary PCI were enrolled between January 2013 and January 2016, 40 patients were administrated tirofiban in the plug of culprit vessel through aspiration catheter, 41 patients were administrated tirofiban through guided catheter in the coronary. The primary end point is death within 30 days of various causes; secondary end points include immediate thrombolysis in myocardial infarction (TIMI) after PCI, myocardial blush grades (MBG), re-myocardial infarction during hospitalization, target vessel reconstruction (TVR), Unstable angina (UA) and heart failure (HF). Results There were no significant differences in age, sex, cardiovascular risk factors, blood pressure and heart rate between the two groups. The incidence of MBG 3 in aspiration catheter group was significant higher than that in guided catheter group (68% vs. 36%; P value = 0.002). The incidence of nonfatal heart failure in aspiration catheter group was significant lower than that in guided catheter group (12.5% vs. 25.6%; P value = 0.0027). There were no significant differences in death within 30 days (2.5% vs. 2.4%; P value = 0.943), TIMI 3 (92.5% vs. 87.8%; P value = 0.848), re-myocardial infarction during hospitalization (0% vs. 1.2%; P value = 0.764), TVR (2.5% vs. 4.9%; P value = 0.931), UA (15% vs. 19.5%; P value = 0.840). Conclusion Tirofiban administrated through aspiration catheter during PCI can improve myocardial perfusion, reduce the incidence of non-fatal heart failure during hospitalization, but cannot reduce adverse events within 30 days.
STEMI; Percutaneous coronary intervention; Tirofiban; Myocardial perfusion
R541.4
A
1674-4055(2017)06-0738-04
1212300 丹阳,江苏省丹阳市人民医院心血管内科
邱林林,E-mail:13952912866@163.com
10.3969/j.issn.1674-4055.2017.06.29
