肠型胃癌和弥漫型胃癌的临床特点及预后研究
2017-05-18曹文君李慧娟
曹文君,李 敏,李慧娟
·论著·
肠型胃癌和弥漫型胃癌的临床特点及预后研究
曹文君1*,李 敏2,李慧娟2
目的 探讨肠型胃癌和弥漫型胃癌的临床特点及预后。方法 选取2007-01-01至2015-12-30在长治医学院附属和平医院外科病房手术治疗的胃癌患者392例,其中肠型231例(58.9%),弥漫型161例(41.1%)。建立胃癌流行病学调查问卷,并由经过培训的专业人员按统一标准采集胃癌患者信息,包括基本情况(性别、年龄、身高、体质量、文化程度、婚姻状况、血型、幽门螺杆菌感染、肿瘤家族史)、生活方式及习惯(吸烟、饮酒、进食速度、进食烫食、进食酸菜/咸菜/泡菜、进食油炸食品)及病理诊断与临床分期等;并由本院中心实验室具有硕士及以上学历人员对患者进行电话随访,询问生存情况,随访截至2015-12-30。结果 肠型与弥漫型胃癌患者性别、体质指数(BMI)、文化程度、婚姻状况、血型、幽门螺杆菌感染、肿瘤家族史比较,差异无统计学意义(P>0.05);肠型与弥漫型胃癌患者年龄比较,差异有统计学意义(P<0.05)。肠型与弥漫型胃癌患者吸烟、饮酒比较,差异有统计学意义(P<0.05);肠型与弥漫型胃癌患者进食速度、进食烫食、进食酸菜/咸菜/泡菜、进食油炸食品比较,差异无统计学意义(P>0.05)。肠型与弥漫型胃癌患者T期、M期比较,差异无统计学意义(P>0.05);肠型与弥漫型胃癌患者N期比较,差异有统计学意义(P<0.05)。340例胃癌患者完成随访,随访率为86.7%;截至随访日期,肠型胃癌患者生存率为66.5%(129/194),中位生存时间为24个月;弥漫型胃癌患者生存率为52.7%(77/146),中位生存时间为18个月。肠型与弥漫型胃癌患者生存曲线比较,差异有统计学意义(P<0.05)。结论 不同Lauren分型胃癌临床特点和预后不同。Lauren分型在胃癌治疗及预防中起一定的决策作用。
胃肿瘤;Lauren分型;临床特点;预后
曹文君,李敏,李慧娟.肠型胃癌和弥漫型胃癌的临床特点及预后研究[J].中国全科医学,2017,20(13):1587-1591.[www.chinagp.net]
CAO W J,LI M,LI H J.Clinical characteristics and prognosis of intestinal-type and diffuse-type gastric cancer[J].Chinese General Practice,2017,20(13):1587-1591.
胃癌是世界上常见恶性肿瘤之一,是癌症相关死亡的一个主要原因[1]。据国际癌症研究机构(IARC)发布的癌症统计数据显示,2012年,全世界范围内有952 000例新增胃癌患者,占癌症患者的6.8%,其中死亡患者为723 000例,占癌症总死亡患者的8.8%[2]。全世界有超过70%的胃癌患者在发展中国家,其中50%的胃癌患者在亚洲东部(主要是中国)。在我国城市,胃癌死亡率男性为112.5/10万,居恶性肿瘤的第3位;女性为50.4/10万,居恶性肿瘤的第2位[3]。胃癌早期诊断率低,预后较差,严重影响身体健康。目前,胃镜是诊断胃癌的金标准,但由于胃镜灵敏度较低、成本较高,从而使得胃癌的早期诊断受到了一定的限制[4]。此外,由于胃癌早期症状不明显,不易被确诊,多数患者临床确诊时已到了胃癌晚期,导致胃癌的预后效果差[5]。当前,胃癌仍以手术治疗为主,但术后仍有50%患者发生复发转移,有研究显示,胃癌Ⅱ期患者的5年生存率为30%~50%,但是Ⅲ期患者的5年生存率就降为10%~25%[6]。此外,有研究认为,约30%的癌症死亡源自个体行为[7]。胃癌按照Lauren分型分为肠型和弥漫型[8],本研究拟通过收集患者的基本情况(年龄、职业、文化程度等)、生活方式及习惯(吸烟、饮酒、进食速度等)、病理诊断与临床分期等信息,对不同分型胃癌的临床特点和预后进行深入探讨,分析个人行为对不同分型胃癌发病风险的影响,以期有效预防胃癌的发生,从而降低其发病率。
1 对象与方法
1.1 研究对象 选取2007-01-01至2015-12-30在长治医学院附属和平医院外科病房手术治疗的胃癌患者392例。纳入标准:均经手术病理检查确诊为胃癌。排除标准:认知行为异常及伴其他躯体疾病不能参与数据采集者。其中男308例(78.6%),女84例(21.4%);年龄29~80岁,中位年龄59.0(12.8)岁;已婚378例(96.4%),未婚/离婚/丧偶14例(3.6%);BMI为14.2~31.6 kg/m2,平均BMI为(22.2±3.2)kg/m2;肠型231例(58.9%),弥漫型161例(41.1%)。本研究经长治医学院伦理学委员会批准,患者或其家属知情同意。
1.2 研究方法
1.2.1 问卷调查 参照国内外胃癌健康风险因素和相关文献[9-11]建立胃癌流行病学调查问卷,并由经过培训的专业人员按统一标准采集胃癌患者信息,包括基本情况(性别、年龄、身高、体质量、文化程度、婚姻状况、血型、幽门螺杆菌感染、肿瘤家族史)、生活方式及习惯(吸烟、饮酒、进食速度、进食烫食、进食酸菜/咸菜/泡菜、进食油炸食品)及病理诊断与临床分期等,将信息录入已建立的肿瘤信息标本库。
1.2.2 标本判定 手术标本统一由2名具有高级职称的病理医师进行判定。胃癌病理分型按照Lauren分型分为肠型和弥漫型[8]。临床分期按照美国癌症联合会(AJCC)第6版(2002年)TNM分期,TNM是对肿瘤浸润(T)、淋巴结转移(N)及远端组织(M)进行定义[12]。本研究中T分为T1(肿瘤侵犯黏膜基层或下层)、T2(肿瘤侵犯固有肌层或浆膜下层)、T3(肿瘤侵犯浆膜)、T4(肿瘤侵犯邻近组织结构);N分为N1(1~2个淋巴结转移)、N2(3~6个淋巴结转移)、N3(7个及以上淋巴结转移);M分为M0(无远端转移)、M1(有远端转移)。
1.2.3 预后随访 由本院中心实验室具有硕士及以上学历人员对患者进行电话随访,随访截至2015-12-30。随访前进行专业语言培训,询问患者生存情况,如死亡则记录死亡时间,如存活则记录目前身体状况,并嘱咐其家属按时复查。
1.3 统计学方法 采用SPSS 19.0统计软件进行统计学分析,计数资料比较采用χ2检验;采用Kaplan-Meier法绘制生存曲线,组间比较采用Log-rank检验。以P<0.05为差异有统计学意义。
2 结果
2.1 肠型与弥漫型胃癌患者基本情况比较 肠型与弥漫型胃癌患者性别、体质指数(BMI)、文化程度、婚姻状况、血型、幽门螺杆菌感染、肿瘤家族史比较,差异无统计学意义(P>0.05);肠型与弥漫型胃癌患者年龄比较,差异有统计学意义(P<0.05,见表1)。
2.2 肠型与弥漫型胃癌患者生活方式及习惯比较 肠型与弥漫型胃癌患者吸烟、饮酒比较,差异有统计学意义(P<0.05);肠型与弥漫型胃癌患者进食速度、进食烫食、进食酸菜/咸菜/泡菜、进食油炸食品比较,差异无统计学意义(P>0.05,见表2)。
2.3 肠型与弥漫型胃癌患者临床分期比较 肠型与弥漫型胃癌患者T期、M期比较,差异无统计学意义(P>0.05);肠型与弥漫型胃癌患者N期比较,差异有统计学意义(P<0.05,见表3)。
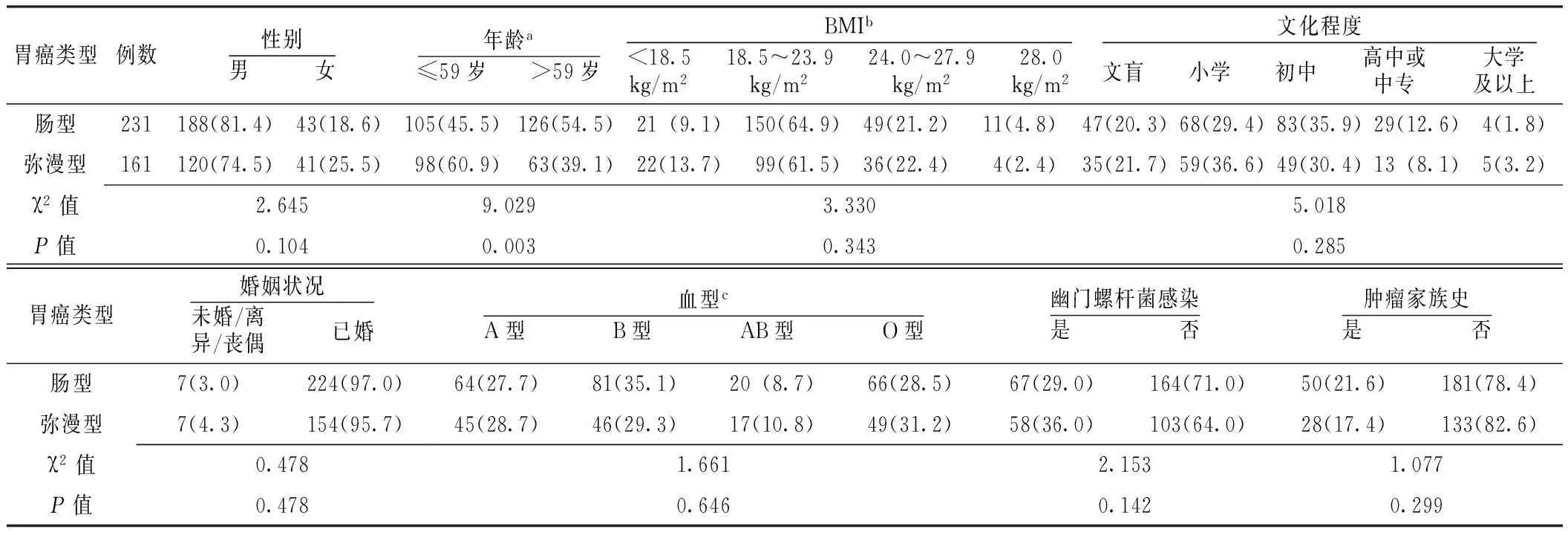
表1 肠型与弥漫型胃癌患者基本情况比较〔n(%)〕
注:a年龄的分类根据中位年龄;bBMI的分类参照文献[13]定义标准;c为数据有缺失;BMI=体质指数

表2 肠型与弥漫型胃癌患者生活方式及习惯比较〔n(%)〕

表3 肠型与弥漫型胃癌患者临床分期比较〔n(%)〕
2.4 肠型胃癌与弥漫型胃癌患者Kaplan-Meier生存曲线比较 340例胃癌患者完成随访,随访率为86.7%;截至随访日期,肠型胃癌患者生存率为66.5%(129/194),中位生存时间为24个月;弥漫型胃癌患者生存率为52.7%(77/146),中位生存时间为18个月。肠型与弥漫型胃癌患者生存曲线比较,差异有统计学意义(χ2=12.415,P<0.001,见图1)。
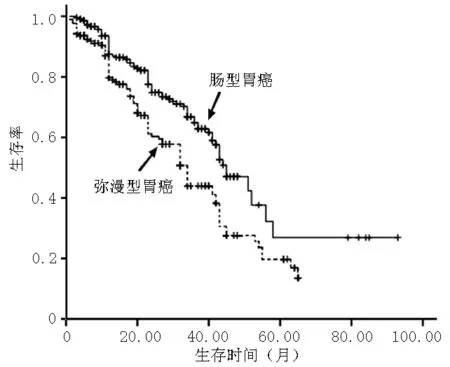
图1 肠型与弥漫型胃癌患者Kaplan-Meier生存曲线比较
Figure 1 Comparison of the Kaplan-Meier survival curve between patients with intestinal-type gastric cancer and patients with diffuse-type gastric cancer
3 讨论
有研究报道,发展中国家胃癌的死亡率是发达国家的3.8~7.9倍[14],而我国中部的山西省又是胃癌高发区[15]。Lauren分型最早于1965年提出,因其简单易行、可重复性强而被大多数国家临床工作者和研究者采用至今。不同胃癌分型健康危险因素和预后不同,临床流行病学研究发现,亚洲国家如中国、日本肠型胃癌发病率高于其他国家[16]。本研究中肠型胃癌患者占58.9%,弥漫型胃癌患者占41.1%。
有研究认为,弥漫型胃癌多发于年轻女性,更易出现淋巴结转移[17]。本研究结果显示,弥漫型胃癌更易发生距原发灶边缘3 cm以外的淋巴结转移,而不同Lauren分型胃癌的T、M分期无统计学意义。有最新研究报道,幽门螺杆菌阳性与胃癌组织学分型无关[17],本研究结果进一步验证了这一点。此外,多数研究关注不同胃癌分型的临床特点及治疗[18-21],而较少报道不同胃癌分型患者在个人行为习惯方面的差异,本研究结果显示,弥漫型胃癌与肠型胃癌在吸烟、饮酒上有差异,而在性别、BMI、文化程度、婚姻状况、血型、肿瘤家族史、饮食习惯(进食速度、进食烫手、进食酸菜/咸菜/泡菜、进食油炸食品)上无差异。
本研究生存分析结果显示,弥漫型胃癌患者预后差,总体生存率较肠型胃癌患者低,与既往研究报道结果一致,即弥漫型胃癌患者5年总生存率(44.1%)低于肠型胃癌患者(52.7%),且弥漫型胃癌发生远端淋巴结转移的风险较高[22]。因此Lauren分型在胃癌治疗及预防中起一定的决策作用。
作者贡献:曹文君进行文章的构思与设计、统计学处理、结果的分析与解释、撰写论文、中英文修订,负责文章的质量控制及审校,对文章整体负责,监督管理;李敏进行研究的实施与可行性分析、数据整理;李慧娟进行数据收集。
本文无利益冲突。
本文链接:
胃癌Lauren分型的病理表现:(1)肠型,一般有腺腔形成,癌细胞为柱状或立方形,游离缘常可见刷状缘,似肠上皮的吸收细胞,部分癌细胞似肠化生的杯状细胞,癌旁黏膜常伴有广泛的萎缩性胃炎和肠上皮化生;(2)弥漫型,无腺腔形成,癌细胞为分化差的小圆形细胞,细胞之间黏着力差,弥漫散在,癌旁黏膜无或仅有小片萎缩性胃炎和肠上皮化生;(3)不能分型,难以划分为肠型或弥漫型或在同一肿瘤内含有两种类型。
[1]BERTUCCIO P,CHATENOUD L,LEVI F,et al.Recent patterns in gastric cancer:a global overview [J].Int J Cancer,2009,125(3):666-673.DOI:10.1002/ijc.24290.
[2]FERLAY J,SOERJOMATARAM I,DIKSHIT R,et al.Cancer incidence and mortality worldwide:sources,methods and major patterns in GLOBOCAN 2012[J].Int J Cancer,2015,136(5):E359-386.DOI:10.1002/ijc.29210.
[3]CHEN W,ZHENG R,BAADE P D,et al.Cancer statistics in China,2015 [J].CA Cancer J Clin,2016,66(2):115-132.DOI:10.3322/caac.21338.
[4]WANG J L,HU Y,KONG X,et al.Candidate microRNA biomarkers in human gastric cancer:a systematic review and validation study[J].PLoS One,2013,8(9):e73683.DOI:10.1371/journal.pone.0073683.
[5]ANG T L,KHOR C J,GOTODA T.Diagnosis and endoscopic resection of early gastric cancer[J].Singapore Med J,2010,51(2):93-100.
[6]WÖHRER S S,RADERER M,HEJNA M.Palliative chemotherapy for advanced gastric cancer[J].Ann Oncol,2004,15(11):1585-1595.DOI:10.1093/annonc/mdh422.
[7]STEWART B,WILD C P,International Agency for Research on Cancer,et al.World cancer report 2014[EB/OL].[2016-03-11].http://www.thehealthwell.info/node/725845.
[8]LAUREN P.The two histologic main types of gastric carcinoma:diffuse andso-called intestinal type carcinoma.An attempt at a histo-clinical classification[J].Acta Parhol Microbid Scand,1965,64(1):31-49.DOI:10.1002/1097-0142.
[9]陈增瑞,江飞.玉环县海岛居民胃癌影响因素的病例对照研究[J].实用肿瘤杂志,2007,22(3):213-217.DOI:10.13267/j.cnki.syzlzz.2007.03.009. CHEN Z R,JIANG F.A matched case-control study on influential factor of gastric cancer in Island Yuhuan[J].Journal of Practical Oncology,2007,22(3):213-217.DOI:10.13267/j.cnki.syzlzz.2007.03.009.[10]王学高,刘爱民,刘荣海,等.盐城市35岁以上居民胃癌发病影响因素的条件Logsitic回归分析[J].预防医学论坛,2007,13(11):963-965.DOI:10.3969/j.issn.1672-9153.2007.11.002. WANG X G,LIU A M,LIU R H,et al.Conditional Logistic analysis of gastric cancer among residents over 35 in Yancheng City[J].Prev Med Trib,2007,13(11):963-965.DOI:10.3969/j.issn.1672-9153.2007.11.002.
[11]SUNG N Y,CHOI K S,PARK E C,et al.Smoking,alcohol and gastric cancer risk in Korean men:the National Health Insurance Corporation Study[J].Br J Cancer,2007,97(5):700-704.DOI:10.1038/sj.bjc.6603893.
[12]毛伟征,苏东明,李雪萍,等.AJCC癌症分期手册[M].6版.沈阳:辽宁科学技术出版社,2005:91-98. MAO W Z,SU D M,LI X P,et al.AJCC cancer staging manual[M].6th ed.Shenyang:Liaoning Science and Technology Press,2005:91-98.
[13]CAO W J,CHEN C S,HUA Y,et al.Factor analysis of a health-promoting lifestyle profile (HPLP):application to older adults in mainland China[J].Arch Gerontol Geriatr,2012,55(3):632-638.DOI:10.1016/j.archger.2012.07.003.
[14]YU M,ZHENG H C,XIA P,et al.Comparison in pathological behaviours & prognosis of gastric cancers from general hospitals between China & Japan[J].Indian J Med Res,2010,132:295-302.
[15]HYLAND P L,LIN S W,HU N,et al.Genetic variants in fas signaling pathway genes and risk of gastric cancer[J].Int J Cancer,2014,134(4):822-831.DOI:10.1002/ijc.28415.
[16]刘霞,杨明,张艳桥.肠型胃癌的研究进展[J].中国肿瘤,2015,24(10):855-858.DOI:10.11735/j.issn.1004-0242.2015.10.A012. LIU X,YANG M,ZHANG Y Q.Research progress in intestinal-type gastric cancer[J].China Cancer,2015,24(10):855-858.DOI:10.11735/j.issn.1004-0242.2015.10.A012.
[17]李一鑫,李秀明,张楠,等.幽门螺杆菌感染与胃癌发生发展及预后的相关性研究[J].中华肿瘤防治杂志,2015,22 (2):91-94.DOI:10.16073/j.cnki.cjcpt.2015.02.003. LI Y X,LI X M,ZHANG N,et al.Associations of Helicobacter pylori infection with the pathogenesis,progression and prognosis in patients with gastric cancer[J].Chinese Journal of Cancer Prevention and Treatment,2015,22(2):91-94.DOI:10.16073/j.cnki.cjcpt.2015.02.003.
[18]白鸽,初建虎,郑超,等.胃癌Lauren分型临床特点及预后分析[J].新医学,2015,46(10):682-684.DOI:10.3969/g.issn.0253-9802.2015.10.009. BAI G,CHU J H,ZHENG C,et al.Clinicopathological characteristics and prognosis of gastric adenocarcinoma with different Lauren classification[J].New Medicine,2015,46(10):682-684.DOI:10.3969/g.issn.0253-9802.2015.10.009.
[19]郑真,谢聪颖.胃癌的Lauren分型个体化治疗[J].肿瘤学杂志,2015,21(8):688-693.DOI:10.11735/j.issn.1671-170X.2015.08.B014. ZHENG Z,XIE C Y.Review on Lauren classification and individual treatments of gastric cancer[J].Journal of Chinese Oncology,2015,21(8):688-693.DOI:10.11735/j.issn.1671-170X.2015.08.B014.
[20]LAYKE J C,LOPEZ P P.胃癌:诊断和治疗方案的选择[J].中国全科医学,2015,18(3):248-249.DOI:10.3969/j.issn.1007-9572.2015.03.04. LAYKE J C,LOPEZ P P.Gastric cancer:diagnosis and treatment options[J].Chinese General Practice,2015,18(3):248-249.DOI:10.3969/j.issn.1007-9572.2015.03.04.
[21]黎鹏,衣艳梅,李淑贤.肿瘤浸润淋巴细胞与胃癌预后关系的研究进展[J].中国全科医学,2015,18(28):3496-3500.DOI:10.3969/j.issn.1007-9572.2015.28.027. LI P,YI Y M,LI S X.Research progress of the relationship between tumor infiltrating lymphocytes and gastric carcinoma[J].Chinese General Practice,2015,18(28):3496-3500.DOI:10.3969/j.issn.1007-9572.2015.28.027.
[22]QIU M Z,CAI M Y,ZHANG D S,et al.Clinicopathological characteristics and prognostic analysis of Lauren classification in gastric adenocarcinoma in China[J].J Transl Med,2013,11:58.DOI:10.1186/1479-5876-11-58.
(本文编辑:崔沙沙)
Clinical Characteristics and Prognosis of Intestinal-type and Diffuse-type Gastric Cancer
CAOWen-jun1*,LIMin2,LIHui-juan2
1.DepartmentofEpidemiologyandHealthStatistics,SchoolofPreventiveMedicine,ChangzhiMedicalCollege,Changzhi046000,China2.DepartmentofCentralLaboratory,HepingHospitalAffiliatedtoChangzhiMedicalCollege,Changzhi046000,China
Objective To discuss clinical characteristics and prognosis of intestinal-type and diffuse-type gastric cancer.Methods A total of 392 patients with gastric cancer receiving operative treatment in the surgical ward of Heping Hospital Affiliated to Changzhi Medical College from January 1st2007 to December 30th2015 were selected.Among them,231 (58.9%) were intestinal type and 161 (41.1%) were diffuse type.The epidemiological questionnaire gastric cancer was established.The trained professionals according to unified standards collected the information of patients with gastric cancer.Their basic situation (gender,age,height,body mass,educational level,marital status,blood type,helicobacter pylori infection,family history of cancer);lifestyle and habits (smoking,drinking,eating speed,eating hot food,eating Chinese sauerkraut/pickles/preserved vegetables,eating fried foods);and pathological diagnosis and clinical staging were included in the collected information.The telephone follow-up of patients was made to inquire about survival by people having master degree or above in central lab of the hospital,and would be conducted until December 30th2015.Results There were no significant differences in gender,body mass index (BMI),educational level,marital status,blood type,helicobacter pylori infection and history of cancer between patients with intestinal-type cancer and patients with diffuse-type gastric cancer (P>0.05).There were significant differences in age between patients with intestinal-type cancer and patients with diffuse-type gastric cancer (P<0.05).There were significant differences in smoking and drinking between patients with intestinal-type cancer and patients with diffuse-type gastric cancer (P<0.05).There were no significant differences in eating speed,eating hot food,eating Chinese sauerkraut/pickles/preserved vegetables,eating fried foods between patients with intestinal-type cancer and patients with diffuse-type gastric cancer (P>0.05).There was no significant difference in T phase and M phase between patients with intestinal-type cancer and patients with diffuse-type gastric cancer (P>0.05).There was significant difference in N phase between patients with intestinal-type cancer and patients with diffuse-type gastric cancer (P<0.05).Three hundred and forty patients with gastric cancer had completed the followed up,the follow-up rate was 86.7%.By the end of follow-up,the survival rate of patients with intestinal-type gastric cancer was 66.5% (129/194),the median survival time was 24 months;and the survival rate was 52.7% (77/146) in patients with diffuse-type gastric cancer,and the median survival time was 18 months.The survival curves between patients with intestinal-type gastric cancer and patients with diffuse-type gastric cancer were significantly different (P<0.05).Conclusion The clinical manifestations and prognosis of Lauren classification were different.Lauren classification plays a decision-making role in the treatment and prevention of gastric cancer.
Stomach neoplasms;Lauren classification;Clinical characteristics;Prognosis
山西省基础研究计划项目(2015021185);国家自然科学基金资助项目(81302518);山西省长治医学院创新团队(CX201403)
R 735.2
A
10.3969/j.issn.1007-9572.2017.13.012
2016-12-08;
2017-03-24)
1.046000山西省长治市,长治医学院预防医学系流行病与卫生统计学教研室
2.046000山西省长治市,长治医学院附属和平医院中心实验室
*通信作者:曹文君,副教授;E-mail:wjcao16@hotmail.com
*Correspondingauthor:CAOWen-jun,Associateprofessor;E-mail:wjcao16@hotmail.com
