老年与中年急性冠脉综合征患者不同双联抗血小板方案疗效与出血风险比较
2017-04-20吕中华耿晓雯程庆强任艺虹
吕中华,耿晓雯,程庆强,高 洁,任艺虹
(解放军总医院心血管内科,北京 100853)
双联抗血小板治疗(dual antiplatelet therapy,DAPT)已经成为急性冠脉综合征(acute coronary syndrome,ACS)和经皮冠状动脉介入治疗(percutaneous coronary intervention,PCI)患者的标准治疗方案,目前主要为阿司匹林(aspirin)联合氯吡格雷(clopidogrel)或替格瑞洛(ticagrelor)[1,2]。替格瑞洛凭借其快速、可逆的抗血小板聚集作用,不受代谢酶影响[3-5],逐渐成为首选推荐药物。临床观察中发现即使规律应用抗血小板聚集药物,仍有部分患者再出现心血管事件及血栓弹力图(thromboelastography,TEG)检测血小板抑制率不达标情况。本研究旨在比较年龄<60岁阿司匹林+氯吡格雷组(<60C组)与年龄<60岁阿司匹林+替格瑞洛组(<60T组)、≥75岁阿司匹林+氯吡格雷组(≥75C组)与年龄≥75岁阿司匹林+替格瑞洛组(≥75T组)、<60T组与≥75T组、<60C组与≥75C组主要不良心血管事件(major adverse cardiovascular events,MACE)、出血事件发生情况,并分析相应的危险因素。
1 对象与方法
1.1 研究对象
连续收集2014年3月至2015年5月于解放军总医院心血管内科住院治疗的ACS、年龄<60岁及≥75岁、并进行TEG检查的416例患者的临床资料。根据年龄及应用P2Y12受体拮抗剂类型分为4组:(1)年龄<60岁阿司匹林+氯吡格雷组(<60C组,n=193),(2)年龄≥75岁阿司匹林+氯吡格雷组(≥75C组,n=58),(3)年龄<60岁阿司匹林+替格瑞洛组(<60T组,n=129),(4)年龄≥75岁阿司匹林+替格瑞洛组(≥75T组,n=36)。
1.2 研究方法
临床医师根据患者病情确定治疗药物。收集4组患者的临床资料,并随访,记录患者DAPT期间MACE情况、出血情况。患者因任何原因停止DAPT,终止随访。16人失访,失访率3.85%。
1.3 相关概念
(1)TEG指标:最大振幅(maximal amplitude,MA)反映血小板功能;检测过程中分别加入血小板激活剂花生四烯酸(arachidonic acid,AA)、二磷酸腺苷(adenosine diphosphate,ADP),可测得相应的MA,即:MA-AA、MA-ADP;血小板抑制率(%)分为AA诱发性血小板聚集(AA-induced platelet aggregation,AA-IPA)和ADP-IPA通路[6,7]。(2)MACE:再次血运重建、再次心肌梗死及全因死亡等。(3)出血事件按照出血学术研究协议(Bleeding Academic Research Consortium,BARC)标准定义;Ⅰ型:患者无需因此就医的非活动性出血;Ⅱ型:明显活动性出血,需要就医干预,未达到以下 Ⅲ~Ⅴ型标准;Ⅲ型,分为3个亚型:3a型,血红蛋白降低3~5 g/dl;3b型:血红蛋白降低≥5 g/dl,需要外科干预的出血;3c型:颅内出血,损害视力的眼内出血;Ⅳ型:冠状动脉旁路移植术(coronary artery bypass grafting,CABG)相关出血;Ⅴ型: 致死性出血。
1.4 统计学处理
数据应用SPSS17.0软件进行分析。计量资料以均数±标准差表示,组间比较采用方差分析(正态分布)或秩和检验(非正态分布)。计数资料以百分率表示,组间比较采用χ2检验。应用Cox回归分析MACE危险因素,logistic回归分析出血事件危险因素。以P<0.05为差异具有统计学意义。
2 结 果
2.1 各组基线资料比较
表1结果表明,<60C组与<60T组比较,各指标差异均无统计学意义(P>0.05);≥75C组与≥75T组比较,≥75C组年龄较大(P<0.001),其余指标差异均无统计学意义(P>0.05);与≥75T组比较,<60T组吸烟比例较高(P=0.001),高血压患病率较低(P=0.012),其余指标差异均无统计学意义(P>0.05);<60C组与≥75C组比较,<60C组男性比例、体质量指数(body mass index,BMI)、吸烟比例均较高(P<0.001),eGFR亦较高(P=0.001),其余指标差异均无统计学意义(P>0.05)。
2.2 TEG指标比较
表2结果表明,<60C组与<60T组比较,<60T组ADP途径抑制率较高(P<0.001),MA-ADP较低(P<0.001),其余各项指标差异均无统计学意义(P>0.05);≥75C组与≥75T组比较,≥75T组ADP途径抑制率较高(P<0.001),MA-ADP较低(P<0.001),其余各项指标差异均无统计学意义(P>0.05)。
表3结果表明,<60T组与≥75T组比较,各项指标差异均无统计学意义(P>0.05);<60C组与≥75C组比较,≥75C组ADP途径抑制率较低(P=0.011),MA-ADP较高(P=0.001),MA-AA较低(P=0.005)。
2.3 MACE及出血事件比较
4组患者MACE发生率差异无统计学意义(P>0.05;表4,表5)。应用Cox回归分析总体MACE危险因素:将心率、性别、年龄、BMI、吸烟、饮酒、血糖、MA值、AA-IPA、ADP-IPA、MA-ADP、MA-AA、eGFR、高血压、口服血管紧张素转换酶抑制剂/血管紧张素受体拮抗剂情况、口服β-阻滞剂情况、DAPT方案带入分析,得出MACE相关因素:血糖(B=0.111,RR=1.117,95%CI:1.014~1.231,P=0.025),eGFR(B=-0.023,RR=0.977,95%CI:0.961~0.993,P=0.005),心率(B=0.040,RR=1.041,95%CI:1.013~1.070,P=0.004)。
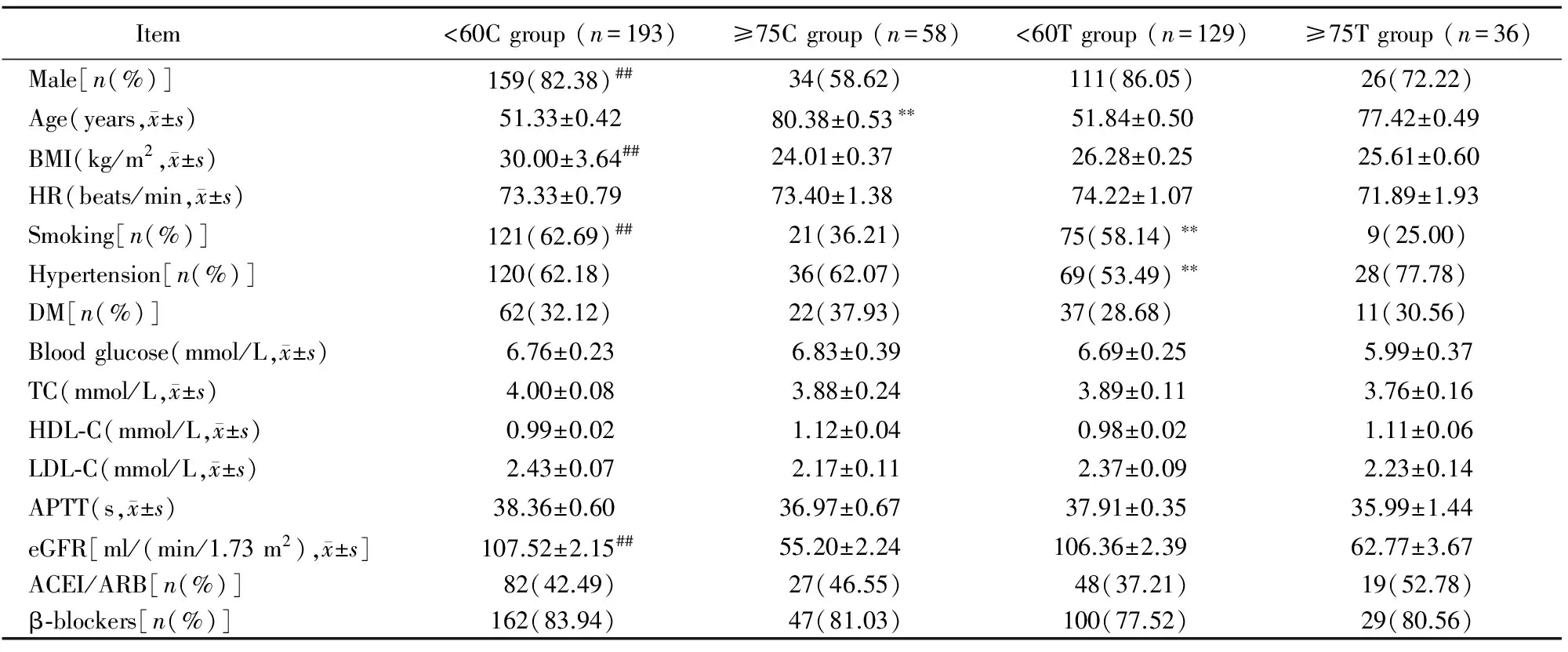
表1 患者基线资料比较
<60C group: <60 years old patients treated with aspirin combined clopidogrel; ≥75C group: ≥75 years old patients treated with aspirin combined clopidogrel; <60T group: <60 years old patients treated with aspirin combined ticagrelor; ≥75T group: ≥75 years old patients treated with aspirin combined ticagrelor; BMI: body mass index; HR: heart rate; DM: diabetes mellitus; TC: total cholesterol; HDL-C: high-density lipoprotein cholesterol; LDL-C: low-density lipoprotein cholesterol; APTT:activated partial thromboplastin time; eGFR: estimated glomerular filtration rate; ACEI: angiotensin-converting enzyme inhibitor; ARB: angiotensin receptor blocker. Compared with ≥75T group,**P<0.01; compared with ≥75C group,##P<0.01

表2 相同年龄段不同P2Y12拮抗剂TEG指标比较
<60C group: <60 years old patients treated with aspirin combined clopidogrel; ≥75C group: ≥75 years old patients treated with aspirin combined clopidogrel; <60T group: <60 years old patients treated with aspirin combined ticagrelor; ≥75T group: ≥75 years old patients treated with aspirin combined ticagrelor; MA: maximal amplitude; AA-IPA: inhibitory rate of arachidonic acid (AA)-induced platelet aggregation; ADP-IPA: inhibitory rate of adenosine diphosphate (ADP)-induced platelet aggregation; MA-ADP: ADP induced maximum amplitude; MA-AA: AA induced maximum amplitude

表3 相同P2Y12拮抗剂不同年龄段TEG指标比较
<60C group: <60 years old patients treated with aspirin combined clopidogrel; ≥75C group: ≥75 years old patients treated with aspirin combined clopidogrel; <60T group: <60 years old patients treated with aspirin combined ticagrelor; ≥75T group: ≥75 years old patients treated with aspirin combined ticagrelor; MA: maximal amplitude; AA-IPA: inhibitory rate of arachidonic acid (AA)-induced platelet aggregation; ADP-IPA: inhibitory rate of adenosine diphosphate (ADP)-induced platelet aggregation; MA-ADP: ADP induced maximum amplitude; MA-AA: AA induced maximum amplitude
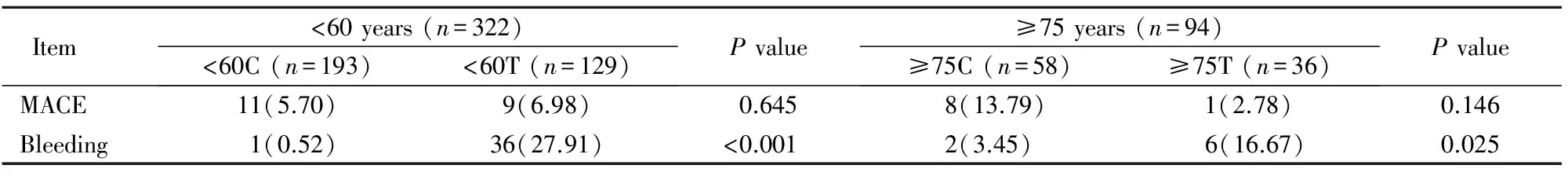
表4 相同年龄段不同P2Y12拮抗剂MACE、出血事件比较
<60C group: <60 years old patients treated with aspirin combined clopidogrel; ≥75C group: ≥75 years old patients treated with aspirin combined clopidogrel; <60T group: <60 years old patients treated with aspirin combined ticagrelor; ≥75T group: ≥75 years old patients treated with aspirin combined ticagrelor; MACE:major adverse cardiovascular events

表5 相同P2Y12拮抗剂不同年龄段MACE、出血事件比较
<60C group: <60 years old patients treated with aspirin combined clopidogrel; ≥75C group: ≥75 years old patients treated with aspirin combined clopidogrel; <60T group: <60 years old patients treated with aspirin combined ticagrelor; ≥75T group: ≥75 years old patients treated with aspirin combined ticagrelor; MACE: major adverse cardiovascular events
“替格瑞洛”患者出血事件发生率较“氯吡格雷”患者升高(P<0.05;表4)。<60C组出血1例(0.52%)表现为月经过多;≥75C组出血2例(3.45%):血尿1例、便血1例;<60T组出血36例(27.91%):淤斑20例、牙龈出血10例、鼻出血6例;≥75T组出血6例(16.67%):淤斑3例、牙龈出血1例、鼻出血1例、眼底出血1例。出血事件多为不需要临床干预的Ⅰ型出血。应用logistic回归分析出血事件危险因素:(1)总体:DAPT方案(B=3.527,OR=34.025,95%CI:9.560~121.101,P<0.001),性别(B=1.126,OR=3.085,95%CI:1.083~8.788,P=0.035);(2)分别对<60C与<60T,≥75C与≥75T进行logistic回归分析,均提示DAPT方案为出血事件危险因素。
3 讨 论
DAPT已经成为ACS、PCI患者抗血小板的标准方案,那么如何选择同为P2Y12受体拮抗剂的氯吡格雷与替格瑞洛,则成为临床医师面临的问题。氯吡格雷作为经典的P2Y12受体拮抗剂,仍是目前国内的一线用药,但存在着如下问题:为前体药物,需要经肝酶代谢后形成活性产物;代谢受ABCB1、CYP2C19基因的影响[8,9],在慢代谢患者体内活性代谢物的血药浓度降低,抗血小板作用降低。替格瑞洛为新型P2Y12受体拮抗剂,已成为首选推荐药物[10];半衰期短,不受代谢酶及ABCB1、CYP2C19基因的影响[3-5,11]。多项研究认为替格瑞洛能够更快速、强效地抑制血小板[12,13]。对氯吡格雷低反应性患者应用替格瑞洛可得到良好疗效[14]。有研究显示中国人群中替格瑞洛低反应性的比例明显低于氯吡格雷[15],且在中国人群中有良好的疗效及安全性[16,17],但也有研究显示其出血风险较氯吡格雷增高,且替格瑞洛有呼吸困难等不良反应,因不良反应停药的患者中约55.6%源于呼吸困难[18]。
TEG目前常用来检测血小板活性、判断DAPT的疗效。有研究认为TEG检测的ADP-IPA可作为预测支架内再狭窄的检验指标之一[7]。TEG检测发现替格瑞洛的ADP-IPA高于氯吡格雷、MA-ADP低于氯吡格雷,但MACE发生率无明显差异。这与替格瑞洛可降低MACE[1,2]不符,考虑与此研究为小样本、单中心有关。
综上所述,本研究显示替格瑞洛Ⅰ型出血发生率高于氯吡格雷,但未增加致命性出血风险与文献报道相符[3],出血发生率在<60T组与≥75T组无明显差异。
本研究属于单中心、小样本量研究,特别是≥75T组样本量偏小、口服氯吡格雷的两组患者仅有3例发生出血事件,因此需进一步行多中心、大样本量的随机对照研究以明确中国人群不同DAPT方案的优缺点,同时明确MACE及出血事件的相关因素,以利于临床医师在充分评估出血风险及血栓风险的基础上制定个体化的DAPT方案。
【参考文献】
[1] Roffi M, Patrono C, Collet JP,etal. 2015 ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-segment Elevation of the European Society of Cardiology (ESC)[J]. Eur Heart J, 2016, 37(3): 267-315. DOI: 10.1093/eurheartj/ehv320.
[2] Amsterdam EA, Wenger NK, Brindis RG,etal. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes:a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines[J]. Circulation, 2014, 130(25): e344-e426. DOI: 10.1161/CIR.0000000000000134.
[3] Wallentin L, Becker RC, Budaj A,etal. Ticagrelorversusclopidogrel in patients with acute coronary syndromes[J]. N Engl J Med, 2009, 361(11): 1045-1057. DOI: 10.1056/NEJMoa0904327.
[4] Steg PG, James S, Harrington RA,etal. Ticagrelorversusclopidogrel in patient with ST-elevation acute coronary syndromes intended for reperfusion with primary percutaneous coronary intervention: a Platelet Inhibition and Patient Outcomes(PLATO)trial subgroup analysis[J]. Circulation, 2010, 122(21): 2131-2141. DOI: 10.1161/CIRCULATIONAHA.109.927582.
[5] Lindholm D, Varenhorst C, Cannon CP,etal.Ticagrelorvsclopidogrel in paitents with non-ST-elevation acute coronary syndrome with or without revascularization: results from the PLATO trial[J]. Eur Heart J, 2014, 35(31): 2083-2093. DOI: 10.1093/eurheartj/ehu160.
[6] Bliden KP, DiChiara J, Tantry US,etal. Increased risk in patients with high platelet aggregation receiving chronic clopidogrel therapy undergoing percutaneous coronary intervention:is the current antiplatelet therapy adequate[J]? J Am Coll Cardiol, 2007, 49(6): 657-666.
[7] Fu Z, Dong W, Shen M,etal. Relationship between hyporespon-siveness to clopidogrel measured by thromboelastography and in stent restenosis in patients undergoing percutaneous coronary intervention[J]. Clin Biochem, 2014, 47(16-17): 197-202. DOI: 10.1016/j.clinbiochem.2014.08.009.
[8] Mega JL, Close SL, Wiviott SD,etal.Genetic variants in ABCB1,CYP2C19,and cardiovascular outcomes after treatment with clopidogrel and prasugrel in the TRITON-TIMI 38 trial:a pharmacogenetic analysis[J].Lancet, 2010, 376(9749): 1312-1319. DOI: 10.1016/S0140-6736(10)61273-1.
[9] Mega JL, Simon T, Collet JP,etal. Reduced-function CYP2C19 genotype and risk of adverse clinical outcomes among patients treated with clopidogrel predominantly for PCI: a meta-analysis[J]. JAMA, 2010, 304(16): 1821-1830. DOI: 10.1001/jama.2010.1543.
[10]中国医师协会急诊医师分会, 中华医学会心血管病学分会, 中华医学会检验医学分会. 急性冠脉综合征急诊快速诊疗指南[J]. 中华急诊医学杂志, 2016, 25(4): 391-404.
Emergency Medical Branch of Chinese Medical Doctor Association, Society of Cardiology of Chinese Medical Association, Laboratory Medicine Branch of Chinese Medical Association. Guidelines for rapid diagnosis and treatment of acute coronary syndrome[J]. Chin J Emerg Med, 2016, 25(4): 391-404.
[11]Wallentin L, James S, Storey RF,etal. Effect of CYP2C19 and ABCB1 single nucleotide polymorphisms on outcomes of treatment with ticagrelorversusclopidogrel for acute coronary syndromes: a genetic substudy of the PLATO trial[J]. Lancet, 2010, 376(9749): 1320-1328. DOI: 10.1016/S0140-6736(10)61274-3.
[12] Gurbel PA, Bliden KP, Butler K,etal. Randomized double-blind assessment of the ONSET and OFFSET of the antiplatelet effects of ticagrelorversusclopidogrel in patients with stable coronary artery disease: the ONSET/OFFSET study[J]. Circulation, 2009, 120(25): 2577-2585. DOI: 10.1161/CIRCULATIONAHA.109.912550.
[13] Chen Y, Dong W, Wan Z,etal. Ticagrelorversusclopidogrel in Chinese patients with acute coronary syndrome: a pharmacodynamic analysis[J]. Int J Cardiol, 2015, 201: 545-546. DOI: 10.1016/j.ijcard.2015.06.030.
[14] Li P, Yang Y, Chen T,etal. Ticagrelor overcomes high platelet reactivity in patients with acute myocardial infarction or coronary artery in-stent restenosis: a randomized controlled trial[J]. Sci Rep, 2015, 5: 13789. DOI: 10.1038/srep13789.
[15] 高 洁, 耿晓雯, 吕中华, 等. 血栓弹力图指导下的替格瑞洛与氯吡格雷在急性冠脉综合征患者中的疗效比较[J]. 中华老年多器官疾病杂志, 2016, 15(5): 353-357. DOI: 10.11915/j.issn.1671-5403.2016.05.084
Gao J, Geng XW, Lyu ZH,etal. Efficiency of ticagrelor and clopidogrel in treatment of acute coronary syndrome: a comparative study by thromboelastography[J]. Chin J Mult Organ Dis Elderly, 2016, 15(5): 353-357. DOI: 10.11915/j.issn.1671-5403.2016.05.084
[16] Li H, Butler K, Yang L,etal. Pharmacokinetics and tolerability of single and multiple doses of ticagrelor in healthy Chinese subjects: an open-label, sequential, two-cohort, single-centre study[J]. Clin Drug Invest, 2012, 32(2): 87-97. DOI: 10.2165/11595930-000000000-00000.
[17] 王贺阳, 苏 晞, 沈成兴, 等. 替格瑞洛在急性冠脉综合征患者中应用的安全性和有效性分析[J]. 中国循证心血管医学杂志, 2015, 8(4): 468-471.
Wang HY, Su X, Shen CX,etal. Effectiveness and safety of ticagrelor in acute coronary syndrome[J]. Chin J Evid Based Cardiovasc Med, 2015, 8(4): 468-471.
[18] Gaubert M, Laine M, Richard T,etal. Effect of ticagrelor-related dyspnea on compliance with therapy in acute coronary syndrome patients[J]. Int J Cardiol, 2014, 173(1): 120-121. DOI: 10.1016/j.ijcard.2014.02.028.