TURP术前非那雄胺应用时间对围术期出血的影响
2017-03-28谭书韬
谭书韬,吴 斌
TURP术前非那雄胺应用时间对围术期出血的影响
谭书韬,吴 斌*
目的 评价术前非那雄胺应用时间对经尿道前列腺切除术(Transurethral resection of prostate,TURP)术中及术后出血量的影响。方法 226例良性前列腺增生症(Benign prostatic hyperplasia,BPH)患者,术前服用1周非那雄胺5 mg的80例患者纳为1周组,服用2周的78例患者纳为2周组,未服用非那雄胺的68例患者纳为对照组,比较三组的手术时间、术中出血量、术中及术后冲洗液量、术后冲洗时间、出血指数及强度等。结果 226例TURP术均获得成功。与对照组比较,1周组和2周组的手术时间缩短、术中失血量、术中及术后冲洗液量减少,出血指数均显著降低,2周组术后冲洗时间、出血强度显著降低,差异有统计学意义(P<0.05)。与1周组比较,2周组手术时间缩短,术中失血量、术中冲洗液量减少,出血指数显著降低,差异有统计学意义(P<0.05)。结论 TURP术前2周服用非那雄胺可有效缩短TURP手术时间,减少术中及术后失血量。
良性前列腺增生;TURP;出血;非那雄胺
0 引言
经尿道前列腺切除术(Transurethral resection of prostate,TURP)是药物控制不佳的中重度良性前列腺增生(Benign prostatic hyperplasia,BPH)的标准治疗,是手术治疗的金标准[1]。术中及术后出血是TURP最常见的并发症之一,可能导致术中视野差、患者血流动力学不稳定、血凝块填塞膀胱,甚至需要二次手术治疗[2]。过去几十年,为了减少TURP术中及术后出血,研究者尝试应用过各种形式的促凝剂或硬化剂(如纤维蛋白粘合剂等),但这些方法的应用有一定的困难或局限性,有的甚至导致前列腺窝瘢痕的形成,导致术后排尿困难。由于5α-还原酶抑制剂非那雄胺对前列腺内血管生长因子的调节作用,有研究者已经开始注意其对于减少TURP围术期出血的治疗效果。目前已证明,应用非那雄胺可减少前列腺内血管内皮生长因子(VEGF,一种有效的血管生成生长因子)的表达以及微血管密度(MVD)的水平[3]。但对术前服用药物的时间尚缺乏深入研究。本文探讨了术前服用非那雄胺不同时间对TURP围术期出血的影响,现报道如下。
1 资料与方法
1.1 临床资料 选取2011年6月至2016年6月我院泌尿外科收治的行TURP患者226例,随机分为对照组68例。服用非那雄胺1周组(1周组)80例和服用非那雄胺2周组(2周组)78例,统计三组患者年龄、前列腺体积、国际前列腺症状评分(IPSS),残余尿量、最大尿流率、前列腺切除重量等一般资料。
1.2 纳入及排除标准 纳入标准:患者年龄60~80岁,前列腺体积40~80 mL,有BPH手术指征,患者有手术要求,除外手术禁忌及药物禁忌,服用阿司匹林者停用2周以上。
排除标准:前列腺体积>80 mL或<40 mL;伴神经源性膀胱;伴凝血功能异常;术前服用治疗BPH的植物药或性激素制剂;术后病理报告并发有前列腺癌者。
1.3 方法 1周组术前口服非那雄胺1周,1次/d,每次5 mg;2周组术前口服非那雄胺2周,1次/d,每次5 mg;对照组术前不应用非那雄胺。术前患者完善国际前列腺症状评分(IPSS),前列腺特异性抗原(PSA),前列腺超声,最大尿流率,尿流动力学检查。前列腺体积计算公式为π/6×长度(cm)×宽度(cm)×高度(cm)。采用腰-硬联合麻醉,手术均由同一组泌尿外科医生完成,冲洗液应用4%甘露醇,手术切除范围均达到前列腺外科包膜。
1.4 观察指标 记录每例手术时间,术中、术后冲洗液量及术后冲洗时间。术中出血量测定:冲洗液桶内加入肝素液,手术后充分搅匀冲洗液,取5 mL标本检测血红蛋白浓度,检测方法为氰化高铁血红蛋白比色法。出血量(mL)=冲洗液中血红蛋白浓度(g/L)×冲洗液量(L)/患者术前的血红蛋白浓度(g/L)×1 000[4]。根据每例患者的前列腺切除组织重量和手术时间,计算出血指数(平均切除每克前列腺组织的失血量)及出血强度(平均每分钟的出血量)。

2 结果
2.1 一般资料比较 三组患者的年龄、前列腺体积、IPSS评分、术前最大尿流率、手术切除前列腺重量比较差异均无统计学意义(P>0.05)。见表1。
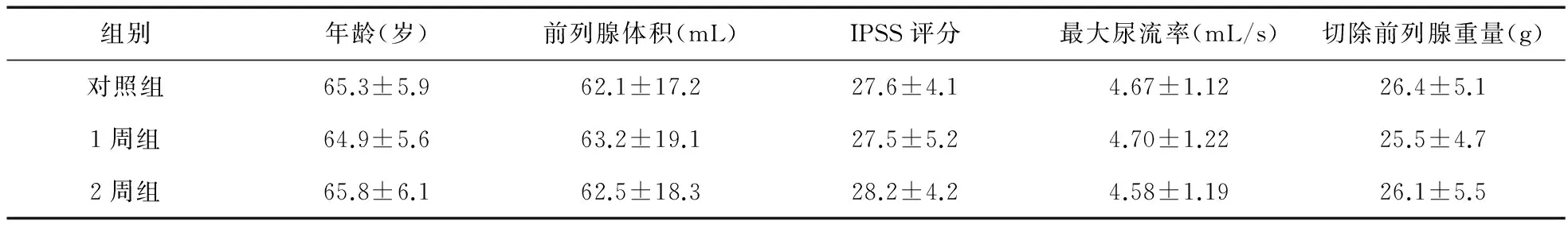
表1 三组一般资料比较
2.2 观察指标比较 与对照组比较,1周组手术时间、术中失血量、术中冲洗液量、术后冲洗时间、出血指数均明显降低,差异有统计学意义(P<0.05)。与对照组比较,2周组术后冲洗液量、出血强度显著降低(P<0.05)。2周组与1周组比较,手术时间、术中冲洗液量、术中失血量、出血指数差异有统计学意义(P<0.05)。见表2。
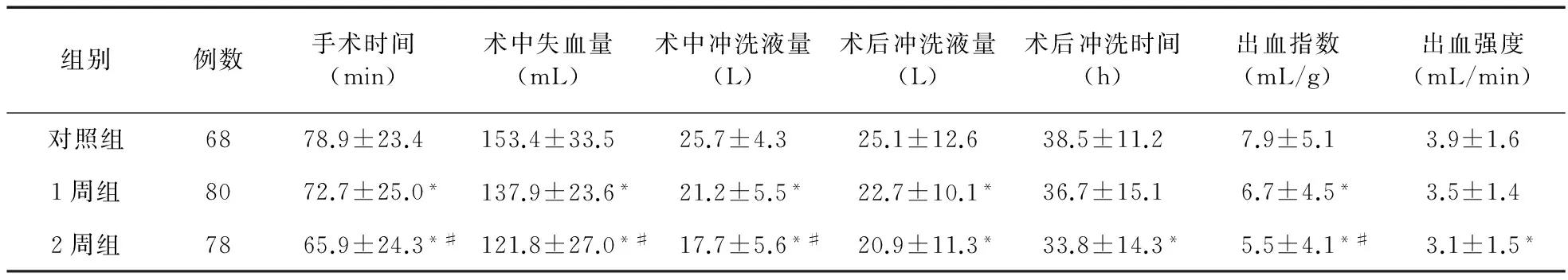
表2 三组临床指标比较
注:*与对照组比较,P<0.05;#与1周组比较,P<0.05
3 讨论
BPH是引起老年男性下尿路症状(LUTS)最主要的原因之一,60岁以上的老年男性中约有超过一半受其影响,BPH患者不但前列腺腺体增生,其血管生成也明显增加[5]。TURP是中重度BPH患者手术治疗的常用术式,其中最重要的并发症之一是术中及术后出血[6]。探索术前适当用药,从而有效控制TURP术中及术后出血,特别是对于那些手术风险较高的BPH患者,将提高TURP的安全性。非那雄胺是一种Ⅱ型5α-还原酶抑制剂,可以阻止睾酮变为活性更高的双氢睾酮(DHT)。有研究已经证明,前列腺内血管受DHT影响,其可以诱导前列腺上皮和基质细胞血管活性介质的表达,如VEGF[7]。有研究表明,BPH合并血尿患者的MVD显著高于未合并血尿的患者,说明MVD可以作为前列腺微血管增殖的指示之一,同时,其可能在TURP围术期出血中起重要作用[8]。VEGF表达增加及MVD被认为是导致BPH相关顽固性血尿的主要机制,亦是TURP术中及术后出血的主要原因之一[9]。作为5α-还原酶抑制剂,非那雄胺可降低前列腺内DHT的水平。Lekas等[10]研究表明,非那雄胺可以降低前列腺内MVD及VEGF水平。Donohue等[3]研究表明,应用非那雄胺2周后,前列腺标本的MVD显著降低。Jia等[11]在动物模型中使用增强磁共振成像评估前列腺的微循环,发现服用非那雄胺后前列腺血流灌注明显减少。 为了降低TURP术中及术后出血,可以术前应用5α-还原酶抑制剂减少前列腺微循环,减少BPH患者的MVD及TURP术中、术后出血[12]。Hagerty等[13]首先提出术前应用非那雄胺治疗对患者有益,能够显著减少输血、血块填塞膀胱和持续性肉眼血尿等情况。Özdal等[14]研究表明,TURP术前应用非那雄胺可以减少术中及术后出血,疗效肯定。Crea等[15]研究表明,术前应用非那雄胺可以减少术后血红蛋白的降低水平。Pastore等[16]研究表明,TURP术前应用5α-还原酶抑制剂度他雄胺,有利于抑制术后血红蛋白的下降。另有一项研究表明,TUPR术前应用度他雄胺,可以有效减少大前列腺(>50 mL)的术中失血[17]。本研究结果显示,与对照组比较,1周组的手术时间缩短,术中失血量减少,术中冲洗液量减少,术后冲洗时间缩短,出血指数降低,2周组的术后冲洗液量、出血强度也优于对照组。提示术前服用非那雄胺可减少TURP术中及术后的出血。
关于TURP术前治疗的最佳时间尚未达成共识。TURP术中及术后出血量与前列腺组织内血管生成及腺体内血管密度有关,而5α-还原酶抑制剂作用一定时间后才可对前列腺血管生成及密度产生影响[18]。目前,国内TURP术前应用非那雄胺的时间有1周或2周[19-20],而对于最优应用时间缺乏相应研究。国际上TURP术前应用5α-还原酶抑制剂的时间较国内延长。Khwaja等[21]研究表明,术前服用非那雄胺2周,可显著减少前列腺组织中的MVD。Donohue等[3]在TURP术前2周应用非那雄胺的患者中也观察到了这种血管生成抑制效果。而Aminsharifi等[22]认为,服用非那雄胺2周,可减少TURP术中出血,对于大体积前列腺的手术,可以适当延长服用非那雄胺时间。Pastore等[23]研究表明,另一种5α-还原酶抑制剂度他雄胺使用6周,可减少BPH手术的出血量。新近研究认为,对于一般TURP,术前应用非那雄胺2周,可有效减少术中及术后出血[21-22]。本研究结果也表明,术前应用非那雄胺2周,在手术时间、术中冲洗液量、术中失血量、出血指数方面均明显优于服用1周者,可以更好地降低围术期的出血。
综上所述,TURP术前应用非那雄胺,能有效减少术中及术后出血,术前应用2周非那雄胺更为适宜。未来仍需进一步的研究来探索TURP术前应用非那雄胺的最适宜时间。
[1] Oelke M,Bachmann A,Descazeaud A,et al.EAU guidelines on the treatment and follow-up of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction[J].Eur Urol,2013,64(1):118-140.
[2] Olvera-Posada D,Villeda-Sandoval C,Ramírez-Bonilla M,et al.Natural history of pyuria and microhematuria after prostate surgery[J].Actas Urol Esp,2013,37(10):625-629.
[3] Donohue JF,Hayne D,Karnik U,et al.Randomized,placebo-controlled trial showing that finasteride reduces prostatic vascularity rapidly within 2 weeks[J].BJU Int,2005,96(9):1319-1322.
[4] 郭麒麟,罗志刚.非那雄胺对减少经尿道前列腺电切术中术后出血的临床意义[J].现代医药卫生,2015,31(2):182-183,186.
[5] Gabuev A,Oelke M.Latest trends and recommendations on epidemiology,diagnosis,and treatment of benign prostatic hyperplasia (BPH)[J].Aktuelle Urol,2011,42(3):167-178.
[6] Shrivastava A,Gupta VB.Various treatment options for benign prostatic hyperplasia:a current update[J].J Midlife Health,2012,3(1):10-19.
[7] Sharif MR,Shaabani A,Mahmoudi H,et al.Association of the serum vascular endothelial growth factor levels with benign prostate hyperplasia and prostate malignancies[J].Nephrourol Mon,2014,6(3):e14778.
[8] Vasdev N,Kumar A,Veeratterapillay R,et al.Hematuria secondary to benign prostatic hyperplasia:retrospective analysis of 166 men identified in a single one stop hematuria clinic[J].Curr Urol,2013,6(3):146-149.
[9] Zhu YP,Dai B,Zhang HL,et al.Impact of preoperative 5α-reductase inhibitors on perioperative blood loss in patients with benign prostatic hyperplasia:a meta-analysis of randomized controlled trials[J].BMC Urol,2015,2(15):47.
[10]Lekas AG,Lazaris AC,Chrisofos M,et al.Finasteride effects on hypoxia and angiogenetic markers in benign prostatic hyperplasia[J].Urology,2006,68(2):436-441.
[11]Jia G,Heverhagen JT,Polzer H,et al.Dynamic contrast enhanced magnetic resonance imaging as a biological marker to noninvasively assess the effect of finasteride on prostatic suburethral microcirculation[J].J Urol,2006,176(5):2299-2304.
[12]Kavanagh LE,Jack GS,Lawrentschuk,N,et al.Prevention and management of TURP-related hemorrhage[J].Nat Rev Urol,2011,8(9):504-514.
[13]Hagerty JA,Ginsberg PC,Harmon JD,et al.Pretreatment with finasteride decreases perioperative bleeding associated with transurethral resection of the prostate[J].Urology,2000,55(5):684-689.
[14]Ozdal OL,Ozden C,Benli K,et al.Effect of short-term finasteride therapy on perioperative bleeding in patients who were candidates for transurethral resection of the prostate (TUR-P):a randomized controlled study[J].Prostate Cancer Prostatic Dis,2005,8(3):215-218.
[15]Crea G,Sanfilippo G,Anastasi G,et al.Pre-surgical finasteride therapy in patients treated endoscopically for benign prostatic hyperplasia[J].Urol Int,2005,74(1):51-53.
[16]Pastore AL,Mariani S,Barrese F,et al.Transurethral resection of prostate and the role of pharmacological treatment with dutasteride in decreasing surgical blood loss[J].J Endourol,2013,27(1):68-70.
[17]Busetto GM,Giovannone R,Antonini G,et al.Short-term pretreatment with a dual 5α-reductase inhibitor before bipolar transurethral resection of the prostate (B-TURP):evaluation of prostate vascularity and decreased surgical blood loss in large prostates[J].BJU Int,2015,116(1):117-123.
[18]Aboumarzouk OM,Aslam MZ,Wedderburn A,et al.Should Finasteride Be Routinely Given Preoperatively for TURP[J].ISRN Urol,2013,2013:458353.
[19]温海东,吕军,肖远松,等.比较围手术期应用度他雄胺和非那雄胺对经尿道前列腺电切术出血量的影响[J].现代泌尿外科杂志,2015,20(12):867-870.
[20]何二宝,李解方.非那雄胺剂量对减少经尿道前列腺电切术中出血的影响[J].现代泌尿外科杂志,2012,17(3):287-289.
[21]Khwaja MA,Nawaz G,Muhammad S,et al.The Effect of Two Weeks Preoperative Finasteride Therapy in Reducing Prostate Vascularity[J].J Coll Physicians Surg Pak,2016,26(3):213-215.
[22]Aminsharifi A,Salehi A,Noorafshan A,et al.Effect of preoperative finasteride on the volume or length density of prostate vessels,intraoperative,postoperative blood loss during and after monopolar transurethral resection of prostate:a dose escalation randomized clinical trial using stereolog methods[J].Urol J,2016,13(1):2562-2568.
[23]Pastore AL,Mariani S,Barrese F,et al.Transurethral resection of prostate and the role of pharmacological treatment with dutasteride in decreasing surgical blood loss[J].J Endourol,2013,27(1):68-70.
Effect of different courses of preoperative finasteride on perioperative bleeding in patients with
TURP TAN Shu-tao,WU Bin*
(Department of Urology,Shengjing Hospital of China Medical University,Shenyang 110004,China)
Objective To evaluate the effect of different courses of preoperative finasteride on the amount of perioperative bleeding during and after transurethral resection of prostate (TURP).Methods Totally 226 patients with benign prostatic hyperplasia (BPH) were scheduled for TURP,80 of them received 5 mg of finasteride daily for 1 week before surgery (group A),78 of them received finasteride for 2 weeks (group B),and the other 68 patients didn′t receive finasteride (control group).The operating time,intraoperative blood loss,intraoperative & postoperative irrigating fluid volume,postoperative irrigating time,bleeding index and intensity of the three groups were compared.Results The operation was successfully completed in 226 cases.Compared with control group,the operating time,intraoperative blood loss,intraoperative & postoperative irrigating fluid volume and bleeding index of group A and group B were significantly decreased,and the postoperative irrigating time and blood loss of group B were significantly decreased,the differences being significant (P<0.05).There were significant differences in the operating time,intraoperative blood loss,intraoperative irrigating fluid volume and bleeding index between group A and group B(P<0.05).Conclusion The use of finasteride two weeks before TURP can shorten the operating time and reduce perioperative and postoperative bleeding.
BPH;TURP;Bleeding;Finasteride
2016-09-18
中国医科大学附属盛京医院泌尿外科,沈阳 110004
*通信作者
10.14053/j.cnki.ppcr.201703012
